Abstract
Purpose
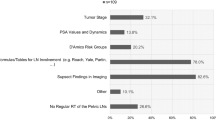
Radiotherapy (RT) has an established role in the treatment of prostate cancer patients. Despite the large number of patients treated with RT, some issues about optimal techniques, doses, volumes, timing, and association with androgen deprivation are still subject of debate. The aim of this survey was to determine the patterns of choice of Italian radiation oncologists in two different clinical cases of prostate cancer patients treated with radical RT.
Study design
During the 2010 Italian Association of Radiation Oncology (AIRO) National congress, four different clinical cases were presented to attending radiation oncologists. Two of them were prostate cancer cases that could be treated by RT +/− hormonal therapy (HT), different for T stage of primary tumour according to TNM, preoperative diagnostic procedures for staging, initial prostate specific antigen (iPSA), and Gleason Score sum of biopsy. For each clinical case, radiation oncologists were asked to: (a) give indication to pretreatment procedures for staging; (b) give indication to treatment; (c) define specifically, where indicated, total dose, type of fractionation, volumes of treatment, type of technique, type of image-guided setup control; (d) indicate if HT should be prescribed; (e) define criteria that particularly influenced prescription. A descriptive statistical analysis was performed.
Results
Three hundred questionnaires were given to radiation oncologists attending the congress, 128 questionnaires were completed and considered for this analysis (41%). Some important differences were shown in prescribing and delivering RT, particularly with regards to treatment volumes and fractionation.
Conclusions
Despite the results of clinical trials, several differences still exist among Italian radiation oncologists in the treatment of prostate cancer patients. These patients probably deserve a more uniform approach, based on upto-date, detailed, and evidence-based recommendations.
Riassunto
Obiettivo
La radioterapia (RT) ricopre un ruolo ben stabilito nel trattamento dei pazienti con tumore della prostata. Nonostante il grande numero di pazienti trattati con RT, alcune controversie circa la tecnica ottimale di trattamento, le dosi, i volumi, il timing rispetto alla chirurgia e l’associazione con la terapia ormonale sono ancora oggetto di dibattito. Lo scopo di questa indagine è stato di determinare la modalità di scelta di trattamento degli oncologi radioterapisti italiani in 2 diversi casi clinici di pazienti affetti da tumore prostatico trattati con RT a scopo radicale.
Disegno di studio
Durante il Congresso Nazionale dell’Associazione Italiana di Radioterapia Oncologica (AIRO) del 2010, 4 casi clinici sono stati proposti agli oncologi radioterapisti presenti. Due di questi casi clinici si presentavano adeguati alla RT a scopo radicale +/− ormonoterapia (OT), ed erano diversi per stadio clinico, procedure diagnostiche di staging pre-trattamento, antigene specifico della prostata (PSA) iniziale, Gleason Score bioptico. Per ogni caso clinico si chiedeva di (a) dare indicazione a nuove procedure di staging pre-trattamento; (b) dare indicazione al trattamento; (c) definire in particolare, se indicato, la dose totale, il tipo di frazionamento, i volumi di trattamento, il tipo di tecnica, il tipo di controllo del set-up guidato dalle immagini; (d) dare indicazione a un trattamento ormonale eventuale; (e) definire i criteri maggiormente influenzanti la prescrizione. è stata eseguita un’analisi descrittiva delle risposte.
Risultati
Trecento questionari sono stati consegnati agli oncologi radioterapisti partecipanti; 128 sono stati correttamente compilati e considerati per questa analisi (41%). Alcune importanti differenze sono state messe in evidenza nella prescrizione e nell’erogazione della RT, particolarmente riguardanti i volumi di trattamento e il frazionamento della dose. Sono state evidenziate alcune differenze con le raccomandazioni internazionali e i dati disponibili in letteratura sono stati rivisti e discussi.Conclusioni
Conclusioni
Nonostante i risultati di diversi studi clinici, persistono alcune differenze significative tra gli oncologi radioterapisti italiani nel trattamento dei pazienti con tumore prostatico. Questi pazienti meriterebbero un approccio più uniforme basato su raccomandazioni aggiornate, dettagliate e condivise sulla base delle evidenze disponibili.
Similar content being viewed by others
References/Bibliografia
Jemal A, Bray F, Center MM et al (2011) Global cancer statistics. CA Cancer J Clin 61: 69–90. Epub 2011 Feb 4. Erratum in: CA Cancer J Clin 61:134
Kuban DA, Thames HD, Levy LB et al (2003) Long-term multi-institutional analysis of stage T1–T2 prostate cancer treated with radiotherapy in the PSA era. Int J Radiat Oncol Biol Phys 57:915–928
Shipley WU, Thames HD, Sandler HM et al (1999) Radiation therapy for clinically localized prostate cancer: a multi-institutional pooled analysis. JAMA 281:1598–1604
Vieillot S, Fenoglietto P, Aillères N et al (2010) Prostate cancer. Cancer Radiother 14:S161–S173
Teoh M, Clark CH, Wood K et al (2011) Volumetric modulated arc therapy: a review of current literature and clinical use in practice. Br J Radiol 84:967–996
Sale C, Moloney P (2011) Dose comparisons for conformal, IMRT and VMAT prostate plans. J Med Imaging Radiat Oncol 55:611–621
Sze HC, Lee MC, Hung WM et al (2012) RapidArc radiotherapy planning for prostate cancer: Single-arc and double-arc techniques vs. intensitymodulated radiotherapy. Med Dosim 37:87–89
Yeung TP, Yartsev S, Rodrigues G, Bauman G (2011) Evaluation of image-guidance strategies with helical tomotherapy for localised prostate cancer. J Med Imaging Radiat Oncol 55:220–228
Magrini SM, Bertoni F, Vavassori V et al (2002) Practice patterns for prostate cancer in nine central and northern Italy radiation oncology centers: a survey including 1759 patients treated during two decades (1980–1998). Int J Radiat Oncol Biol Phys 52:1310–1319
Padhani AR (2011) Integrating multiparametric prostate MRI into clinical practice. Cancer Imaging 11:S27–S37
Clyne M (2011) Prostate cancer: PETCT for pelvic node staging. Nat Rev Urol 8:649
Bauman G, Belhocine T, Kovacs M et al (2012) (18)F-fluorocholine for prostate cancer imaging: a systematic review of the literature. Prostate Cancer Prostatic Dis 15:45–55
Alongi F, De Bari B, Franco F et al on behalf of AIRO Young and AIRO Prostate cancer Working Group (2013) The “PROCAINA (PROstate CAncer INdication Attitudes) Project” (Part I) — A survey among Italian radiation oncologists on post-operative radiotherapy in prostate cancer. Radiol Med, 2013 Jan 28 [Epub ahead of print]
D’Amico AV, Moran BJ, Braccioforte MH et al (2009) Risk of death from prostate cancer after brachytherapy alone or with radiation, androgen suppression therapy, or both in men with high-risk disease. J Clin Oncol 27:3923–3928
Heidenreich A, Bellmunt J, Bolla M et al (2011) EAU Guidelines on Prostate Cancer. Part 1: Screening, Diagnosis, and Treatment of Clinically Localised Disease. Eur Urol 59:61–71
Sullivan R, Peppercorn J, Sikora K et al (2011) Delivering affordable cancer care in high-income countries. Lancet Oncol 15:933–980
Valdagni R, Albers P, Bangma C et al (2011) The requirements of a specialist Prostate Cancer Unit: a discussion paper from the European School of Oncology. Eur J Cancer 47:1–7
Miller DC, Gruber SB, Hollenbeck BK, Montie JE, Wei JT (2006) Incidence of initial local therapy among men with lower-risk prostate cancer in the United States. Natl Cancer Inst 98(16):1134–1141
Chodak GW, Thisted RA, Gerber GS et al (1994) Results of conservative management of clinically localized prostate cancer. N Engl J Med 330:242–248
Albertsen PC, Hanley JA, Fine J (2005) 20-year outcomes following conservative management of clinically localized prostate cancer. JAMA 293:2095–2101
Albertsen PC, Hanley JA, Gleason DF, Barry MJ (1998) Competing risk analysis of men aged 55 to 74 years at diagnosis managed conservatively for clinically localized prostate cancer. JAMA 280:975–980
Klotz L, Zhang L, Lam A et al (2010) Clinical results of long-term follow-up of a large, active surveillance cohort with localized prostate cancer. J Clin Oncol 28:126–131
Tan CH, Wang J, Kundra V (2011) Diffusion weighted imaging in prostate cancer. Eur Radiol 21:593–603
Alonzi R, Padhani AR, Allen C (2007) Dynamic contrast enhanced MRI in prostate cancer. Eur J Radiol 63:335–350
Verma S, Rajesh A, Fütterer JJ et al (2010) Prostate MRI and 3D MR spectroscopy: how we do it. AJR Am J Roentgenol 194:1414–1426
Hara T, Kosaka N, Kishi H (1998) PET imaging of prostate cancer using carbon-11-choline. J Nucl Med 39:990–995
Farsad M, Schiavina R, Castellucci P et al (2005) Detection and localization of prostate cancer: correlation of (11) C-choline PET/CT with histopathologic step-section analysis. J Nucl Med 46:1642–1649
Martorana G, Schiavina R, Corti B et al (2006) 11C-choline positron emission tomography/computerized tomography for tumor localization of primary prostate cancer in comparison with 12-core biopsy. J Urol 176:954–960; discussion 960. Erratum in J Urol 176:2749
Husarik DB, Miralbell R, Dubs M et al (2008) Evaluation of [(18)F]-choline PET/CT for staging and restaging of prostate cancer. Eur J Nucl Med Mol Imaging 35:253–263
Kotzerke J, Prang J, Neumaier B et al (2000) Experience with carbon-11 choline positron emission tomography in prostate carcinoma. Eur J Nucl Med 27:1415–1419
Reske SN, Blumstein NM, Neumaier B et al (2006) Imaging prostate cancer with 11C-choline PET/CT. J Nucl Med 47:1249–1254
Kwee SA, Coel MN, Lim J, Ko JP (2005) Prostate cancer localization with 18 fluorine fluorocholine positron emission tomography. J Urol 173:252–255
Li X, Liu Q, Wang M et al (2008) C-11 Choline PET/CT imaging for differentiating malignant from benign prostate lesions. Clin Nucl Med 33:671–676
Skanjeti A, Pelosi E (2011) Lymph node staging with choline PET/CT in patients with prostate cancer: a review. ISRN Oncol 219064
Hennequin C, Rivera S, Quero L, Latorzeff I (2010) Prostate cancer: doses and volumes of radiotherapy. Cancer Radiother 14:474–478
Engelbrecht MR, Jager GJ, Laheij RJ et al (2002) Local staging of prostate cancer using magnetic resonance imaging: a meta-analysis. Eur Radiol 12:294–2302
Kestin L, Goldstein N, Vicini F et al (2002) Treatment of prostate cancer with radiotherapy: should the entire seminal vesicles be included in the clinical target volume? Int J Radiat Oncol Biol Phys 54:686–697
Mutanga TF, de Boer HC, van der Wielen GJ et al (2011) Margin evaluation in the presence of deformation, rotation, and translation in prostate and entire seminal vesicle irradiation with daily marker-based setup corrections. Int J Radiat Oncol Biol Phys 81:1160–1167
Meijer GJ, de Klerk J, Bzdusek K et al (2008) What CTV-to-PTV margins should be applied for prostate irradiation? Four-dimensional quantitative assessment using modelbased deformable image registration techniques. Int J Radiat Oncol Biol Phys 72:1416–1425
Seaward SA, Weinberg V, Lewis P et al (1998) Identification of a high-risk clinically localized prostate cancer subgroup receiving maximum benefit from whole-pelvic irradiation. Cancer J Sci Am 4:370–377
Ploysongsang SS, Aron BS, Shehata WM (1992) Radiation therapy in prostate cancer: whole pelvis with prostate boost or small field to prostate? Urology 40:18–26
Seaward SA, Weinberg V, Lewis P et al (1998) Improved freedom from PSA failure with whole pelvic irradiation for high-risk prostate cancer. Int J Radiat Oncol Biol Phys 42:1055–1062
Roach M 3rd, Marquez C, Yuo HS et al (1994) Predicting the risk of lymph node involvement using the pretreatment prostate specific antigen and Gleason score in men with clinically localized prostate cancer. Int J Radiat Oncol Biol Phys 28:33–37
Asbell SO, Martz KL, Shin KH et al (1998) Impact of surgical staging in evaluating the radiotherapeutic outcome in RTOG #77-06, a phase III study for T1BN0M0 (A2) and T2N0M0 (B) prostate carcinoma. Int J Radiat Oncol Biol Phys 40:769–782
Lawton CA, DeSilvio M, Roach M 3rd et al (2007) An update of the phase III trial comparing whole pelvic to prostate only radiotherapy and neoadjuvant to adjuvant total androgen suppression: updated analysis of RTOG 94-13, with emphasis on unexpected hormone/ radiation interactions. Int J Radiat Oncol Biol Phys 69:646–655
Pommier P, Chabaud S, Lagrange JL et al (2007) Is there a role for pelvic irradiation in localized prostate adenocarcinoma? Preliminary results of GETUG-01. J Clin Oncol 25:5366–5373
www.nccn.org, NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines 4.2011 (Last access on 10 May 2013)
Pollack A, Zagars GK, Starkschall G et al (2002) Prostate cancer radiation dose response: results of the M. D. Anderson phase III randomized trial. Int J Radiat Oncol Biol Phys 53:1097–1105
Peeters ST, Heemsbergen WD, Koper PC et al (2006) Dose-response in radiotherapy for localized prostate cancer: results of the Dutch multicenter randomized phase III trial comparing 68 Gy of radiotherapy with 78 Gy. J Clin Oncol 24:1990–1996
Latorzeff I, Mazurier J, Boutry C et al (2010) Benefit of intensity modulated and image-guided radiotherapy in prostate cancer. Cancer Radiother 14:479–487
Kuban DA, Tucker SL, Dong L et al (2008) Long-term results of the M. D. Anderson randomized dose-escalation trial for prostate cancer. Int J Radiat Oncol Biol Phys 70:67–74
Beckendorf V, Guerif S, Le Prisé E et al (2011) 70 Gy versus 80 Gy in localized prostate cancer: 5-year results of GETUG 06 randomized trial. Int J Radiat Oncol Biol Phys 80:1056–1063
Brenner DJ, Martinez AA, Edmundson GK (2002) Direct evidence that prostate tumors show high sensitivity to fractionation (low alpha/beta ratio), similar to late-responding normal tissue. Int J Radiat Oncol Biol Phys 52:6–13
Wang JZ, Guerrero M, Li XA (2003) How low is the alpha/beta ratio for prostate cancer? Int J Radiat Oncol Biol Phys 55:194–203
Ko EC, Forsythe K, Buckstein M et al (2011) Radiobiological rationale and clinical implications of hypofractionated radiation therapy. Cancer Radiother 15:221–229
Azria D, Aillères N, Llacer Moscardo C et al (2009) Radiothérapie de conformation avec modulation d’intensité dans le cancer de prostate: vers un nouveau standard. Cancer Radiother 13:409–415
de Crevoisier R, Garcia R, Louvel G et al (2009) Cone beam CT based image guided radiotherapy: implementation and clinical use. Cancer Radiother 13:482–489
Lisbona A, Averbeck D, Supiot S et al (2010) IMRT combined to IGRT: increase of the irradiated volume. Consequences? Cancer Radiother 14:563–570
Gelblum DY, Potters L, Ashley R et al (1999) Urinary morbidity following ultrasound-guided transperineal prostate seed implantation. Int J Radiat Oncol Biol Phys 45:59–67
Alemozaffar M, Regan MM, Cooperberg MR et al (2011) Prediction of erectile function following treatment for prostate cancer. JAMA 306:1205–1214
Zelefsky MJ, Kuban DA, Levy LB et al (2007) Multi-institutional analysis of long-term outcome for stages T1-T2 prostate cancer treated with permanent seed implantation. Int J Radiat Oncol Biol Phys 67:327–333
Yamada Y, Rogers L, Demanes DJ et al (2012) American Brachytherapy Society consensus guidelines for high-dose-rate prostate brachytherapy. Brachytherapy 11:20–32
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
De Bari, B., Alongi, F., Franco, P. et al. The “PROCAINA (PROstate CAncer INdication Attitudes) Project” (Part II) — A survey among Italian radiation oncologists on radical radiotherapy in prostate cancer. Radiol med 118, 1220–1239 (2013). https://doi.org/10.1007/s11547-013-0925-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-013-0925-z