Abstract
Background
Patients with mental health conditions (MHCs) experience poor anticoagulation control when using warfarin, but we have limited knowledge of the association between specific mental illness and warfarin treatment outcomes.
Objective
To examine the relationship between the severity of MHCs and outcomes of anticoagulation therapy.
Design
Retrospective cohort analysis.
Participants
We studied 103,897 patients on warfarin for 6 or more months cared for by the Veterans Health Administration during fiscal years 2007–2008. We identified 28,216 patients with MHCs using ICD-9 codes: anxiety disorders, bipolar disorder, depression, post-traumatic stress disorder, schizophrenia, and other psychotic disorders.
Main Measures
Outcomes included anticoagulation control, as measured by percent time in the therapeutic range (TTR), as well as major hemorrhage. Predictors included different categories of MHC, Global Assessment of Functioning (GAF) scores, and psychiatric hospitalizations.
Key Results
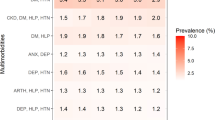
Patients with bipolar disorder, depression, and other psychotic disorders experienced TTR decreases of 2.63 %, 2.26 %, and 2.92 %, respectively (p < 0.001), after controlling for covariates. Patients with psychotic disorders other than schizophrenia experienced increased hemorrhage after controlling for covariates [hazard ratio (HR) 1.24, p = 0.03]. Having any MHC was associated with a slightly increased hazard for hemorrhage (HR 1.19, p < 0.001) after controlling for covariates.
Conclusion
Patients with specific MHCs (bipolar disorder, depression, and other psychotic disorders) experienced slightly worse anticoagulation control. Patients with any MHC had a slightly increased hazard for major hemorrhage, but the magnitude of this difference is unlikely to be clinically significant. Overall, our results suggest that appropriately selected patients with MHCs can safely receive therapy with warfarin.
Similar content being viewed by others
References
Kessler RC, Chiu WT, Demler O, Walter EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617–27.
Chander G, Himelhoch S, Moore RD. Substance abuse and psychiatric disorders in HIV-positive patients: epidemiology and impact on antiretroviral therapy. Drugs. 2006;66(6):769–89.
Daumit GL, Pronovost PJ, Anthony CB, Guallar E, Steinwachs DM, Ford DE. Adverse events during medical and surgical hospitalizations for persons with schizophrenia. Arch Gen Psychiatry. 2006;63(3):267–72.
Desai MM, Rosenheck RA, Druss BG, Perlin JB. Mental disorders and quality of diabetes care in the Veterans Health Administration. Am J Psychiatry. 2002;159(9):1584–90.
Druss BG, Bradford DW, Rosenheck RA, Radford MJ, Krumholz HM. Mental disorders and use of cardiovascular procedures after myocardial infarction. JAMA. 2000;283(4):506–12.
Frayne SM, Halanych JH, Miller DR, Wang F, Lin H, Pogach L, Sharkansky EJ, Keane TM, Skinner KM, Rosen CS, Berlowitz DR. Disparities in diabetes care: impact of mental illness. Arch Intern Med. 2005;165(22):2631–8.
Leucht S, Burkard T, Henderson J, Maj M, Sartorius N. Physical illness and schizophrenia: a review of the literature. Acta Psychiatr Scand. 2007;116(5):317–33.
Druss BG, von Esenwein SA. Improving general medical care for persons with mental and addictive disorders: systematic review. Gen Hosp Psychiatry. 2006;28(2):145–53.
Lawrence D, Kisely S. Inequalities in healthcare provisions for people with severe mental illness. J Psychopharmacol. 2010;24(4):61–8.
Thornicroft G, Rose D, Kassam A. Discrimination in health care against people with mental illness. Int Rev Psychiatry. 2007;19(2):113–22.
Ansell J, Hirsh J, Hylek E, Jacobson A, Crowther M, Palareti G. Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2008;133(6 Suppl):160S–98.
Connolly SJ, Pogue J, Eikelboom J, Flaker G, Commerford P, Franzosi MG, Healey JS, Yusuf S. Benefit of oral anticoagulant over antiplatelet therapy in atrial fibrillation depends on the quality of international normalized ratio control achieved by centers and countries as measured by time in therapeutic range. Circulation. 2008;118(20):2029–37.
Gallagher AM, Setakis E, Plumb JM, Clemens A, van Staa TP. Risks of stroke and mortality associated with suboptimal anticoagulation in atrial fibrillation patients. Thromb Haemost. 2011;106(5):968–77.
Jones M, McEwan P, Morgan CL, Peters JR, Goodfellow J, Currie CJ. Evaluation of the pattern of treatment, level of anticoagulation control, and outcome of treatment with warfarin in patients with non-valvular atrial fibrillation: a record linkage study in a large British population. Heart. 2005;91(4):472–7.
White HD, Gruber M, Feyzi J, Kaatz S, Tse HF, Husted S, Albers GW. Comparison of outcomes among patients randomized to warfarin therapy according to anticoagulant control: results from SPORTIF III and V. Arch Intern Med. 2007;167(3):239–45.
Walker GA, Heidenreich PA, Phibbs CS, Go AS, Chiu VY, Schmitt SK, Ananth L, Frayne SM. Mental illness and warfarin use in atrial fibrillation. Am J Manag Care. 2011;17(9):617–24.
Rose AJ, Hylek EM, Ozonoff A, Ash AS, Reisman JI, Berlowitz DR. Patient characteristics associated with oral anticoagulation control: results of the Veterans AffaiRs Study to Improve Anticoagulation (VARIA). J Thromb Haemost. 2010;8(10):2182–91.
Schauer DP, Moomaw CJ, Wess M, Webb T, Eckman MH. Psychosocial risk factors for adverse outcomes in patients with nonvalvular atrial fibrillation receiving warfarin. J Gen Intern Med. 2005;20(12):1114–9.
Rose AJ, Hylek EM, Ozonoff A, Ash AS, Reisman JI, Berlowitz DR. Risk-adjusted percent time in therapeutic range as a quality indicator for outpatient oral anticoagulation: results of the Veterans Affairs Study to Improve Anticoagulation (VARIA). Circ Cardiovasc Qual Outcomes. 2011;4(1):22–9.
Perlin J, Kazis LE, Skinner KM, Ren XS, Lee A, Rogers W, Spiro A III, Selim A, Miller D. (Veterans Health Administration: Office of Quality and Performance). 1999 Large Health Survey of Veteran Enrollees: Executive Report. 2000.
American Psychiatric Association. “Multiaxial Assessment.” DSM-IV-TR Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Arlington: American Psychiatric Association; 2000.
Greenberg GA, Rosenheck RA. Special section on the GAF: using the GAF as a national mental health outcome measure in the Department of Veterans Affairs. Psychiatr Serv. 2005;56(4):420–6.
Greenberg GA, Rosenheck RA. Use of nationwide outcomes monitoring data to compare clinical outcomes in specialized mental health programs and general psychiatric clinics in the Veterans Health Administration. Psychiatr Q. 2006;77(2):151–72.
Moos RH, Nichol AC, Moos BS. Global assessment of functioning rating and the allocation and outcomes of mental health services. Psychiatr Serv. 2002;53(6):730–7.
Moos RH, Lucie M, Moos BS. Global assessment of functioning (GAF) ratings: determinants and role as predictors of one-year treatment outcomes. J Clin Pyschol. 2000;56(4):449–61.
Aas IHM. Guidelines for rating Global Assessment of Functioning (GAF). Ann Gen Psychiatry. 2011;10(2):1–11.
Aas IHM. Global Assessment of Functioning (GAF): properties and frontier of current knowledge. Ann Gen Psychiatry. 2010;9(20):1–11.
Lip GY, Frison L, Halperin JL, Lane DA. Comparative validation of a novel risk score for predicting bleeding risk in anticoagulated patients with atrial fibrillation: the HAS-BLED (Hypertension, Abnormal Renal/Liver Function, Stroke, Bleeding History or Predisposition, Labile INR, Elderly, Drugs/Alcohol Concomitantly) score. J Am Coll Cardiol. 2011;57(2):173–80.
Rosendaal FR, Cannegieter SC, van Der Meer FJ, Briët E. A method to determine the optimal intensity of oral anticoagulant therapy. Thromb Haemost. 1993;69(3):236–9.
Jasuja GK, Reisman JI, Miller DR, Berlowitz DR, Hylek EM, Ash AS, Ozonoff A, Zhao S, Rose AJ. Identifying major hemorrhage with automated data: results of the Veterans Affairs Study to Improve Anticoagulation (VARIA). Thromb Res. 2013;131(1):31–6.
Frayne SM, Miller DR, Sharkansky EJ, Jackson VW, Wang F, Halanych JH, Berlowitz DR, Kader B, Rosen CS, Keane TM. Using administrative data to identify mental illness: what approach is best? Am J Med Qual. 2010;25(1):42–50.
Acknowledgments
This project was supported by VA grant VA-HSRD-IIR-10-374. The opinions expressed here are those of the authors and do not necessarily represent the official views or policies of the US Department of Veterans Affairs.
Conflict of Interest
Dr. Hylek has served on advisory boards for Bayer, Boehringer-Ingelheim, Bristol Myers Squibb, Daiichi Sankyo, Johnson and Johnson, Merck, and Pfizer. None of the other authors report any potential conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 365 kb)
Rights and permissions
About this article
Cite this article
Paradise, H.T., Berlowitz, D.R., Ozonoff, A. et al. Outcomes of Anticoagulation Therapy in Patients with Mental Health Conditions. J GEN INTERN MED 29, 855–861 (2014). https://doi.org/10.1007/s11606-014-2784-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-014-2784-2