Abstract
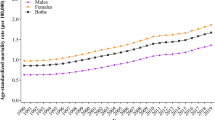
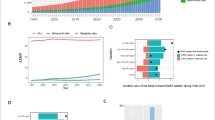
The oldest-old population, those aged ≥ 80 years, is the fastest-growing group in the United States (US), grappling with an increasingly heavy burden of dementia. We aimed to dissect the trends in dementia prevalence, mortality, and risk factors, and predict future levels among this demographic. Leveraging data from the Global Burden of Disease Study 2019, we examined the trends in dementia prevalence, mortality, and risk factors (with a particular focus on body mass index, BMI) for US oldest-old adults. Through decomposition analysis, we identified key population-level contributors to these trends. Predictive modeling was employed to estimate future prevalence and mortality levels over the next decade. Between 1990 and 2019, the number of dementia cases and deaths among the oldest-old in the US increased by approximately 1.37 million and 60,000 respectively. The population growth and aging were highlighted as the primary drivers of this increase. High BMI emerged as a growing risk factor. Females showed a disproportionately higher dementia burden, characterized by a unique risk factor profile, including BMI. Predictions for 2030 anticipate nearly 4 million dementia cases and 160,000 related deaths, with a marked increase in prevalence and mortality anticipated among those aged 80–89. The past 30 years have witnessed a notable rise in both the prevalence and mortality of dementia among the oldest-old in the US, accompanied by a significant shift in risk factors, with obesity taking a forefront position. Targeted age and sex-specific public health strategies that address obesity control are needed to mitigate the dementia burden effectively.




Similar content being viewed by others
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Alzheimer's Association. Alzheimer’s disease facts and figures. Alzheimers Dement. 2019;15:321–387.
Prince M, Bryce R, Albanese E, Wimo A, Ribeiro W, Ferri CP. The global prevalence of dementia: a systematic review and metaanalysis. Alzheimers Dement: J Alzheimers Assoc. 2013;9:63-75.e62.
Xu J, Zhang Y, Qiu C, Cheng F. Global and regional economic costs of dementia: a systematic review. The Lancet. 2017;390:S47.
Hebert LE, Weuve J, Scherr PA, Evans DA. Alzheimer disease in the United States (2010–2050) estimated using the 2010 census. Neurology. 2013;80:1778–83.
Wu Q, Gu D. Oldest-Old Adults. In: Gu D, Dupre ME, editors. Encyclopedia of gerontology and population aging. Cham: Springer International Publishing; 2021. p. 3637–53.
Pierce AL, Kawas CH. Dementia in the oldest old: Beyond Alzheimer disease. PLoS Med. 2017;14:e1002263.
Broyles IH, Li Q, Palmer LM, DiBello M, Dey J, Oliveira I, et al. Dementia’s unique burden: function and health care in the last 4 years of life. J Gerontol A Biol Sci Med Sci. 2023;78:1053–9.
Collaborators GDaI. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet (London, England). 2020;396:1204–22.
GHDx-Link. GBD Results tool. https://vizhub.healthdata.org/gbd-results/. last accessed: 27 June 2023.
GBD 2019 Dementia Forecasting Collaborators. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the Global Burden of Disease Study 2019. The Lancet Public Health. 2022;7:e105–e125.
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet (London, England). 2020;396:1204–1222.
Qin Z, Liu Z, Li R, Luo Y, Wei Z, He L, et al. Association between BMI trajectories in late-middle age and subsequent dementia risk in older age: a 26-year population-based cohort study. BMC Geriatr. 2023;23:773.
Peterson HM, Flaxman AD. Meta-regression with DisMod-MR: how robust is the model? The Lancet. 2013;381:S110.
Aryannejad A, Saeedi Moghaddam S, Mashinchi B, Tabary M, Rezaei N, Shahin S, et al. National and subnational burden of female and male breast cancer and risk factors in Iran from 1990 to 2019: results from the Global Burden of Disease study 2019. Breast Cancer Res. 2023;25:47.
Avan A, Hachinski V. Global, regional, and national trends of dementia incidence and risk factors, 1990–2019: a global burden of disease study. Alzheimers Dement : J Alzheimers Assoc. 2023;19:1281–91.
GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet (London, England). 2020;396:1223–1249.
Mansournia MA, Altman DG. Population attributable fraction. BMJ (Clin Res ed). 2018;360:k757.
Graubard BI, Flegal KM, Williamson DF, Gail MH. Estimation of attributable number of deaths and standard errors from simple and complex sampled cohorts. Stat Med. 2007;26:2639–49.
Riebler A, Held L. Projecting the future burden of cancer: Bayesian age-period-cohort analysis with integrated nested Laplace approximations. Biom J. 2017;59:531–49.
Liu Z, Xu K, Jiang Y, Cai N, Fan J, Mao X, et al. Global trend of aetiology-based primary liver cancer incidence from 1990 to 2030: a modelling study. Int J Epidemiol. 2021;50:128–42.
Cao G, Liu J, Liu M. Global, regional, and national incidence and mortality of neonatal preterm birth, 1990–2019. JAMA Pediatr. 2022;176:787–96.
Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19:335–51.
Cheng X, Yang Y, Schwebel DC, Liu Z, Li L, Cheng P, et al. Population ageing and mortality during 1990–2017: a global decomposition analysis. PLoS Med. 2020;17:e1003138.
Hudomiet P, Hurd MD, Rohwedder S. Trends in inequalities in the prevalence of dementia in the United States. Proc Natl Acad Sci USA. 2022;119:e2212205119.
Langa KM, Larson EB, Crimmins EM, Faul JD, Levine DA, Kabeto MU, et al. A comparison of the prevalence of dementia in the United States in 2000 and 2012. JAMA Intern Med. 2017;177:51–8.
Kramarow EA, Tejada-Vera B. Dementia mortality in the United States, 2000–2017. Natl Vital Stat Rep: Center Dis Control Prev, Natl Center Health Stat, Natl Vital Stat Syst. 2019;68:1–29.
Wetterberg H, Najar J, Rydberg Sterner T, Kern S, Skoog I. The Effect of Diagnostic criteria on dementia prevalence - a population-based study from gothenburg, sweden. The American journal of geriatric psychiatry: Off J Am Assoc Geriatr Psychiatr. 2024;32(2):230–243.
Liu JL, Hlavka JP, Hillestad R, Mattke S. Assessing the preparedness of the U.S. health care system infrastructure for an alzheimer's treatment. Santa Monica, CA: RAND Corporation. https://www.rand.org/content/dam/rand/pubs/research_reports/RR2200/RR2272/RAND_RR2272.pdf. Accessed 10 April 2024.
Lyons B, Watts MOM. Addressing the shortage of direct care workers: insights from seven states (Commonwealth Fund, Mar. 2024). https://doi.org/10.26099/czzn-m038. last accessed: 8 April 2024.
Bullain SS, Corrada MM. Dementia in the oldest old. Continuum (Minneapolis, Minn). 2013;19:457–69.
Rogerson PA, Kim D. Population distribution and redistribution of the baby-boom cohort in the United States: recent trends and implications. Proc Natl Acad Sci USA. 2005;102:15319–24.
Rajan KB, Weuve J, Barnes LL, McAninch EA, Wilson RS, Evans DA. Population estimate of people with clinical Alzheimer’s disease and mild cognitive impairment in the United States (2020–2060). Alzheimers Dement: J Alzheimers Assoc. 2021;17:1966–75.
Boutari C, Mantzoros CS. A 2022 update on the epidemiology of obesity and a call to action: as its twin COVID-19 pandemic appears to be receding, the obesity and dysmetabolism pandemic continues to rage on. Metabolism. 2022;133:155217.
Alexis M. McKee, MD and John E, Morley, MB, BCh. Obesity in the Elderly. https://www.ncbi.nlm.nih.gov/books/NBK532533/. Accessed 10 April 2024.
Percentage of adults aged 65 years or older in the U.S. who were obese from 2013 to 2021. Statista. https://www.statista.com/statistics/720268/elderly-obesity-united-states/. Accessed 10 April 2024
Stokes A, Ni Y, Preston SH. Prevalence and trends in lifetime obesity in the U.S., 1988–2014. Am J Prev Med. 2017;53:567–75.
Anstey KJ, Cherbuin N, Budge M, Young J. Body mass index in midlife and late-life as a risk factor for dementia: a meta-analysis of prospective studies. Obes Rev: Off J Int Assoc Study Obes. 2011;12:e426-437.
Bray GA, Bouchard C. (Eds.). Handbook of Obesity - Volume 2: Clinical Applications 5th ed. CRC Press; 2023. https://doi.org/10.1201/9781003432807
Singh-Manoux A, Dugravot A, Shipley M, Brunner EJ, Elbaz A, Sabia S, et al. Obesity trajectories and risk of dementia: 28 years of follow-up in the Whitehall II Study. Alzheimers Dement. 2018;14:178–86.
Chatterjee S, Peters SA, Woodward M, Mejia Arango S, Batty GD, Beckett N, et al. Type 2 diabetes as a risk factor for dementia in women compared with men: a pooled analysis of 2.3 million people comprising more than 100,000 cases of dementia. Diabetes Care. 2016;39:300–7.
Sierra C. Hypertension and the risk of dementia. Front Cardiovasc Med. 2020;7:5.
Luchsinger JA, Cheng D, Tang MX, Schupf N, Mayeux R. Central obesity in the elderly is related to late-onset Alzheimer disease. Alzheimer Dis Assoc Disord. 2012;26:101–5.
Ntlholang O, McCarroll K, Laird E, Molloy AM, Ward M, McNulty H, et al. The relationship between adiposity and cognitive function in a large community-dwelling population: data from the Trinity Ulster Department of Agriculture (TUDA) ageing cohort study. Br J Nutr. 2018;120:517–27.
Item F, Konrad D. Visceral fat and metabolic inflammation: the portal theory revisited. Obes Rev: Off J Int Assoc Study Obes. 2012;13(Suppl 2):30–9.
Abbatecola AM, Lattanzio F, Spazzafumo L, Molinari AM, Cioffi M, Canonico R, et al. Adiposity predicts cognitive decline in older persons with diabetes: a 2-year follow-up. PLoS One. 2010;5:e10333.
Veronese N, Facchini S, Stubbs B, Luchini C, Solmi M, Manzato E, et al. Weight loss is associated with improvements in cognitive function among overweight and obese people: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2017;72:87–94.
Balasubramanian P, Kiss T, Tarantini S, Nyul-Toth A, Ahire C, Yabluchanskiy A, et al. Obesity-induced cognitive impairment in older adults: a microvascular perspective. Am J Physiol Heart Circ Physiol. 2021;320:H740–61.
Baumgart M, Snyder HM, Carrillo MC, Fazio S, Kim H, Johns H. Summary of the evidence on modifiable risk factors for cognitive decline and dementia: a population-based perspective. Alzheimers Dement: J Alzheimers Assoc. 2015;11:718–26.
Ungvari Z, Toth P, Tarantini S, Prodan CI, Sorond F, Merkely B, et al. Hypertension-induced cognitive impairment: from pathophysiology to public health. Nat Rev Nephrol. 2021;17:639–54.
Rusanen M, Kivipelto M, Quesenberry CP Jr, Zhou J, Whitmer RA. Heavy smoking in midlife and long-term risk of Alzheimer disease and vascular dementia. Arch Intern Med. 2011;171:333–9.
Ohara T, Ninomiya T, Hata J, Ozawa M, Yoshida D, Mukai N, et al. Midlife and late-life smoking and risk of dementia in the community: the Hisayama study. J Am Geriatr Soc. 2015;63:2332–9.
Crane PK, Walker R, Hubbard RA, Li G, Nathan DM, Zheng H, et al. Glucose levels and risk of dementia. N Engl J Med. 2013;369:540–8.
Choi D, Choi S, Park SM. Effect of smoking cessation on the risk of dementia: a longitudinal study. Ann Clin Transl Neurol. 2018;5:1192–9.
Campbell JM, Stephenson MD, de Courten B, Chapman I, Bellman SM, Aromataris E. Metformin use associated with reduced risk of dementia in patients with diabetes: a systematic review and meta-analysis. J Alzheimers Dis: JAD. 2018;65:1225–36.
AreosaSastre A, Vernooij RW, González-ColaçoHarmand M, Martínez G. Effect of the treatment of type 2 diabetes mellitus on the development of cognitive impairment and dementia. Cochrane Database Syst Rev. 2017;6:003804.
Rosenberg A, Ngandu T, Rusanen M, Antikainen R, Bäckman L, Havulinna S, et al. Multidomain lifestyle intervention benefits a large elderly population at risk for cognitive decline and dementia regardless of baseline characteristics: the FINGER trial. Alzheimers Dement: J Alzheimers Assoc. 2018;14:263–70.
Sindi S, Solomon A, Kåreholt I, Hovatta I, Antikainen R, Hänninen T, et al. Telomere length change in a multidomain lifestyle intervention to prevent cognitive decline: a randomized clinical trial. J Gerontol A Biol Sci Med Sci. 2021;76:491–8.
Plassman BL, Langa KM, Fisher GG, Heeringa SG, Weir DR, Ofstedal MB, et al. Prevalence of dementia in the United States: the aging, demographics, and memory study. Neuroepidemiology. 2007;29:125–32.
Eikelboom WS, Pan M, Ossenkoppele R, Coesmans M, Gatchel JR, Ismail Z, et al. Sex differences in neuropsychiatric symptoms in Alzheimer’s disease dementia: a meta-analysis. Alzheimers Res Ther. 2022;14:48.
Eastman J, Bahorik A, Kornblith E, Xia F, Yaffe K. Sex differences in the risk of dementia in older veterans. J Gerontol A Biol Sci Med Sci. 2022;77:1250–3.
Bagit A, Hayward GC, MacPherson REK. Exercise and estrogen: common pathways in Alzheimer’s disease pathology. Am J Physiol Endocrinol Metab. 2021;321:E164–8.
Jett S, Malviya N, Schelbaum E, Jang G, Jahan E, Clancy K, et al. Endogenous and exogenous estrogen exposures: how women’s reproductive health can drive brain aging and inform Alzheimer’s prevention. Front Aging Neurosci. 2022;14:831807.
Valencia-Olvera AC, Maldonado Weng J, Christensen A, LaDu MJ, Pike CJ. Role of estrogen in women’s Alzheimer’s disease risk as modified by APOE. J Neuroendocrinol. 2023;35:e13209.
Zhao L, Woody SK, Chhibber A. Estrogen receptor beta in Alzheimer’s disease: from mechanisms to therapeutics. Ageing Res Rev. 2015;24:178–90.
Nguyen DH, Cunningham JT, Sumien N. Estrogen receptor involvement in vascular cognitive impairment and vascular dementia pathogenesis and treatment. Geroscience. 2021;43:159–66.
Deer RR, Stallone JN. Effects of estrogen on cerebrovascular function: age-dependent shifts from beneficial to detrimental in small cerebral arteries of the rat. Am J Physiol Heart Circ Physiol. 2016;310:H1285-1294.
Davezac M, Buscato M, Zahreddine R, Lacolley P, Henrion D, Lenfant F, et al. Estrogen receptor and vascular aging. Front Aging. 2021;2:727380.
Malpetti M, Sala A, Vanoli EG, Gianolli L, Luzi L, Perani D. Unfavourable gender effect of high body mass index on brain metabolism and connectivity. Sci Rep. 2018;8:12584.
Li R, Li R, Xie J, Chen J, Liu S, Pan A, et al. Associations of socioeconomic status and healthy lifestyle with incident early-onset and late-onset dementia: a prospective cohort study. The Lancet Healthy Longev. 2023;4:e693–702.
Li C, Hua R, Gao D, Zheng F, Xie W. Cognitive decline before and during COVID-19 pandemic among older people with multimorbidity: a longitudinal study. J Am Med Dir Assoc. 2023;24:419-425.e410.
Owens CD, Bonin Pinto C, Mukli P, Szarvas Z, Peterfi A, Detwiler S, et al. Vascular mechanisms leading to progression of mild cognitive impairment to dementia after COVID-19: protocol and methodology of a prospective longitudinal observational study. PLoS One. 2023;18:e0289508.
Kirkpatrick A, Delpirou NC, Husain F, Xu C, Vincent A, Yabluchanskiy A, et al. MCI patients with COVID-19 have increased progression to dementia at 18 months (S39. 010). Neurology. 2023;100.
Matsuzono K, Mashiko T, Anan Y, Koide R, Yoshizumi H, Fujimoto S. Impact of COVID-19 pandemic on mortality and cognitive function of dementia patients: Tochigi Dementia Cohort Study. J Neurol Sci. 2024;456:122840.
Acknowledgements
We appreciate the works by the Global Burden of Disease Study 2019.
Funding
This work was supported by the National Natural Science Foundation of China (grant number 82103727), the fellowship of China Postdoctoral Science Foundation (grant number 2021M702221), Guangdong Basic and Applied Basic Research Foundation (grant number 2022A1515010957), Shenzhen Science and Technology Program (grant number RCBS20210706092408008), the National Research, Development and Innovation Fund of Hungary (grant number TKP2021-NKTA-47), the National Cardiovascular Laboratory Program (grant number RRF-2.3.1–21-2022–00003), the National Research, Development and Innovation Fund of Hungary K_20 funding scheme (grant number 135784), the National Research, Development and Innovation Fund of Hungary New National Excellence Program of the Ministry for Innovation and Technology (grant number ÚNKP-24–3-II-SE-14), and the European University for Well-Being (EUniWell) program (grant number 101004093/ EUniWell/EAC-A02-2019 / EAC-A02-2019–1). The funding sources had no role in the writing of the manuscript; and in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
Conceptualization: XC, YG, and VFP. Data acquisition: YG, MW, and YM. Data analysis: YG, MZ, YM. Data interpretation: XC, MW, and YG. Drafting manuscript: XC, VFP, YG. Revising manuscript: MW, MZ, YM, DM, AL, and YG. Approving final version of the manuscript: All authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Cao, X., Wang, M., Zhou, M. et al. Trends in prevalence, mortality, and risk factors of dementia among the oldest-old adults in the United States: the role of the obesity epidemic. GeroScience (2024). https://doi.org/10.1007/s11357-024-01180-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11357-024-01180-6