Abstract
We investigated whether eating and body image disturbances in mid-adolescence were associated with substance use in young adulthood. Participants (n = 1566) completed the drive for thinness, bulimic behavior, and body dissatisfaction subscales from the Eating Disorder Inventory during adolescence (15–16 years), and reported frequencies of substance use (tobacco, cannabis, binge drinking, other illicit substances) across young adulthood (19–20, 23–24, and 27–28 years). Adolescent body dissatisfaction was associated with a 10% increase in the rate of binge drinking and tobacco smoking, with effects being of similar magnitude in men and women, and across young adulthood. The association between bulimic behavior and tobacco smoking was strongest in the earlier years of young adulthood (19–20 years). Relationships between cannabis use, bulimic behavior, and body dissatisfaction were evident in men only. Findings highlight important targets for prevention programs, as well as focused monitoring efforts to identify individuals at risk of later substance use.
Similar content being viewed by others
There has been widespread interest in the course and impact of eating and body image disturbances after their first presentation in adolescence. Prior reports reveal that eating and body image disturbances have increased nearly three-fold over the past two decades, with between 15 and 50% of adolescents exhibiting significant weight concerns or disordered eating behaviors (Mitchison et al., 2019). Eating and body image disturbances can persist into middle to older adulthood (Brown et al., 2020), transition to a life-threatening eating disorder (Neumark-Sztainer et al., 2006), and lead to impairments in functioning (Linardon et al., 2021; Mitchell, 2016; Mitchison et al., 2012).
Research has also consistently reported high comorbidity rates (~ 30%) between eating and substance use disorders (Bahji et al., 2019). One possible explanation is that body image concerns experienced in younger people may motivate consumption of stimulant drugs or tobacco cigarettes as a chemical means of weight control (Stice & Shaw, 2003; Stice et al., 2004). This may be particularly so in adolescence where smoking, for example, may be initiated to mitigate the weight gain resultant from recurrent binge eating or regulate the emotional distress that accompanies binge-purge behaviors (Sonneville et al., 2013). Another explanation is that underlying deficiencies in impulse control may constitute a shared risk factor for the overconsumption of food and psychoactive substances (Stice et al., 2004). Alternatively, a neurobiological explanation has been profited by Gearhardt and colleagues (Gearhardt et al., 2011) who propose that the tendency towards overconsumption could also stem from a dysregulation of the neural circuitry implicated in reward seeking, given that both eating and psychoactive substances activate this network.
Despite clear evidence of high comorbidity, exceedingly little is known about longer term relationships between eating and body image problems in adolescence and later substance use. Stice and colleagues conducted a series of studies in adolescent girls, finding that elevated levels of body dissatisfaction and bulimic pathology at baseline predicted smoking onset (Stice & Shaw, 2003), substance use onset (Stice et al., 2004), and poly-substance use (Measelle et al., 2006) at follow-up periods spanning 2–5 years. Similar findings have also emerged between baseline bulimic behaviors in adolescent girls and later onset of cannabis use over a longer period (6–8 years; e.g., Sonneville et al., 2013). Recent evidence also suggests that comparable risk relationships exist in males, with a prospective study of community-based adult men finding elevated body image concerns at baseline predicting a higher odds of binge drinking at 1-year follow-up (Eik‐Nes et al., 2018). However, one prospective study (Johnson et al., 2002) of adolescents (51% female) found that the presence of a diagnostic-level eating disorder at baseline (Mage = 13.8 years) did not increase risk for any substance abuse onset in early adulthood (Mage = 22.0 years).
Longer term effects of eating and body image disturbances in adolescence on later substance use into young adult life remain largely unknown. However, there is no reason to suspect that underlying mechanisms linking these behaviors in adolescence (e.g., impulse control and affect regulation strategies) do not persist beyond this period. To address this gap in our knowledge, additional studies, conducted in mature early life-course cohorts, are needed to map risk relationships into young adulthood. This work needs to include males in light of growing evidence indicating that the course, impact, and onset of eating disturbances, body image concerns, and substance use differ between the sexes (McHugh et al., 2018; Murray et al., 2017). To inform preventive interventions, this work would ideally be conducted within population-based cohort studies, where eating and body image problems are assessed (across multiple indices) at their initial onset, with comprehensive follow-up across adolescence and into young adult life. This would allow examination of temporal separation between eating/body image problems and substance use behaviors, and address prognostic questions about the longer term associations between eating/body image problems in adolescence and later substance use.
Here, we capitalize on rare prospective data from one of Australia’s longest running, population-based cohort studies that has been following > 2000 Australian children and their families from infancy to young adulthood since 1983. Specifically, we used assessment of eating and body image disturbances in adolescence (15–16 years) and substance use in young adulthood (19–20, 23–24, and 27–28 years) to examine the extent to which (1) bulimic behavior, body dissatisfaction, and drive for thinness in adolescence are associated with long-term risk for alcohol, tobacco, cannabis, and other illicit substance use in young adulthood; (2) risk relationships weaken, stabilize, or strengthen across the young adulthood years; and (3) risk relationships are moderated by sex. It was hypothesized that higher scores on bulimic behavior, body dissatisfaction, and drive for thinness in adolescence would be associated with higher frequency of alcohol, tobacco, cannabis, and other illicit substance use in young adulthood. No a priori hypotheses were derived for when these associations might be strongest (or weakest) or for possible sex differences, given the limited available research in this area.
Method
Participants and Procedure
Participants were drawn from the Australian Temperament Project (ATP), a 16-wave longitudinal study tracking the psychosocial development of young people from infancy to adulthood. In 1983, 67 Local Government Areas (LGAs) in the state of Victoria were randomly selected based on Australian Bureau of Statistics, to provide a representative community sample (Sanson et al., 1985). Parents of every 4–8-month-old infant who visited one of the selected centers between 22nd April and 6th May (1983) were invited to participate. Approximately 3000 questionnaires were administered. The baseline sample consisted of 2443 infants aged between 4 and 8 months, recruited in 1983 from urban and rural areas and representative of the state of Victoria, Australia. Since then, families have been invited to participate via mail surveys approximately every 2 years until 19–20 years and every 4 years thereafter (Prior et al., 2000). The ATP has sustained approximately 1% attrition per annum.. Further details regarding study design and procedure are presented elsewhere (Vassallo & Sanson, 2013). Data collection waves have been variously approved by Human Research Ethics Committees at the University of Melbourne, the Australian Institute of Family Studies and/or the Royal Children’s Hospital, Melbourne. For this study, data for the primary analytic variables are drawn from four waves spanning adolescence (eating and body image disturbances; 1 wave: age 15–16 years) and young adulthood (substance use; 3 waves: ages 19–20, 23–24, and 27–28 years). To be included in the current study, participants needed to have provided relevant data in adolescence or young adulthood. This resulted in a sample size of 1566 (805 females) for the current study.
Measures
Eating and Body Image Disturbances
The Eating Disorder Inventory (EDI; Garner et al., 1983) drive for thinness and bulimia subscales were completed by adolescents (15–16 years) with minor wording alterations to suit Australian adolescents (see Krug et al., 2016). The drive for thinness subscale was assessed using 7 items such as “I am preoccupied with the desire to be thinner.” The bulimia subscale was assessed using 7 items, such as “I eat moderately in front of others and stuff myself when they’re gone.” A body dissatisfaction scale, assessing discontentment with overall shape and size of body regions, was specifically developed for the ATP. It consisted of four items, including “I think I am too fat,” “I feel satisfied with the shape of my body” (reversed), “I think I am not muscular enough,” and “I think I am too skinny.” The decision to use this subscale rather than the original EDI subscale was based on substantial numbers of missing items (and consequently missing data) in the previous wave and negative feedback from participants (Prior et al., 2000). Each item from the three scales was rated along a 6-point scale (1 = never, 6 = always), as is recommended for normative samples where the prevalence of clinically significant disorders is low.
Substance Use
Substance use was assessed at three waves in young adulthood (19–20, 23–24, and 27–28 years). Participants were asked to report the number of days in the last month that they used alcohol (any/binge drinking; ≥ five drinks on one occasion/in quick succession), tobacco, cannabis, and six other illicit substances (LSD, ecstasy, amphetamines, heroin, cocaine, and sleeping tablets/tranquilizers). Illicit substance use frequency was defined as the maximum number of days in the last month the participant had used any of the six substances.
Potential Confounding Variables
Potential confounders were assessed according to the modified disjunctive cause criteria, identified as pre-exposure variables that are associated with the exposure and/or outcomes, or a proxy for a potential unmeasured confounder, but unlikely to act as an instrument (associated with the outcome only via exposure; VanderWeele, 2019). These included parent reported family characteristics of country of birth (either parent not born in Australia), low parental education (< year 12), separation/divorce during the participant’s childhood (ages 0–13 years), experience of stressful events (age 11–14 years), and parental warmth and harsh parental discipline (ages 13–14 years, see Prior et al., 1999). We also included individual pre-exposure factors of participant sex, early puberty onset (menarche/voice break prior to 12 years old), BMI at ages 12–13, self-reported elevated depression/anxiety symptoms (age 13–14 years; Short Mood and Feelings Questionnaire ≥ 11 (Angold & Stephen, 1995), the anxious-fearful scale from the Rutter Child Behavior Questionnaire > 1 (Rutter et al., 1970), easy-difficult temperament (age 11–14 years), and both peer and family attachment (age 13–14 years; Armsden & Greenberg, 1987). Finally, to reduce the potential for reverse causality where possible (VanderWeele, 2019), early (age 13–14 years) substance use (alcohol, tobacco, or cannabis) behavior was controlled for.
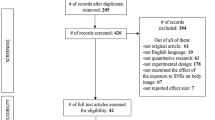
Statistical Analyses
All analyses were conducted in Stata 15. Negative binomial generalized estimating equations (GEEs) with an exchangeable working correlation (to account for repeated measures) were used to estimate associations between adolescent EDI subscales (15–16 years) and substance use frequencies at young adult waves (19–20, 23–24, and 27–28 years). Models were fitted separately for the relationships between each eating/body image disturbance and substance type. For each model, analyses were estimated: (1) adjusting for outcome wave only, (2) adjusting for family background characteristics and participant sex, and (3) adjusting for all potential confounders. Fully adjusted models were then repeated by including an interaction between each eating/body image disturbance subscale and outcome measurement wave to examine whether associations variated across young adulthood.
Multiple imputation was used to handle missing data in the inferential analyses. Fifty complete datasets were imputed, based on a multivariate normal model (Lee & Carlin, 2010). Binary variables were imputed as continuous variables and then back transformed with adaptive rounding following imputation (Bemaards et al., 2007). Estimates were obtained by pooling results across the 50 imputed datasets using Rubin’s rules (Rubin, 1988). Prior to inferential analyses, eating and body image disturbance scores were standardized (z-scores). Incidence rate ratios (IRRs) from the negative binomial models are interpreted as the change in substance use counts (i.e., number of days) for every standard deviation change in eating and body image disturbances, in terms of percentage increase (Piza, 2012).
Results
Descriptive statistics for study variables are presented in Table 1. Adolescent females reported higher levels of drive for thinness, bulimic behavior, and body dissatisfaction than males. While young adult binge drinking frequency was higher in men than women, tobacco, cannabis, and illicit use frequencies were comparable.
The results of the negative binomial GEE models where substance use frequencies were regressed onto each of the EDI subscales are presented in Table 2. After adjusting for outcome period and potential confounders, higher body dissatisfaction scores were associated with > 10% increase in the frequency of both binge drinking (IRR = 1.11) and tobacco use (IRR = 1.11) across young adulthood. These associations were of similar strength across young adult ages and in both men and women. In addition, high bulimia scores were associated with > 10% increase in the frequency of tobacco use (IRR = 1.10) across young adulthood; this association was strongest in early young adult life (19–20 years; IRR = 1.17, Table S1).
Although statistically significant main effects for EDI subscales were not evident for cannabis use, significant gender × bulimia and gender × body dissatisfaction interactions emerged, such that higher scores on each subscale were associated with higher cannabis frequency only in men, IRR = 1.24 and 1.35 (Table S2), respectively. Associations were not evident between drive for thinness and any substance use, nor illicit substance use frequency and any EDI subscale. For completeness, we present the three-way interactions between each EDI subscale scores, participant sex, and outcome assessment wave in Figures S1, S2, S3, and S4.
Discussion
Using rare prospective data from one of Australia’s longest running studies of social and emotional development, we found that certain indices of eating and body image disturbances in adolescence were associated with long-term substance use outcomes in young adulthood. Specifically, adolescent body dissatisfaction was associated with a 10% increase in the rate of binge drinking and tobacco smoking, with risk relationships remaining stable across the 20 s and across sex. Adolescent bulimic behavior was also associated with a 10% increase in the rate of tobacco smoking, which was strongest in the early 20 s. Bulimic behavior and body dissatisfaction was associated with increased rate of cannabis use, but only in men. Taken together, these findings highlight the potential longer term importance of investing in evidence-based universal, selective and indicated prevention programs designed to address eating and body image disturbances as they typically emerge in adolescence.
Findings from this study extend insights from prior longitudinal research (Measelle et al., 2006; Sonneville et al., 2013; Stice & Shaw, 2003; Stice et al., 2004) in several important ways. First, adolescent eating/body image disturbances are associated with substance use over a much longer period of development than has previously been documented (extending through the 20 s). Second, such risk relationships are nuanced and depend on the type of symptom assessed, with body dissatisfaction and bulimic behavior being most influential. Third, there may be sex-specific pathways associated with cannabis use risk, with body dissatisfaction and bulimic behavior emerging as risk factors for men but not women. Fourth, risk relationships remain largely stable across the young adult years, suggesting that earlier disturbances in eating and body image are associated with long-term and stable substance use outcomes.
Potential Mechanisms
In line with the modified disjunctive cause criteria (VanderWeele, 2019), we accounted for many potential confounding factors to develop models that would support causal claims about the impact of adolescent eating and body image disturbances on later substance use frequency. Research should now seek to uncover plausible mechanisms through which this risk is transmitted. A potential explanation for the identified associations between body dissatisfaction, bulimia scores, and tobacco use is that eating and body image problems encountered in younger people may encourage initiation of tobacco smoking as a means to alleviate weight gain resultant from excess caloric consumption or to modulate any distress arising from bulimic behaviors (Stice & Shaw, 2003). Such underlying motivations (weight control and defensive affect regulation) may persist well into adult life, in part explaining longer term associations. Another mechanistic explanation for associations between bulimic behaviors, tobacco smoking, and cannabis use may signal deficiencies in neural circuity or developmental influences that underpin reward-seeking behaviors (Gearhardt et al., 2011; Treasure et al., 2018). This explanation may explain why these associations were strongest in males, as prior research has established sex-specific differences in both hormone secretion and activation of neural regions implicated in sensation seeking behaviors and impulse control (Cross et al., 2013; Harden et al., 2018). Further research is needed to both replicate findings and further examine possible developmental pathways.
Future Directions
Findings highlight several potential avenues for future research. First, there is a need to examine potential explanatory mechanisms that underpin the identified risk relationships. We suggest taking a broad perspective when seeking to understand these associations, whereby biological (e.g., neural circuitry, hormones, pubertal impacts), psychological (e.g., fear of weight gain, affect), and social (e.g., peer pressures) influences are considered potential mediating mechanisms. Second, future research should employ longer follow-up assessments to get a more comprehensive understanding of these risk relationships. It is possible that certain associations strengthen, weaken, or diminish across middle and older adulthood, which may have important implications for prevention. Third, future research should assess whether the identified associations are causal in nature, by conducting randomized trials designed to manipulate eating and body image disturbances and observing what long-term impact this has on substance use behaviors.
Broader Implications
Findings from this study also highlight the importance of the adolescent years as a key period for investment in prevention and early intervention. Targeted educational campaigns in healthcare and school settings that seek to promote greater awareness of longer term risks of eating and body image disturbances in adolescence could be an important translational outcome from this work (Harrer et al., 2020). Likewise, monitoring systems that provide policy makers with a population snapshot of the extent of eating- and body image-specific risks in young populations would allow better planning of prevention programs. More detailed screening within high-school settings could further pinpoint those who could benefit from enriched support, diverting them to empirically supported clinical and/or health educational programs.
Strengths and Limitations
Despite key strengths to this study, including the large sample size, long follow-up assessments, and use of population-based cohort data, there are also limitations to consider. One limitation is the use of self-report assessments, which could have produced underestimations or overestimations related to the frequency of substance use patterns or severity of eating and body image disturbances. Second, since the EDI was not administered to participants between ages 17 and 28 years, we were unable to pinpoint specific ages at which eating and body image disturbances are most influential, nor were we able to investigate potential dynamic and bi-directional relationships. Addressing such questions in future studies could yield a more nuanced insight towards when best to intervene on these types of problems. Third, although we adjusted for a range participant factors, including early adolescence substance use, as with all observational studies, the potential for confounding remains. Randomized prevention trials that seek to modify these types of eating and body image disturbances and observe what effect this has on later substance use would be valuable for generating experimental evidence that these variables are causally related.
Conclusion
Here, we suggest that eating and body image disturbances in adolescence may play a long-term role in influencing patterns of substance use in young adulthood. Future research is now needed to replicate our findings, as well as investigate causal pathways (mechanisms) through which early disturbances in eating and body image operate to create longer term risk for substance problems in young adulthood. To the extent to which our findings are confirmed through this process, better monitoring of, and intervention with, adolescents with eating and body disturbances could yield significant long-term health dividends.
Data Availability
Ethics approvals for this study do not permit the data to be made publicly available, due to limitations of participant consent and concerns regarding potential re-identifiability. The current institutional body responsible for ethical approval is the Royal Children’s Hospital Human Research Ethics Committee. Enquires about access to pre-existing cohort data used in this submission are possible through our institutional data access protocol (https://lifecourse.melbournechildrens.com/data-access/).
References
Angold, A., & Stephen, C. (1995). Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. Age (years), 6, 237–249.
Armsden, G. C., & Greenberg, M. T. (1987). The inventory of parent and peer attachment: Individual differences and their relationship to psychological well-being in adolescence. Journal of Youth and Adolescence, 16, 427–454.
Bahji, A., Mazhar, M. N., Hudson, C. C., Nadkarni, P., MacNeil, B. A., & Hawken, E. (2019). Prevalence of substance use disorder comorbidity among individuals with eating disorders: A systematic review and meta-analysis. Psychiatry Research, 273, 58–66.
Bemaards, C. A., Belin, T. R., & Schafer, J. L. (2007). Robustness of a multivariate normal approximation for imputation of binary incomplete data. Statistics in Medicine, 26, 1368–1382.
Brown, T. A., Forney, K. J., Klein, K. M., Grillot, C., & Keel, P. K. (2020). A 30-year longitudinal study of body weight, dieting, and eating pathology across women and men from late adolescence to later midlife. Journal of Abnormal Psychology, 129, 376–386. https://doi.org/10.1037/abn0000519
Cross, C. P., Cyrenne, D.-L.M., & Brown, G. R. (2013). Sex differences in sensation-seeking: A meta-analysis. Scientific Reports, 3, 1–5.
Eik-Nes, T. T., Austin, S. B., Blashill, A. J., Murray, S. B., & Calzo, J. P. (2018). Prospective health associations of drive for muscularity in young adult males. International Journal of Eating Disorders, 51, 1185–1193.
Garner, D. M., Olmstead, M. P., & Polivy, J. (1983). Development and validation of a multidimensional eating disorder inventory for anorexia nervosa and bulimia. International Journal of Eating Disorders, 2, 15–34.
Gearhardt, A. N., Davis, C., Kuschner, R., Brownell, D., & K. (2011). The addiction potential of hyperpalatable foods. Current Drug Abuse Reviews, 4, 140–145.
Harden, K. P., Mann, F. D., Grotzinger, A. D., Patterson, M. W., Steinberg, L., Tackett, J. L., & Tucker-Drob, E. M. (2018). Developmental differences in reward sensitivity and sensation seeking in adolescence: Testing sex-specific associations with gonadal hormones and pubertal development. Journal of Personality and Social Psychology, 115, 161.
Harrer, M., Adam, S. H., Messner, E. M., Baumeister, H., Cuijpers, P., Bruffaerts, R., Auerbach, R. P., Kessler, R. C., Jacobi, C., Taylor, C. B., & Ebert, D. D. (2020). Prevention of eating disorders at universities: A systematic review and meta-analysis. International Journal of Eating Disorders, 53, 813–833. https://doi.org/10.1002/eat.23224
Johnson, J. G., Cohen, P., Kasen, S., & Brook, J. S. (2002). Eating disorders during adolescence and the risk for physical and mental disorders during early adulthood. Archives of General Psychiatry, 59, 545–552.
Krug, I., King, R. M., Youssef, G. J., Sorabji, A., Wertheim, E. H., Le Grange, D., ... & Olsson, C. A. (2016). The effect of low parental warmth and low monitoring on disordered eating in mid-adolescence: Findings from the Australian Temperament Project. Appetite, 105, 232–241.
Lee, K. J., & Carlin, J. B. (2010). Multiple imputation for missing data: Fully conditional specification versus multivariate normal imputation. American Journal of Epidemiology, 171, 624–632.
Linardon, J., Greenwood, C. J., Fuller-Tyszkiewicz, M., Macdonald, J. A., Spry, E., Hutchinson, D. M., Youssef, G., J., Sanson, A., Wertheim E, H., McIntosh, J E, Le Grange, D, Letcher, P., & Olsson, C. A. (2021). Young adult mental health sequelae of eating and body image disturbances in adolescence. International Journal of Eating Disorders. https://doi.org/10.1002/eat.23575
McHugh, R. K., Votaw, V. R., Sugarman, D. E., & Greenfield, S. F. (2018). Sex and gender differences in substance use disorders. Clinical Psychology Review, 66, 12–23.
Measelle, J. R., Stice, E., & Hogansen, J. M. (2006). Developmental trajectories of co-occurring depressive, eating, antisocial, and substance abuse problems in female adolescents. Journal of Abnormal Psychology, 115, 524.
Mitchell, J. E. (2016). Medical comorbidity and medical complications associated with binge-eating disorder. International Journal of Eating Disorders, 49, 319–323.
Mitchison, D., Hay, P. J., Slewa-Younan, S., & Mond, J. (2012). Time trends in population prevalence of eating disorder behaviors and their relationship to quality of life. PLoS ONE, 7, 1–7. https://doi.org/10.1371/journal.pone.0048450
Mitchison, D., Mond, J., Bussey, K., Griffiths, S., Trompeter, N., Lonergan, A., . . . Hay, P. (2019). DSM-5 full syndrome, other specified, and unspecified eating disorders in Australian adolescents: Prevalence and clinical significance. Psychological Medicine, 1–10.
Murray, S. B., Nagata, J. M., Griffiths, S., Calzo, J. P., Brown, T. A., Mitchison, D., . . . Mond, J. M. (2017). The enigma of male eating disorders: A critical review and synthesis. Clinical Psychology Review, 57, 1–11. https://doi.org/10.1016/j.cpr.2017.08.001
Neumark-Sztainer, D., Wall, M., Guo, J., Story, M., Haines, J., & Eisenberg, M. (2006). Obesity, disordered eating, and eating disorders in a longitudinal study of adolescents: How do dieters fare 5 years later? Journal of the American Dietetic Association, 106, 559–568.
Piza, E. L. (2012). Using Poisson and Negative Binomial Regression Models to Measure the Influence of Risk on Crime Incident Counts.
Prior, M., Sanson, A., Smart, D., & Oberklaid, F. (1999). Psychological disorders and their correlates in an Australian community sample of preadolescent children. The Journal of Child Psychology and Psychiatry and Allied Disciplines, 40, 563–580.
Prior, M., Sanson, A., Smart, D., & Oberklaid, F. (2000). Pathways from infancy to adolescence: Australian Temperament Project 1983–2000. Australian Institute of Family Studies.
Rubin, D. B. (1988). An overview of multiple imputation. Proceedings of the section on survey research methods of the annual meeting of the american statistical association (pp. 79–84). New Orleans, LA: American Statistical Organization. Available at https://www.amstat.org/Sections/Srms/Proceedings/papers/1988_016.pdf
Rutter, M., Tizard, J., & Whitmore, K. (1970). Education, health and behaviour: psychological and medical study of childhood development: Longman Group Limited.
Sanson, A. V., Prior, M., & Oberklaid, F. (1985). Normative data on temperament in australian infants. Australian Journal of Psychology, 37(2), 185–195. https://doi.org/10.1080/00049538508256397
Sonneville, K. R., Horton, N. J., Micali, N., Crosby, R. D., Swanson, S. A., Solmi, F., & Field, A. E. (2013). Longitudinal associations between binge eating and overeating and adverse outcomes among adolescents and young adults: Does loss of control matter? JAMA Pediatrics, 167, 149–155.
Stice, E., & Shaw, H. (2003). Prospective relations of body image, eating, and affective disturbances to smoking onset in adolescent girls: How Virginia slims. Journal of Consulting and Clinical Psychology, 71, 129.
Stice, E., Burton, E. M., & Shaw, H. (2004). Prospective relations between bulimic pathology, depression, and substance abuse: Unpacking comorbidity in adolescent girls. Journal of Consulting and Clinical Psychology, 72, 62.
Treasure, J., Leslie, M., Chami, R., & Fernández-Aranda, F. (2018). Are trans diagnostic models of eating disorders fit for purpose? A consideration of the evidence for food addiction. European Eating Disorders Review, 26, 83–91.
VanderWeele, T. J. (2019). Principles of confounder selection. European Journal of Epidemiology, 34, 211–219.
Vassallo, S., & Sanson, A. (2013). The Australian temperament project: The first 30 years. Melbourne: Australian Institute of Family Studies.
Acknowledgements
The ATP study is located at the Royal Children’s Hospital Melbourne and is a collaboration between Deakin University, the University of Melbourne, the Australian Institute of Family Studies, the University of New South Wales, the University of Otago (New Zealand), La Trobe University and the Royal Children’s Hospital (further information available at https://www.melbournechildrens.com/atp/). We acknowledge all collaborators who have contributed to the ATP, especially Professors Ann Sanson, Margot Prior, Frank Oberklaid, and Dr Diana Smart. We would also like to sincerely thank the participating families for their time and invaluable contribution to the study.
Funding
J.L. (APP1196948) and C.O. (APP1175086) hold National Health and Medical Research Council of Australia Investigator Grants. This work was also supported by the Australian Research Council [DP130101459; DP160103160; DP180102447] and the National Health and Medical Research Council [APP1082406].
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by C.G., P.L., and C.O. The first draft of the manuscript was written by J.L., and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5). Informed consent was obtained from all patients for being included in the study.
Conflict of Interest
The authors declare no competing interests.
Disclaimer
The views expressed in this paper are those of the authors and may not reflect those of their organizational affiliations, nor of other collaborating individuals or organizations.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Primrose Letcher and Craig A. Olsson share joint senior authorship.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Linardon, J., Greenwood, C.J., Macdonald, J.A. et al. Eating and Body Image Disturbances in Adolescence and Substance Use Throughout Young Adulthood: Findings from the Australian Temperament Project. Int J Ment Health Addiction (2023). https://doi.org/10.1007/s11469-023-01023-z
Accepted:
Published:
DOI: https://doi.org/10.1007/s11469-023-01023-z