Abstract
Even after successful treatment of aortic coarctation, a high risk of cardiovascular morbidity and mortality remains. Uncertainty exists on the factors contributing to this increased risk among which are the presence of (1) a residual narrowing leading to an additional resistance and (2) a less distensible zone disturbing the buffer function of the aorta. As the many interfering factors and adaptive physiological mechanisms present in vivo prohibit the study of the isolated impact of these individual factors, a numerical fluid–structure interaction model is developed to predict central hemodynamics in coarctation treatment. The overall impact of a stiffening on the hemodynamics is limited, with a small increase in systolic pressure (up to 8 mmHg) proximal to the stiffening which is amplified with increasing stiffening and length. A residual narrowing, on the other hand, affects the hemodynamics significantly. For a short segment (10 mm), the combination of a stiffening and narrowing (coarctation index 0.5) causes an increase in systolic pressure of 58 mmHg, with 31 mmHg due to narrowing and an additional 27 mmHg due to stiffening. For a longer segment (25 mm), an increase in systolic pressure of 50 mmHg is found, of which only 9 mmHg is due to stiffening.







Similar content being viewed by others
References
Aspden A, Nikiforakis N, Dalziel S, Bell J (2009) Analysis of implicit LES methods. Commun Appl Math Comput Sci 3:103–126
Bols J, De Santis G, Degroote J, Verhegghe B, Segers P, Vierendeels J (2013) Automated hexahedral mesh generation in a complex vascular tree: the extended treemesh method. In: ASME 2013 summer bioengineering conference. American Society of Mechanical Engineers, pp V01AT13A019–V001AT013A019
Bouchart F, Dubar A, Tabley A, Litzler PY, Haas-Hubscher C, Redonnet M, Bessou JP, Soyer R (2000) Coarctation of the aorta in adults: surgical results and long-term follow-up. Ann Thorac Surg 70:1483–1488. doi:10.1016/s0003-4975(00)01999-8
Carvalho JS, Redington AN, Shinebourne EA, Rigby ML, Gibson D (1990) Continuous wave doppler echocardiography and coarctation of the aorta—gradients and flow patterns in the assessment of severity. Br Heart J 64:133–137
Celermajer DS, Greaves K (2002) Survivors of coarctation repair: fixed but not cured. Heart 88:113–114. doi:10.1136/heart.88.2.113
Charonko JJ, Ragab SA, Vlachos PP (2009) A scaling parameter for predicting pressure wave reflection in stented arteries. J Med Device Trans Asme. doi:10.1115/1.3089140
Clark C (1976) Fluid-mechanics of aortic-stenosis. 2 Unsteady-flow experiments. J Biomech 9:567. doi:10.1016/0021-9290(76)90097-x
Cohen M, Fuster V, Steele PM, Driscoll D, McGoon DC (1989) Coarctation of the aorta—long-term follow-up and prediction of outcome after surgical-correction. Circulation 80:840–845
Coogan JS, Humphrey JD, Figueroa CA (2013) Computational simulations of hemodynamic changes within thoracic, coronary, and cerebral arteries following early wall remodeling in response to distal aortic coarctation. Biomech Model Mechanobiol 12:79–93. doi:10.1007/s10237-012-0383-x
de Divitiis M, Rubba P, Calabro R (2005) Arterial hypertension and cardiovascular prognosis after successful repair of aortic coarctation: a clinical model for the study of vascular function. Nutr Metabol Cardiovasc Dis 15:382–394. doi:10.1016/j.numecd.2005.08.002
De Santis G, Mortier P, De Beule M, Segers P, Verdonck P, Verhegghe B (2010) Patient-specific computational fluid dynamics: structured mesh generation from coronary angiography. Med Biol Eng Comput 48:371–380. doi:10.1007/s11517-010-0583-4
Degroote J, Bathe K-J, Vierendeels J (2009) Performance of a new partitioned procedure versus a monolithic procedure in fluid–structure interaction. Comput Struct 87:793–801. doi:10.1016/j.compstruc.2008.11.013
Ebeid M (2003) Balloon expandable stents for coarctation of the aorta: review of current status and technical considerations. Image Paediatr Cardiol 5:25–41
Fletcher SE, Nihill MR, Grifka RG, Olaughlin MP, Mullins CE (1995) Balloon angioplasty of native coarctation of the aorta—midterm follow-up and prognostic factors. J Am Coll Cardiol 25:730–734. doi:10.1016/0735-1097(94)00437-u
Formaggia L, Nobile F, Quarteroni A (2002) A one dimensional model for blood flow: application to vascular prosthesis. In: Ciarlet PG, Miyoshi T (eds) Mathematical modeling and numerical simulation in continuum mechanics, vol 19. Lecture notes in computational science and engineering, pp 137–153
Giddens DP, Mabon RF, Cassanova RA (1976) Measurements of disordered flows distal to subtotal vascular stenoses in thoracic aortas of dogs. Circ Res 39:112–119
Humphrey JD (2008) Mechanisms of arterial remodeling in hypertension: coupled roles of wall shear and intramural stress. Hypertension 52:195–200. doi:10.1161/hypertensionaha.107.103440
Jenkins NP, Ward C (1999) Coarctation of the aorta: natural history and outcome after surgical treatment. Qjm Mon J Assoc Physicians 92:365–371. doi:10.1093/qjmed/92.7.365
Johnston TA, Grifka RG, Jones TK (2004) Endovascular stents for treatment of coarctation of the aorta: acute results and follow-up experience. Catheter Cardiovasc Interv 62:499–505. doi:10.1002/ccd.20071
Keshavarz-Motamed Z, Kadem L (2011) 3D pulsatile flow in a curved tube with coexisting model of aortic stenosis and coarctation of the aorta. Med Eng Phys 33:315–324. doi:10.1016/j.medengphy.2010.10.017
Kim HJ, Vignon-Clementel IE, Figueroa CA, LaDisa JF, Jansen KE, Feinstein JA, Taylor CA (2009) On coupling a lumped parameter heart model and a three-dimensional finite element aorta model. Ann Biomed Eng 37:2153–2169. doi:10.1007/s10439-009-9760-8
LaDisa JF Jr, Dholakia RJ, Figueroa CA, Vignon-Clementel IE, Chan FP, Samyn MM, Cava JR, Taylor CA, Feinstein JA (2011) Computational simulations demonstrate altered wall shear stress in aortic coarctation patients treated by resection with end-to-end anastomosis. Congenit Heart Dis 6:432–443. doi:10.1111/j.1747-0803.2011.00553.x
LaDisa JF Jr, Figueroa CA, Vignon-Clementel IE, Kim HJ, Xiao N, Ellwein LM, Chan FP, Feinstein JA, Taylor CA (2011) Computational simulations for aortic coarctation: representative results from a sampling of patients. J Biomech Eng Trans Asme. doi:10.1115/1.4004996
Langille BL (1996) Arterial remodeling: relation to hemodynamics. Can J Physiol Pharmacol 74:834–841. doi:10.1139/cjpp-74-7-834
Liu B (2007) The influences of stenosis on the downstream flow pattern in curved arteries. Med Eng Phys 29:868–876. doi:10.1016/j.medengphy.2006.09.009
Marom G, Kim H-S, Rosenfeld M, Raanani E, Haj-Ali R (2013) Fully coupled fluid–structure interaction model of congenital bicuspid aortic valves: effect of asymmetry on hemodynamics. Med Biol Eng Comput 51:839–848. doi:10.1007/s11517-013-1055-4
Marshall AC, Perry SB, Keane JF, Lock JE (2000) Early results and medium-term follow-up of stent implantation for mild residual or recurrent aortic coarctation. Am Heart J 139:1054–1060. doi:10.1067/mhj.2000.106616
Menon A, Wendell DC, Wang H, Eddinger TJ, Toth JM, Dholakia RJ, Larsen PM, Jensen ES, LaDisa JF Jr (2012) A coupled experimental and computational approach to quantify deleterious hemodynamics, vascular alterations, and mechanisms of long-term morbidity in response to aortic coarctation. J Pharmacol Toxicol Methods 65:18–28. doi:10.1016/j.vascn.2011.10.003
Moireau P, Xiao N, Astorino M, Figueroa CA, Chapelle D, Taylor CA, Gerbeau JF (2012) External tissue support and fluid–structure simulation in blood flows. Biomech Model Mechanobiol 11:1–18. doi:10.1007/s10237-011-0289-z
Oechslin EN (2008) Does a stent cure hypertension? Heart 94:828–829. doi:10.1136/hrt.2007.130013
Olivieri LJ, de Zelicourt DA, Haggerty CM, Ratnayaka K, Cross RR, Yoganathan AP (2011) Hemodynamic modeling of surgically repaired coarctation of the aorta. Cardiovasc Eng Technol 2:288–295. doi:10.1007/s13239-011-0059-1
Orourke MF, Cartmill TB (1971) Influence of aortic coarctation on pulsatile hemodynamics in proximal aorta. Circulation 44:281
Pedersen TA (2012) Late morbidity after repair of aortic coarctation. Dan Med J 59:B4436
Pihkala J, Thyagarajan GK, Taylor GP, Nykanen D, Benson LN (2001) The effect of implantation of aortic stents on compliance and blood flow. An experimental study in pigs. Cardiol Young 11:173–181. doi:10.1017/s1047951101000075
Prendergast PJ, Lally C, Daly S, Reid AJ, Lee TC, Quinn D, Dolan F (2003) Analysis of prolapse in cardiovascular stents: a constitutive equation for vascular tissue and finite-element modelling. J Biomech Eng Trans Asme 125:692–699. doi:10.1115/1.1613674
Rothman A (1998) Coarctation of the aorta: an update. Curr Probl Pediatr 28:37–60. doi:10.1016/S0045-9380(98)80039-X
Stergiopulos N, Segers P, Westerhof N (1999) Use of pulse pressure method for estimating total arterial compliance in vivo. Am J Physiol Heart Circ Physiol 276:H424–H428
Stewart AB, Ahmed R, Travill CM, Newman CGH (1993) Coarctation of the aorta life and health 20–44 years after surgical repair. Br Heart J 69:65–70
Taelman L, Degroote J, Swillens A, Vierendeels J, Segers P (2014) Fluid–structure interaction simulation of pulse propagation in arteries: numerical pitfalls and hemodynamic impact of a local stiffening. Int J Eng Sci 77:1–13. doi:10.1016/j.ijengsci.2013.12.002
Valverde I, Staicu C, Grotenhuis H, Marzo A, Rhode K, Shi Y, Brown A, Tzifa A, Hussain T, Greil G, Lawford P, Razavi R, Hose R, Beerbaum P (2011) Predicting hemodynamics in native and residual coarctation: preliminary results of a rigid-wall computational-fluid-dynamics model (RW-CFD) validated against clinically invasive pressure measures at rest and during pharmacological stress. J Cardiovasc Magn Reson 13:1–4. doi:10.1186/1532-429X-13-S1-P49
van den Wijngaard JPHM, Siebes M, Westerhof BE (2009) Comparison of arterial waves derived by classical wave separation and wave intensity analysis in a model of aortic coarctation. Med Biol Eng Compu 47:211–220. doi:10.1007/s11517-008-0387-y
Verhaaren H, De Mey S, Coomans I, Segers P, De Wolf D, Matthys D, Verdonck P (2001) Fixed region of nondistensibility after coarctation repair: in vitro validation of its influence on Doppler peak velocities. J Am Soc Echocardiogr 14:580–587. doi:10.1067/mje.2001.113256
Vogt M, Kühn A, Baumgartner D, Baumgartner C, Busch R, Kostolny M, Hess J (2005) Impaired elastic properties of the ascending aorta in newborns before and early after successful coarctation repair: proof of a systemic vascular disease of the prestenotic arteries? Circulation 111:3269–3273. doi:10.1161/circulationaha.104.529792
Vriend JWJ, Mulder BJM (2005) Late complications in patients after repair of aortic coarctation: implications for management. Int J Cardiol 101:399–406. doi:10.1016/j.ijcard.2004.03.056
Wendell DC, Samyn MM, Cava JR, Ellwein LM, Krolikowski MM, Gandy KL, Pelech AN, Shadden SC, LaDisa JF Jr (2013) Including aortic valve morphology in computational fluid dynamics simulations: initial findings and application to aortic coarctation. Med Eng Phys 35:723–735. doi:10.1016/j.medengphy.2012.07.015
Acknowledgments
This research was funded by the Research Foundation—Flanders (FWO-Vlaanderen), Project No. 3G008509.
Author information
Authors and Affiliations
Corresponding author
Appendix: Mesh and time step sensitivity study
Appendix: Mesh and time step sensitivity study
Given the focus of the study on pressure, the criterion for the grid convergence and time step dependency study was the accuracy of the predicted pressures along the aortic arch. The case used for the analysis was the case with the shortest stenosis length (1 cm) and highest degree of stenosis (coarctation index 0.5).
1.1 Mesh sensitivity analysis
Four different, full hexahedral uniform meshes (R1, R2, R3 and R4) with an increasing number of elements in the boundary layer (ranging from 4 to 8 layers), the transversal and axial direction were constructed, with R4 considered as reference. A conforming mesh was applied in the fluid and solid domain. The number of cells is depicted in Table 1, together with the calculation time required to compute one cardiac cycle (on two 10-core Intel Xeon E5-2680v2 processors).
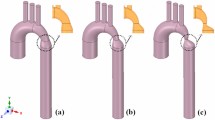
As the flow distal to the stenosis is complex and highly disturbed (Reynolds numbers up to 11,139), a high mesh density is required in this region to resolve the flow field in space. This is realized by locally adapting the fluid mesh. The resulting fluid mesh (R5) has, compared to the finest mesh (R4), a higher mesh density in the coarctation zone, but a coarser grid proximal to the stenosis and in the lower part of the descending aorta (see Fig. 8).
Left indication of sections where pressure was calculated (p proximal; d distal). Right a mesh for the fluid domain (blue) and the arterial wall (red) of an aortic arch with aortic coarctation. Note the axial coarsening toward the descending aorta (R5). b, c The cross-sectional grids of the fluid mesh at the coarctation (coa) and the descending aorta (desc), which result from multiblock structures R4 (uniform grid refinement) and R5 (local grid refinement) (color figure online)
Figure 9 depicts the pressure along the centerline of the aorta at peak systole, with Table 1 tabulating the mean error of the pressure in different cross sections (indicated by the dashed lines in Fig. 9). These errors are defined with respect to the reference grid R4 and relative to the pressure amplitude in the corresponding cross section. The mean error thereby denotes the error averaged over one cardiac cycle and over the respective cross section. From the results in Table 1, it can be seen that even for meshes with a low cell density, the mean errors proximal, halfway and distal to the coarctation zone remain low (<2 %). When comparing the locally refined grid R5 with the uniformly refined grids R3 and R4, an important reduction in computation time is gained (23 h 38 min per cardiac cycle vs 30 h 33 min and 40 h 38 min) without a loss in accuracy. The mean error obtained with the mesh R5 stays below 1.15 %, and comparable errors are found as for the mesh R3.
1.2 Time step sensitivity analysis
Figure 10 illustrates the impact of the time step size on the pressure evolution at different cross sections along the aorta. It can be observed that the results in the proximal part and at the coarctation zone are more or less time step independent, whereas the small pressure oscillations in the distal part are not captured with a large time step size (of 4 or 5 ms). Moreover, the oscillations developing in d3 are not even resolved properly with a time step size of 1 ms. As such, the time step size was further decreased to 0.5 and 0.25 ms and the results are shown in Fig. 11. An unstable behavior was found if a small time step size was applied. The observed oscillations responsible for this behavior were indeed not resolved for the simulations using larger time step sizes. Because the oscillations itself are resolved by multiple time steps and the frequency of the oscillations is more or less time step independent, it is presumed that these oscillations do not arise from a numerical instability but have a physical origin, triggered by the disturbed blood flow. In a physiological setting, this oscillation would, however, be cushioned by the damping nature of the surrounding tissue. We believe that the lack of physical damping in our model resulted in the observed oscillations that eventually got unstable when using a time step size smaller than 1 ms.
Influence of the time step size on the pressure evolution at proximal cross section p1, halfway the coarctation zone (coa) and at two distal cross sections (d1 and d3). See Fig. 8 for an indication of these plane locations
To test this hypothesis, Rayleigh damping was added to the structural model and the simulation using a time step size of 0.5 ms was repeated. The Rayleigh damping coefficients α and β were selected such that 1 % damping of the waves with a 1-Hz frequency (close to the frequency of the cardiac cycle) was obtained and 20 % damping for the 250-Hz waves (i.e., the frequency of the observed oscillations). These constrictions resulted in a value of 0.116 for the mass proportional damping parameter α and 0.000255 for the stiffness proportional damping β. It is demonstrated in Fig. 11 that the unstable behavior indeed disappears with the use of Rayleigh damping.
The larger pressure oscillations at the start of the simulation (t < 0.2 s) for the case with Rayleigh damping is explained by the temporal discretization schemes used at the start. The simulation without damping is started with a first-order scheme, to facilitate the startup. After 0.2 s, the accuracy is improved by switching to a second-order scheme. For the case with damping, a second-order scheme can be used from the start on. In this study, a time step size of 2 ms has been used as a compromise between accuracy and computation time. The error obtained with this time step size is sufficiently smaller than the mutual differences in results.
Rights and permissions
About this article
Cite this article
Taelman, L., Bols, J., Degroote, J. et al. Differential impact of local stiffening and narrowing on hemodynamics in repaired aortic coarctation: an FSI study. Med Biol Eng Comput 54, 497–510 (2016). https://doi.org/10.1007/s11517-015-1336-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-015-1336-1