Abstract
Background
Few studies have looked at health system factors associated with laboratory test use.
Objective
To determine the association between health system factors and routine laboratory test use in medical inpatients.
Design
We conducted a retrospective cohort study on adult patients admitted to clinical teaching units over a 3-year period (January 2015 to December 2017) at three tertiary care hospitals in Calgary, Alberta.
Participants
Patients were assigned to a Case Mix Group+ (CMG+) category based on their clinical characteristics, and patients in the top 10 CMG+ groups were included in the cohort.
Exposures
The examined health system factors were (1) number of primary attending physicians seen by a patient, (2) number of attending medical teams seen by a patient, (3) structure of the medical team, and (4) day of the week.
Main Measures
The primary outcome was the total number of routine laboratory tests ordered on a patient during their admission. Statistical models were adjusted for age, sex, length of stay, Charlson comorbidity index, and CMG+ group.
Results
The final cohort consisting of 36,667 patient-days in hospital (mean (SD) age 62.5 (18.4) years) represented 5071 unique hospitalizations and 4324 unique patients. Routine laboratory test use was increased when patients saw multiple attending physicians; with an adjusted incidence rate ratio (IRR) of 1.46 (95% CI, 1.37–1.55) for two attending physicians, and 2.50 (95% CI, 2.23-2.79) for three or more attending physicians compared to a single attending physician. The number of routine laboratory tests was slightly lower on weekends (IRR 0.98, 95% CI, 0.96–0.99) and on teams without a senior resident as part of their team structure (IRR 0.89, 95% CI 0.830.96).
Conclusions
The associations observed in this study suggest that breaks in continuity of care, including increased frequency in patient transfer of care, may impact the utilization of routine laboratory tests.
Similar content being viewed by others
INTRODUCTION
Healthcare spending is rising, reaching an estimated 11.5% of the Canadian GDP in 2019.1,2,3 The misutilization of laboratory testing has seen increasing scrutiny in recent years.4 The estimated proportion of inappropriate laboratory tests is between 16 and 56% of the total tests ordered.5,6,7 Harms from laboratory test overutilization include increased patient discomfort, prolonged hospitalization, and downstream effects of additional investigations prompted by false-positive results.8,9 Increasing recognition of laboratory test overutilization as a systemic healthcare problem has prompted initiatives such as Choosing Wisely to provide recommendations on appropriate test use.10
The drivers of laboratory test overutilization are multifactorial. Several studies have identified patient-related factors (comorbidity level, diagnostic uncertainty) as well as practitioner-related factors (lack of awareness of appropriate test ordering practices), as predictors for inappropriate test use.11,12 There have been interventions designed to target these specific factors, including physician education, audit and feedback programs, and the use of computerized order entry systems.13,14,15 While these interventions have been somewhat effective, their overall success may be limited by a lack of consideration of systemic factors that contribute to laboratory test over-utilization.
Many health system factors have been studied in the context of broader health outcomes. For instance, frequent handover of patients between multiple physician teams may worsen patient outcomes and act as a source of medical errors.16,17 Similarly, patients admitted on weekends potentially have increased mortality compared to those admitted on weekdays, which may be attributable to reduced hospital staff availability on weekends.18,19,20 Whether these systemic factors also have an effect on the frequency of routine laboratory testing, however, is relatively unknown. Identifying any systemic factors contributing to the overutilization of laboratory tests could provide specific targets for cost-saving initiatives, including the implementation of system-related changes to existing practitioner-associated interventions.
The objective of this retrospective cohort study was to examine the association between health system factors and the utilization of routine laboratory tests in a cohort of medical inpatients admitted to clinical teaching units. The Clinical Teaching Unit, or CTU, is a hospital team structure which has widespread use in academic hospitals across Canada. The CTU structure integrates patient care with medical education by having medical learners (i.e. medical students and resident physicians) directly involved in patient care under the supervision of an internist acting as the most responsible practitioner (MRP).21 While some literature has found similar overall costs for resource utilization between teaching and non-teaching units, other studies have suggested slightly higher overall costs associated with teaching hospitals, as well as higher isolated costs for laboratory and radiographic testing within teaching units.22,23 Conducting our analysis within this setting provides useful insights into factors affecting laboratory test utilization with a degree of external validity within other academic structures similar to CTUs.
METHODS
Setting
We examined three tertiary care hospitals within Calgary, Alberta. Each hospital contained 2–3 CTU teams, each responsible for the care of approximately 20 inpatients. The CTU teams consisted of a general internist as the primary attending physician, along with 4–5 medical learners (medical students and resident physicians). All CTU teams had at least 2 junior postgraduate year (PGY)-1 residents and 2 medical students. Some CTU teams also had one senior resident in a leadership role. Senior residents are in the second or third year of their Internal Medicine residency and have the role of providing oversight on the clinical care provided by other learners on the team.24 In Calgary CTUs, senior residents do not engage in overnight on-call duties and, therefore, avoid off-duty post-call days to help ensure continuity of patient care.25 Only one of the three included hospitals had regularly scheduled day-time senior residents. The presence of senior residents does not alter the patient mix or admitting process. Specifically in Calgary, CTU teams are fully staffed during weekdays and staffed by only the attending physician and one learner on weekends. The vast majority of patients in the three hospitals are admitted directly from the emergency department, with few being transferred from other hospitals or rural sites.
Study Design and Participants/Cohort Creation
In this retrospective cohort study, we identified adults (age ≥18 years) admitted as patients to CTUs at three Calgary hospitals during a 3-year period (January 2015 to December 2017). Although there are small non-teaching internal medicine teams in two of these hospitals, data from those teams were excluded given differences in types of patients and model of care delivery. All three hospitals ordered laboratory tests through the same electronic medical record system, or EMR (Sunrise Clinical Manager; Allscripts, Chicago, IL.) There were no ongoing routine laboratory test–related quality improvement initiatives at any of the three sites during the timeframe of this study. A catalogue of all hospital patient-days recorded was sorted based on their Case Mix group (CMG+) classification, a research tool developed by the Canadian Institute of Health Information (CIHI) to facilitate the grouping of medical inpatients based on their clinical characteristics.26 The CMG+ categories assign patients to one of the various major clinical categories on the basis of their ICD-10 diagnostic code, as well as additional pertinent clinical data including in-hospital interventions such as intensive unit level of care. Only the ten most common CMG+ groups were included in our cohort for analysis to facilitate comparisons within similar groups of patients based on their clinical and resource utilization characteristics. The CMG+ group was used as a confounder in our statistical model to allow us to attribute changes in the outcome of laboratory test utilization to healthcare system factors within groups of similar patients.
Exposures/Variables
Four health system factors were examined: number of successive primary attending physicians seen by a patient throughout their CTU admission, number of medical attending teams involved throughout their CTU admission, whether the CTU team structure included a senior resident, and day of the week that tests were ordered (weekend versus weekday). These factors were included based on previous literature, showing their associations with other healthcare outcomes, including the rate of complications and length of hospitalization.27,28,29
The number of attending physicians refers to the number of individual physicians who assumed care of the patient during their CTU admission. MRP changeover at all three sites occurred every 7–14 days, on a fixed day of the week. Hence, depending on the day of admission and the handover schedule, patients with the same length of stay may have had different numbers of attending physicians. CTU learner teams changed every 28 days (on Mondays), with changeovers between attendings and learners typically being staggered to provide some continuity of care.
The number of medical attending teams refers to the number of times a patient was under the care of a different CTU team. While the regular MRP changeover does not typically result in the transfer of a patient’s care to a different CTU team, transfer between teams occasionally occurs for optimization of patient loads. A change in teams in this study refers to team-to-team transfers, as opposed to temporal changes that happen with changes in attending physician or learner teams.
There were two main types of team structure for CTUs: (1) teams with only junior-level residents and medical students; and (2) teams with a senior resident in addition to junior resident and student learners.
Outcomes
The primary outcome was the total number of routine laboratory tests ordered on a patient during their stay on CTU. Even though resident physicians can place test orders, in our method of data collection, all test orders are attributed to the most responsible physician for the patient at the time of order entry. This is done to create responsibility on the MRP to provide oversight on laboratory test ordering. We used local data on laboratory test utilization to identify laboratory tests that were top contributors to expenditure. Using that data, we defined the ‘routine’ panel of laboratory tests to include the following (cost per test in CAD in brackets): complete blood count ($7), electrolytes (sodium, potassium, chloride, and CO2) ($5), creatinine ($5), urea ($5), international normalized ratio ($7.5), partial thromboplastin time ($7.5), calcium ($5), magnesium ($5), phosphate ($5), and creatine kinase ($15).30 Creatine kinase as a single expensive test with few important indications for use was identified as an important part of the low-value routine test panel. This panel of repetitively ordered ten tests has been recognized as a low-value routine panel in our health zone and a target for improvement interventions.
Covariates/Controlled Variables
We adjusted for patient age, sex, length of CTU admission, Charlson comorbidity index, and CMG+ group in all of our models. We used the Charlson comorbidity index for approximation of patient comorbidity level, which has been validated in our population of medical inpatients.
31To adjust for clinical characteristics pertaining to the patient’s current hospitalization, we used their CMG+ category.
Data Sources/Measurement
We obtained data on the number and type of laboratory tests ordered, number of physicians and medical teams involved in the care of each patient, and day of the week that tests were ordered from our hospital EMR. Data on CTU team structure was obtained from the scheduling system provided by the Internal Medicine residency training program. We obtained patient variables including age, sex, most responsible diagnosis, Charlson comorbidity index, CMG+, and acute length of stay from the discharge abstract database. Length of stay on our CTUs only represents acute length of stay, with patients being transferred to a hospitalist service prior to being designated as ‘alternate level of care.’ The dataset included the identifier of the unique MD and the color of the CTU team associated with each patient-day. An attending MRP switch occurred with a change in MD identifier. A team switch occurred with a change in MD identifier and change in CTU team color.
Statistical Methods
We used mixed-effect Poisson regression to model the primary outcome of total routine laboratory tests ordered per patient on the CTU, adjusting for patient age, sex, Charlson comorbidity index, length of stay on the CTU, and CMG+ category. Healthcare system factors were examined as categorical variables: number of attending physicians (one, two, three, or more), number of attending teams (one, two, or more), CTU team structure (senior resident versus no senior resident), and day of the week (weekend versus weekday). Regression analyses were conducted at the patient level for the number of attending physicians, number of attending teams, and teams with or without senior resident; and at the hospitalization-day level for the day of the week. P values less than 0.05 were regarded as statistically significant. All statistical analyses were performed using Stata SE V.15.2 (Stata Corp, College Station, TX, USA).
Ethics Approval
Ethics approval was obtained from the Conjoint Health Research Ethics Board of the University of Calgary (CHREB 17-1215).
RESULTS
Cohort Characteristics
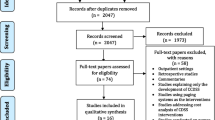
There were 111,207 hospital days at the three hospital sites between January 1, 2015, and December 31, 2017. Of these, the top 10 CMGs included a total of 36,667 hospital days (33%). These 36,667 hospital days represented 5071 unique hospitalizations and 4324 unique patients (Fig. 1). 27.6% of days in the cohort were on the weekend, and 92.5% of patients were seen by a single CTU team. CTU teams without a senior resident saw 68.4% of all patients. Cohort characteristics are described in Table 1.
Primary Outcome
Associations between examined health system factors and the use of the routine panel of laboratory tests are listed in Table 2. As compared to having one attending physician throughout a patient’s hospitalization, there were 1.46 times more tests ordered (95% CI: 1.37 to 1.55) when two attending physicians were involved. A two-and-a-half-fold increase (95% CI: 2.2–2.79) was found with three or more attending physicians. A total of 92.5% of patients stayed with the same CTU team throughout their admission. Patients who saw two or more teams did not have a significant difference in their test ordering rate. Having a senior resident as part of the team resulted in a slight increase in the number of tests ordered compared to teams that did not have a senior resident (IRR 1.12; 95% CI: 1.04 to 1.20). The number of laboratory tests ordered was slightly lower on weekends as compared to that on weekdays (IRR=0.98; 95% CI: 0.96 to 0.99).
DISCUSSION
In this retrospective cohort study, several health system factors were associated with the frequency of routine laboratory test use, after controlling for principal diagnosis, length of stay, patient age, sex, and comorbidity. Notably, having multiple attending physicians involved in the care of a patient resulted in a substantial increase in the number of routine laboratory tests ordered for that patient during their hospitalization. Weekdays and medical teams containing senior trainees were other factors associated with increased routine laboratory test utilization.
We found an approximate 50% increase in the number of routine tests ordered when two physicians were involved in the care of a patient, and 2.5 times increase for 3 or more physicians. This association was present after adjusting for patient comorbidity, principal diagnosis, and length of stay, decreasing the likelihood of confounding by patient complexity. In total, 92.5% of patients remained with a single CTU team throughout their admission. When a change in teams did occur, the number of attending teams was not significantly associated with the number of routine tests ordered. It is possible that patients who are transferred between teams are more stable, or have more clarity in clinical progression, and hence, we do not see the increase in the use of routine laboratory tests with this transition. It may also suggest that it is primarily the change in attending MRP that drives the increased use of routine tests, independent of the transfer between teams.
The increased number of routine tests ordered with more attending physicians is likely attributable to repetitive test ordering during the transfer of care between attending physicians. Repetitive or redundant laboratory test ordering has been observed in patient transfers of care within other healthcare settings, including inter-facility transfer (i.e. from the emergency department of a community site to that of a tertiary care center).32,33 However, to our knowledge, the frequency of transfer of care for admitted inpatients has not been studied in regards to laboratory test utilization. Prior research has also shown that frequent handover of patients can adversely affect a variety of patient outcomes, including the rate of medical errors, length of stay, and poorer patient outcomes..27,28 Further research is needed to confirm our findings and elucidate whether there are reasons other than the transfer of care that result in increased laboratory test use with the involvement of multiple physicians.
It has previously been found that senior medical trainees order more laboratory tests than junior trainees overall, but junior trainees have a higher frequency of ordering inappropriate or unnecessary tests.11 We found that CTU teams led by a senior resident ordered slightly more routine tests than teams fielded by only junior-level trainees, although our study does not allow us to comment on the appropriateness of utilization. Further research could explore the test-ordering tendencies of senior and junior trainees when they are considered in a team-wide setting. Weekend days had slightly fewer routine tests ordered compared to weekdays. Prior studies have reported an increase in adverse outcomes for patients on weekend admissions compared to weekday admissions, although it is unclear whether laboratory test utilization has a role in determining this association.29 Within the CTU team structure, weekends differ from weekdays in having a reduced number of residents and medical students present. This may again have an impact on patient continuity of care as medical learners who would typically be caring for a particular patient are often absent on weekends. As such, it is unclear from our analysis whether the lower number of tests ordered on weekends represents an appropriate or inappropriate reduction due to missed tests. Future studies should examine the link between the intensity of utilization of routine laboratory tests and patient-relevant outcomes like re-admissions, mortality, and length of stay.
There are several limitations of our study. Firstly, we were not able to differentiate between appropriate and inappropriate laboratory test use. Similarly, owing to limitations in the data set, we were unable to control for whether the test results were normal or abnormal, or the degree of specialist involvement in care. This information could have helped understand the ordering pattern better. Although factors known to affect test ordering tendencies were adjusted for in our statistical analysis, as with any observational study, we are limited by unmeasured confounders. Our study was limited to a single city, which operates using a similar format for inpatient CTUs. While the CTU is a widely used structure for the care of medical inpatients across Canada, differences between hospitals in Calgary and other cities (e.g. use of EMR, patient population) may affect the applicability of our findings to other centers. Finally, patients outside of the 10 most common CMG+ categories were excluded from our final cohort. While this enabled us to make comparisons within similar patient groups, it does limit the generalizability of our findings.
In conclusion, in this retrospective cohort study conducted on medical inpatients at three tertiary hospitals, the number of attending physicians seen by a patient, inpatient medical team structure, and day of the week were significantly associated with the number of routine laboratory tests ordered. The strongest association was observed with a higher number of attending physicians resulting in more routine tests being ordered. Overall, our findings highlight patient continuity of care as a potential systemic factor warranting further investigation for cost reduction through targeting laboratory test overutilization.
References
Watson R. Health spending rising faster than GDP in most rich countries. BMJ. 2006;333(7558):60. doi:https://doi.org/10.1136/bmj.333.7558.60-a
2. Health spending | CIHI. Cihi.ca. https://www.cihi.ca/en/health-spending. Published 2021. Accessed June 9, 2021
Sorenson C, Drummond M, Bhuiyan Khan B. Medical technology as a key driver of rising health expenditure: disentangling the relationship. Clinicoecon Outcomes Res. 2013;5:223-34 doi:https://doi.org/10.2147/CEOR.S39634
Sarkar MK, Botz CM, Laposata M. An assessment of overutilization and underutilization of laboratory tests by expert physicians in the evaluation of patients for bleeding and thrombotic disorders in clinical context and in real time. Diagnosis (Berl). 2017;4(1):21-26. doi:https://doi.org/10.1515/dx-2016-0042
Bindraban RS, Ten Berg MJ, Naaktgeboren CA, Kramer MHH, Van Solinge WW, Nanayakkara PWB. Reducing Test Utilization in Hospital Settings: A Narrative Review. Ann Lab Med. Sep 2018;38(5):402-412. doi:https://doi.org/10.3343/alm.2018.38.5.402
Zhi M, Ding EL, Theisen-Toupal J, Whelan J, Arnaout R. The landscape of inappropriate laboratory testing: a 15-year meta-analysis. PLoS One. 2013;8(11):e78962. doi:https://doi.org/10.1371/journal.pone.0078962
Hanson C Plumhoff E. Test utilization and the clinical laboratory. Mayo Med Lab Commun. 2012:1-4.
Naugler C, Wyonch R. What the Doctor Ordered: Improving the Use and Value of Laboratory Testing. 2019. Commentary.
Eaton KP, Levy K, Soong C, et al. Evidence-Based Guidelines to Eliminate Repetitive Laboratory Testing. JAMA Intern Med. 2017;177(12):1833-1839. doi:https://doi.org/10.1001/jamainternmed.2017.5152
Our Mission. Choosing Wisely. https://www.choosingwisely.org/our-mission/. Published 2020. Accessed November 26, 2020
Miyakis S, Karamanof G, Liontos M, Mountokalakis TD. Factors contributing to inappropriate ordering of tests in an academic medical department and the effect of an educational feedback strategy. Postgrad Med J. Dec 2006;82(974):823-9. doi:https://doi.org/10.1136/pgmj.2006.049551
Vrijsen BEL, Naaktgeboren CA, Vos LM, van Solinge WW, Kaasjager HAH, Ten Berg MJ. Inappropriate laboratory testing in internal medicine inpatients: Prevalence, causes and interventions. Ann Med Surg (Lond). Mar 2020;51:48-53. doi:https://doi.org/10.1016/j.amsu.2020.02.002
Rudolf JW, Dighe AS, Coley CM, et al. Analysis of Daily Laboratory Orders at a Large Urban Academic Center: A Multifaceted Approach to Changing Test Ordering Patterns. Am J Clin Pathol. Aug 2017;148(2):128-135. doi:https://doi.org/10.1093/ajcp/aqx054
Jalbert R, Gob A, Chin-Yee I. Decreasing daily blood work in hospitals: What works and what doesn't. Int J Lab Hematol. May 2019;41 Suppl 1:151-161. doi:https://doi.org/10.1111/ijlh.13015
Almeqdadi M, Nair HK, Hill J, Sanchez-Cruz J, Nader C, Jaber BL. A quality improvement project to reduce overutilization of blood tests in a teaching hospital. J Community Hosp Intern Med Perspect. 2019;9(3):189-194. doi:https://doi.org/10.1080/20009666.2019.1601979
Breuer RK, Taicher B, Turner DA, Cheifetz IM, Rehder KJ. Standardizing postoperative PICU handovers improves handover metrics and patient outcomes. Pediatr Crit Care Med. Mar 2015;16(3):256-63. doi:https://doi.org/10.1097/PCC.0000000000000343
Raduma-Tomàs MA, Flin R, Yule S, Williams D. Doctors' handovers in hospitals: a literature review. BMJ Qual Saf. Feb 2011;20(2):128-33. doi:https://doi.org/10.1136/bmjqs.2009.034389
Mathew A, Fyyaz SA, Carter PR, Potluri R. The enigma of the weekend effect. J Thorac Dis. Jan 2018;10(1):102-105. doi:https://doi.org/10.21037/jtd.2017.12.115
Dorn SD, Shah ND, Berg BP, Naessens JM. Effect of weekend hospital admission on gastrointestinal hemorrhage outcomes. Dig Dis Sci. 2010;55(6):1658-66. doi:https://doi.org/10.1007/s10620-009-0914-1
Saposnik G, Baibergenova A, Bayer N, Hachinski V. Weekends: a dangerous time for having a stroke? Stroke. Apr 2007;38(4):1211-5. doi:https://doi.org/10.1161/01.STR.0000259622.78616.ea
Tang B, Sandarage R, Dutkiewicz K, et al. Clinical teaching unit design: a realist systematic review protocol of evidence-based practices for clinical education and health service delivery. BMJ Open. 2020;10(2):e034370. doi:https://doi.org/10.1136/bmjopen-2019-034370
Khaliq AA, Huang CY, Ganti AK, Invie K, Smego RA. Comparison of resource utilization and clinical outcomes between teaching and nonteaching medical services. J Hosp Med. May 2007;2(3):150-7. doi:https://doi.org/10.1002/jhm.174
Silber JH, Rosenbaum PR, Niknam BA, et al. Comparing Outcomes and Costs of Medical Patients Treated at Major Teaching and Non-teaching Hospitals: A National Matched Analysis. J Gen Intern Med. 2020;35(3):743-752. doi:https://doi.org/10.1007/s11606-019-05449-x
Huda N, Faden L, Goldszmidt M. Entrustment of the on-call senior medical resident role: implications for patient safety and collective care. BMC Med Educ. 2017;17(1):121. doi:https://doi.org/10.1186/s12909-017-0959-3
Cheung JY, Mueller D, Blum M, et al. An observational pre-post study of re-structuring Medicine inpatient teaching service: Improved continuity of care within constraint of 2011 duty hours. Healthc (Amst). 2015;3(3):129-134. doi:https://doi.org/10.1016/j.hjdsi.2015.05.001
CMG+ | CIHI. Cihi.ca. https://www.cihi.ca/en/cmg. Published 2021. Accessed January 2021.
Bollschweiler E, Krings A, Fuchs KH, et al. Alternative shift models and the quality of patient care. An empirical study in surgical intensive care units. Langenbecks Arch Surg. Mar 2001;386(2):104-9. doi:https://doi.org/10.1007/s004230000188
Horwitz LI, Krumholz HM, Green ML, Huot SJ. Transfers of patient care between house staff on internal medicine wards: a national survey. Arch Intern Med. Jun 2006;166(11):1173-7. doi:https://doi.org/10.1001/archinte.166.11.1173
Pauls LA, Johnson-Paben R, McGready J, Murphy JD, Pronovost PJ, Wu CL. The Weekend Effect in Hospitalized Patients: A Meta-Analysis. J Hosp Med. 2017;12(9):760-766. doi:https://doi.org/10.12788/jhm.2815
Ambasta A, Pancic S, Wong BM, Lee T, McCaughey D, Ma IWY. Expert Recommendations on Frequency of Utilization of Common Laboratory Tests in Medical Inpatients: a Canadian Consensus Study. J Gen Intern Med. 2019;34(12):2786-2795. doi:https://doi.org/10.1007/s11606-019-05196-z
Frenkel WJ, Jongerius EJ, Mandjes-van Uitert MJ, van Munster BC, de Rooij SE. Validation of the Charlson Comorbidity Index in acutely hospitalized elderly adults: a prospective cohort study. J Am Geriatr Soc. 2014;62(2):342-346. doi:https://doi.org/10.1111/jgs.12635
Bertrand J, Fehlmann C, Grosgurin O, Sarasin F, Kherad O. Inappropriateness of Repeated Laboratory and Radiological Tests for Transferred Emergency Department Patients. J Clin Med. 2019;8(9) doi:https://doi.org/10.3390/jcm8091342
Rogg JG, Rubin JT, Hansen P, Liu SW. The frequency and cost of redundant laboratory testing for transferred ED patients. Am J Emerg Med. Jul 2013;31(7):1121-3. doi:https://doi.org/10.1016/j.ajem.2013.03.037
Acknowledgements
We acknowledge the Department of Medicine at the University of Calgary and Alberta Health Services for funding this project. The funding bodies played no role in the design of the study, collection, analysis, and interpretation of the data, and the decision to approve the publication of the finished manuscript.
Data Availability
The dataset analyzed in this study is available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tam, K., Williamson, T., Ma, I.W.Y. et al. Association Between Health System Factors and Utilization of Routine Laboratory Tests in Clinical Teaching Units: a Cohort Analysis . J GEN INTERN MED 37, 1444–1449 (2022). https://doi.org/10.1007/s11606-021-07063-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-021-07063-2