Abstract
Recent studies have linked ambient air pollution to depression. Anhedonia is a core symptom of depression which severely impacts on prognosis. The present study aims to investigate the association of PM2.5 and PM10 exposure with anhedonia in depressed patients. A total of 538 patients with depression who were hospitalized at the Fourth People’s Hospital of Hefei between June 2017 and December 2021 were included. We estimated ambient particulate matters exposure, including PM2.5 and PM10, using a satellite-based spatiotemporal model at a resolution of 1 km2. The revised Physical Anhedonia Scale (RPAS) and the revised Social Anhedonia Scale (RSAS) were evaluated. The association of ambient particulate matters and anhedonia was examined using multiple linear regression models, adjusted for potential confounders. We observed that exposure to PM2.5 were significantly associated with increased RSAS score and RPAS score, with the major effect in the 12-month exposure window (β = 1.238; 95%CI, 0.353, 2.123) and 18-month exposure window (β = 1.888; 95%CI, 0.699, 3.078), respectively. Meanwhile, PM10 levels were also significantly associated with increased RSAS score and RPAS score, with the major effect in the 18-month exposure window (β = 1.220; 95%CI, 0.439, 2) and 3-month exposure window (β = 1.602; 95%CI, 0.062, 3.143), respectively. Subgroup analysis showed that both PM2.5 and PM10 were significantly associated with anhedonia in females, patients < 40 years old, low family income group, and those who had a higher educational level. Our study suggests that long-term PM2.5 and PM10 exposure are associated with more severe anhedonia in patients with depression. These associations were different in subgroup by age, gender, family income, and educational level.
Similar content being viewed by others
Introduction
Depression is a worldwide health problem that can lead to disability, functional decline, and an elevated risk of suicide (Friedrich 2017). Epidemiological evidence suggests that 4.4% of the global population suffers from depression, which is ranked as the single largest contributor to non-fatal health loss (7.5% of all years lived with disability [YLDs]) (World Health Organization 2018). In China, the annual prevalence of depression is 6.8%, and the lifetime prevalence is 3.6% (Huang et al. 2019). Anhedonia, a diminished motivation and sensitivity to pleasurable stimuli, is a core clinical symptom of depression (Berrios and Olivares 1995, American Psychiatry Organization 2013). Up to 70% of patients with depression experience significant anhedonia, which severely impairs not only their social functioning but also their cognitive abilities (McIntyre et al. 2016). Anhedonia also becomes a prominent residual symptom in some patients after clinical cure and even leads to refractory depression (Ely et al. 2021). Thus, the identification of modifiable risk factors for anhedonia is needed to provide potential prevention and control.
Air pollution contains many individual pollutants, including particulate matter (PM), gaseous pollutants, and metallic and organic compounds (Liu et al. 2023; Wang et al. 2023). PM is the most widespread health threat which may cause increased risk of mortality (Silva et al. 2013), cancer (Christiani 2021), respiratory disease (Jung et al. 2017), and cardiorespiratory diseases (Katsoulis et al. 2014). Recent studies show that air pollution (particulate matter) may interfere with the normal structure and function of the brain with long-lasting effects on mental health, particularly both depressive symptoms and depressive disorders (Fan et al. 2020; Rautio et al. 2018). A meta-analysis reported that long-term exposure to particulate matter exposure with an aerodynamic diameter < 2.5 µm (PM2.5) to ambient air pollution is associated with an augmented risk of depression (Braithwaite et al. 2019). Wang et al. (2020) found that exposure to PM2.5 increases depressive symptoms in older Chinese adults. Zhang et al. (2019) found a positive association between 12- and 60-month PM10 exposure and the developing depression. Lim et al. (2012) evaluated data from 537 elderly adults in Korea and reported that emotional symptoms were more likely to be associated with air pollution exposure than somatic and affective symptoms. Niedzwiecki et al. (2020) found that particulate matter exposure during pregnancy is positively associated with PPD and symptoms of anhedonia and depression at 6 months postpartum. However, the relationships between anhedonia and ambient particulate matters in depressed patients remain unclear.
In this cross-sectional study, we leverage a sample of participants with depression to examine the specific association of ambient particulate matter (PM2.5, PM10) exposure to anhedonia and to investigate the existence of susceptible subgroups.
Materials and methods
Study design and participants
Five hundred sixty-two patients were recruited from Hefei Fourth People’s Hospital, Hefei, China, in 2017 to 2021. All patients were assessed by the Mini-International Neuropsychiatric Interview (MINI) 6.0.0 to confirm the diagnosis of major depressive disorders (MDD). Structured questionnaires were administered by all participants and were used to record sociodemographic characteristics, lifestyle, and depressive symptoms. Ground PM2.5 and PM10 concentration and satellite AOD data were obtained from 2017 to 2021 according to each participant’s residential address.
Participants were enrolled as the following criteria: (1) diagnosis of MDD according to Diagnosis and Statistical Manual-5th edition (DSM-V), (2) Han Chinese ethnicity, (3) age 18–65 years, (4) be able to cooperate in completing questionnaires. The exclusion criteria were as follows: (1) other concurrent psychiatric disorders defined in the DSM-V such as schizophrenia and substance use disorders, (2) and current severe physical conditions (e.g., neurological diseases, malignancy, cardiovascular diseases, respiratory diseases, severe trauma, state of pregnancy, or breastfeeding), (3) moved in the last 2 years. After the strict clinical screening, we excluded 40 depressed patients, among whom 18 patients missed information on anhedonia and address, 12 patients moved in the last 2 years, and 8 patients diagnosed with cardiovascular diseases or respiratory diseases. The final analyses included 538 depressed patients.
All subjects received and signed informed consent forms prior to enrollment, and this study was approved by the Ethics Committee of Anhui Mental Health Center (AMHC).
Exposure measurements
Exposure to PM2.5 and PM10 was estimated at each participant’s address, which was reported in the questionnaire coordinates and geocoded into latitude and longitude data. A satellite-based spatiotemporal model with a high spatial resolution of 1 × 1 km on the basis of National Aeronautics and Space Administration (NASA) aerosol optical thickness (AOD) data were used to estimate ambient PM2.5 and PM10 concentrations. And we used 1 month, 3 months, 6 months, 12 months, 18 months, and 24 months before the survey day as exposure windows.
Clinical assessments
Revised Social Anhedonia Scale (RSAS)
Social anhedonia is defined as an impaired ability to feel pleasure in the interpersonal domain, and the Chinese version of the revised social anhedonia scale is a 40-item self-assessment questionnaire with a total score of 0 to 40, with higher scores indicating a more severe social anhedonia. The items are scored relative to standard answers. Items requiring reverse scoring are “False,” and items not requiring reverse scoring are “True” based on the standard answer. An item is scored as a “1” if the response to the item is consistent with the standard answer for that item; otherwise, it is scored as a “0.” The total score is the sum of the scores for each item. A series of studies have shown that it has a high excellent coefficient (Hu et al. 2018).
Revised Physical Anhedonia Scale (RPAS)
The RPAS is a 61-item self-rated questionnaire to assess whether participants can experience physical satisfaction from typical pleasurable stimuli such as food and situations, and each item is scored in the same way as the RSAS. The total score is the sum of the scores for each item. This psychometric scale provides a reliable and valid measure for patients with depression (Kollias et al. 2008).
Hamilton Depression Scale (HAMD24)
This is the most commonly used scale worldwide to assess the severity of depression with high reliability and validity. The HAMD24 has 24 items. Most of the HAMD24 items (item 1, 2, 3, 7, 8, 9, 10, 11, 15, 19, 20, 22, 23, 24) are scored on a scale of 0–4 according to the severity of each symptom. The total score is the sum of the scores for each item. Other items are scored on a scale of 0–2. Score higher than 8 in HAMD24 indicates the presence of depressive symptoms (Hamilton 1967).
Hamilton Anxiety Rating Scale (HAMA)
HAMA consists of 14 entries and two factor categories: somatic anxiety (7, 8, 9, 10, 11, 12, and 13 entries) and psychiatric anxiety (1, 2, 3, 4, 5, 6, and 14 entries), depending on the severity of each symptom using a 0 to 4 scoring method. The total score is the sum of the scores for each item. Score higher than 7 indicates the presence of anxiety symptoms. The scale was developed by Hamilton in 1959 and has been widely used to assess anxiety symptoms with good validity and reliability (Zimmerman et al. 2017).
Covariates
In addition to clinical assessments, we controlled for potential confounding covariates in the analysis. The following covariates were included in data analysis: age (years), gender (male and female), educational level (middle school or below, high school or above), smoking status (non-smoker, smoker), alcohol drinking (non-drinker, drinker), the frequency of physical activity in the past 1 month (sedentary, 1–2 times/week, 3–5 time/week, > 6 time/week), use of antidepressants in the past 1 month (“yes,” “no”), season of visit, and family income (< 4000 RMB, ≥ 4000 RMB). Body mass index (BMI) was calculated as weight in kilograms divided by squared height in meters.
Statistical analysis
Continuous variables were presented as mean ± standard deviation if distributed normally, or expressed as medians (interquartile ranges) if distributed skewed. Categorical variables were presented as frequency (percentage). And we used multiple linear regression models to investigate the association between PM2.5 and PM10 on anhedonia among all study participants. The measure of variance inflation factors (VIFs < 2) was used to avoid the multicollinearity among the variables (Yu et al. 2022). Model 1 adjusted for age, sex, educational level, family income, and employment; Model 2 further adjusted for BMI, smoking status, drinking status, and physical activity; Model 3 further adjusted for season of visit and use of antidepressants. All results were expressed as changes in RSAS and RPAS score associated with an IQR increase in exposure and corresponding 95% confidence intervals (CI). To analyze the effect of different ambient particulate matters exposure windows, we calculated 1-month, 3-month, 6-month, 12-month, 18-month, and 24-month average levels. Subgroup analyses were conducted stratified by gender, age, and family income. All analyses were performed using the R software (version 3.6.0, R Foundation for Statistical Computing).
Result
General characteristics
Table 1 shows characteristics of the study population. The mean age of the study population was 41.2 years (standard deviation [SD] = 13.1) with 68% females. 43.5% of the study population had high school or above educational status, and the mean BMI is 22.7 kg/m2 (SD = 3.2). As for the smoking and drinking status, 15.2% and 9.8% of participants were smokers and alcohol drinkers. Fig. S1 showed the distribution of 538 participants in 16 cities from Anhui province of China. One-month, 3-month, 6-month, 12-month, 18-month, and 24-month average concentrations with the median and IQR of air pollution among study participants are shown in Table S1.
Associations between ambient particulate matters and anhedonia
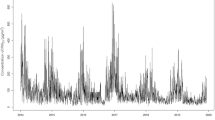
Figure 1 shows the adjusted associations between different exposures to ambient particulate matters. We observed that PM2.5 levels for the 6-month, 12-month, 18-month, and 24-month exposure windows were significantly associated with RSAS score in Model 3, with the major effect in the 12-month exposure window (β = 1.238; 95%CI, 0.353, 2.123). As for PM2.5 and RPAS score, PM2.5 exposure for the 3-month, 6-month, 12-month, 18-month, and 24-month windows were significantly associated with RPAS score in fully adjusted model, with the major effect in the 18-month exposure window (β = 1.888; 95%CI, 0.699, 3.078). For PM10 and RSAS score, the significant exposure windows were the 3 months, 6 months, 12 months, 18 months, and 24 months, with the major effect in the 18-month exposure window (β = 1.220; 95%CI, 0.439, 2). And in regard to PM10 and RPAS score, after fully adjusted, IQR increases in PM10 levels for the 3-month (β = 1.602; 95%CI, 0.062, 3.143), 6-month (β = 1.466; 95%CI, 0.288, 2.704), 12-month (β = 1.218; 95%CI, 0.120, 2.442), and 18-month (β = 1.390; 95%CI, 0.172, 2.608) exposure windows were, respectively, associated with RPAS score.
Adjusted change (95% confidence interval (CI)) of RSAS and RPAS scores for an interquartile range (IQR) change in ambient particulate matters (N = 538). Notes: *p < 0.05, **p < 0.01. Abbreviations: CI, confidence interval; IQR, interquartile range; PM2.5, particulate matter with aerodynamic diameter ≤ 2.5 µm; PM10, particulate matter with aerodynamic diameter ≤ 10 µm. Model 1 is adjusted for age, sex, educational level, family income, and employment. Model 2 further adjusted BMI, smoking status, drinking status, and physical activity on the basis of Model 1. Model 3 further adjusted season of visit and use of antidepressants on the basis of Model 2
Subgroup analyses
In subgroup analysis, the effect size of exposure to PM2.5 and PM10 on RSAS and RPAS score was significantly higher among those who were female or younger than 40 years old. We also found the association between ambient particulate matters and anhedonia would be stronger in participants who had a lower family income and a higher educational level (Figs. 2 and 3).
Subgroup analysis for the association between 12-month exposure to ambient particulate matters and RSAS scores. Notes: All results were adjusted for age, sex, educational level, family income, employment, BMI, smoking status, drinking status, physical activity, season of visit, and use of antidepressants. Notes: *p < 0.05, **p < 0.01. Abbreviations: CI, confidence interval; PM2.5, particulate matter with aerodynamic diameter ≤ 2.5 µm; PM10, particulate matter with aerodynamic diameter ≤ 10 µm
Subgroup analysis for the association between 12-month exposure to ambient particulate matters and RPAS scores. Notes: All results were adjusted for age, sex, educational level, family income, employment, BMI, smoking status, drinking status, physical activity, season of visit, and use of antidepressants. Notes: *p < 0.05, **p < 0.01. Abbreviations: CI, confidence interval; PM2.5, particulate matter with aerodynamic diameter ≤ 2.5 µm; PM10, particulate matter with aerodynamic diameter ≤ 10 µm
Discussion
In the present study, we found that RSAS and RPAS score was associated with increased exposure to ambient particulate matters such as PM2.5 and PM10 in depressed patients after adjusting for potential confounders. Stronger associations were estimated among female, patients < 40 years old, low family income group, and those who had a higher educational level. Our results indicate that anhedonia in depressed patients was positively associated with PM2.5 and PM10 exposure, and female, patients < 40 years old, low family income group, and those who had a higher educational level were more susceptible to PM exposure.
This study initially found a positive association between environmental particulate matter and anhedonia in patients with depression. Despite few studies on ambient particulate matters exposure and anhedonia, two studies conducted among pregnant women showed similar results. Results from a birth cohort in Mexico City (509 mothers with available data) suggest that particulate matter exposure during pregnancy is positively associated with PPD and symptoms of anhedonia and depression at 6 months postpartum (Niedzwiecki et al. 2020). Another study from the USA found that increased PM2.5 exposure in mid-pregnancy was associated with increased depressive and anhedonia symptoms (Sheffield et al. 2018). Mechanistic data indicates that inflammation may be a pathophysiologic pathway to anhedonia. Felger et al. (2017) found that inflammatory stimuli reduce neural activity and dopamine release in reward-related brain regions in association with reduced motivation and anhedonia. And increasing evidence suggests that inflammation may mediate the relationship between air pollution and anhedonia. Hogan et al. (2015) reported that PM2.5 exposure could trigger depression-like responses (anhedonia) in mice through upregulates neuroinflammatory cytokines and altering structural changes in the CA1 hippocampus. Future studies are needed to further explore the potential mechanism linking air pollution and anhedonia. However, results from MOBILIZE Boston Study found no evidence of a positive association between long-term exposure to PM2.5 and depressive symptoms using the Revised Center for Epidemiological Studies Depression Scale (CESD-R) in older adults (Wang et al. 2014). One possible reason is that CESD-R items do not measure the diagnostic criteria of anhedonia (Smarr and Keefer 2011). A study from the French CONSTANCES cohort suggests that the relationship between air pollution and depressive symptoms is not fully explained by somatic symptoms (Zare Sakhvidi et al. 2022). Additional studies about air pollution and different dimensions of depressive symptoms in human cohorts are warranted.
Notably, the present study found that longer-term cumulative air pollution exposure was significantly associated with anhedonia, but the result was not found in the short term. Similar results were found in a Scottish study assessing the relationship between air pollution and mortality, in which Beverland et al. (2012) compared associations between short-term exposure to black smoke (BS) and mortality with long-term exposure-mortality associations in two cohorts and the results showed that short-term exposure-mortality associations were substantially lower than equivalent long-term associations.. The difference in the magnitude of the effects between long-term and short-term exposures may be due to the greater and more persistent cumulative effects of long-term exposures.
In subgroup analysis, interestingly, we observe stronger associations between anhedonia and PM exposure among female, patients < 40 years old, low family income group, and those who had a higher educational level. Previous studies have shown that particulate matter exposure risks are higher for women than for men (Bell et al. 2013), which may be attributed to differences in life stage, co-exposures, hormonal status, or other factors (Clougherty 2011). As in our study, higher susceptibility of individuals younger than 40 years old of ambient air pollution exposure on anhedonia has been reported. A recent study from Canada found that the negative effect of air pollution on depressed mood may be greater in younger people (Szyszkowicz and Rowe 2014), and this discrepancy may result from different indoor/outdoor activity patterns and occupational exposures. The impact of education on particulate matter-associated risks is controversial. In our study, subgroup analyses showed few significant associations in participants with low education. Filleul et al. (2004) found greater associations between particles and mortality among the more highly educated. But Martins et al. (2004) reported that the effect of particulate matters was negatively correlated with percentage of people with college education. One possible explanation of our finding is that residential groups by educational level may lead to differences in exposure to particulate matter of different source and component. In addition, our results suggested that the relationship between ambient particulate matters and anhedonia was more significant in the low-income groups were all higher than in high-income groups. This finding is consistent with the finding of a recent meta-analysis (Bell et al. 2013), which may be due to the difference in personal self-protection strategies against air pollution (Carlsten et al. 2020).
Our study had several strengths. First, to the best of our knowledge, this is the first study to investigate associations between anhedonia among depressed patients and air pollution after controlling for individual effects. Most of our patients were in severe depression; the diagnoses were based on semi-structured interview kit. Second, PM2.5 and PM10 exposure were assessed accurately using high-performance satellite-based technology with a high spatial resolution of 1 km2. We also acknowledge some limitations. First, the sample size in this clinical research is relatively smaller; future studies should target on larger-sized cohorts of depressive patients. Second, anhedonia was assessed using only the RSAS and RPAS. The stages of reward processing were not assessed (e.g., motivation, consumption-based anhedonia). Third, other confounding factors that may affect the estimation effect such as traffic noise and surrounding green space have not been considered, but it remains unknown to what extent these factors would affect our findings. Future studies could further explore the association between other environmental exposures and anhedonia. Lastly, we did not measure levels of indoor air pollution. Levels of PM2.5 and PM10 were estimated at the home addresses of the participants. Although we took into account the confounding factor of smoking which is one of the important components of indoor PM2.5 sources, it may not accurately reflect actual personal exposure. Future studies may better use personal exposure data for health-related exploration.
Conclusion
This is the first report to investigate the relationship between anhedonia among depressive patients and air pollution. The results of this study showed that exposure to PM2.5 and PM10 was significantly associated with anhedonia in patients with depressive disorders. In addition, we found that female, younger people (< 40 years old), and those with lower family income and higher educational level were more vulnerable to PM2.5 and PM10. This study provides clinical evidence to elucidate the etiological pathway of air pollution on depressive orders and also reference for the public health sector in the prevention and treatment of refractory depression.
Data availability
The data sets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
American Psychiatry Association (2013) Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
Bell ML, Zanobetti A, Dominici F (2013) Evidence on vulnerability and susceptibility to health risks associated with short-term exposure to particulate matter: a systematic review and meta-analysis. Am J Epidemiol 178:865–876. https://doi.org/10.1093/aje/kwt090
Berrios GE, Olivares JM (1995) The anhedonias: a conceptual history. Hist Psychiatry 6:453–470. https://doi.org/10.1177/0957154x9500602403
Beverland IJ, Cohen GR, Heal MR, Carder M, Yap C, Robertson C, Hart CL, Agius RM (2012) A comparison of short-term and long-term air pollution exposure associations with mortality in two cohorts in Scotland. Environ Health Perspect 120:1280–1285. https://doi.org/10.1289/ehp.1104509
Braithwaite I, Zhang S, Kirkbride JB, Osborn DPJ, Hayes JF (2019) Air pollution (particulate matter) exposure and associations with depression, anxiety, bipolar, psychosis and suicide risk: a systematic review and meta-analysis. Environ Health Perspect 127:126002. https://doi.org/10.1289/ehp4595
Carlsten C, Salvi S, Wong GWK, Chung KF (2020) Personal strategies to minimise effects of air pollution on respiratory health: advice for providers, patients and the public. Eur Respir J 55. https://doi.org/10.1183/13993003.02056-2019
Christiani DC (2021) Ambient air pollution and lung cancer: nature and nurture. Am J Respir Crit Care Med 204:752–753. https://doi.org/10.1164/rccm.202107-1576ED
Clougherty JE (2011) A growing role for gender analysis in air pollution epidemiology. Cienc Saude Colet 16:2221–2238. https://doi.org/10.1590/s1413-81232011000400021
Ely BA, Nguyen TNB, Tobe RH, Walker AM, Gabbay V (2021) Multimodal investigations of reward circuitry and anhedonia in adolescent depression. Front Psychiatry 12:678709. https://doi.org/10.3389/fpsyt.2021.678709
Fan SJ, Heinrich J, Bloom MS, Zhao TY, Shi TX, Feng WR, Sun Y, Shen JC, Yang ZC, Yang BY, Dong GH (2020) Ambient air pollution and depression: a systematic review with meta-analysis up to 2019. Sci Total Environ 701:134721. https://doi.org/10.1016/j.scitotenv.2019.134721
Felger JC, Treadway MT (2017) Inflammation effects on motivation and motor activity: role of dopamine. Neuropsychopharmacol: Off Publ Am Coll Neuropsychopharmacol 42:216–241. https://doi.org/10.1038/npp.2016.143
Filleul L, Rondeau V, Cantagrel A, Dartigues JF, Tessier JF (2004) Do subject characteristics modify the effects of particulate air pollution on daily mortality among the elderly? J Occup Environ Med 46:1115–1122. https://doi.org/10.1097/01.jom.0000144998.82543.9d
Friedrich MJ (2017) Depression is the leading cause of disability around the world. JAMA 317:1517. https://doi.org/10.1001/jama.2017.3826
Hamilton M (1967) Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol 6:278–296. https://doi.org/10.1111/j.2044-8260.1967.tb00530.x
Hogan MK, Kovalycsik T, Sun Q, Rajagopalan S, Nelson RJ (2015) Combined effects of exposure to dim light at night and fine particulate matter on C3H/HeNHsd mice. Behav Brain Res 294:81–88. https://doi.org/10.1016/j.bbr.2015.07.033
Hu HX, Chu MY, Yang Y, Wang LL, Zhang RT, Lui SSY, Cheung EFC, Chan RCK (2018) Mediation effect of beliefs about pleasure and emotional experience between social anhedonia and prediction of pleasant events. Psychiatry Res 264:39–45. https://doi.org/10.1016/j.psychres.2018.03.070
Huang Y et al (2019) Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry 6:211–224. https://doi.org/10.1016/s2215-0366(18)30511-x
Jung KH, Torrone D, Lovinsky-Desir S, Perzanowski M, Bautista J, Jezioro JR, Hoepner L, Ross J, Perera FP, Chillrud SN, Miller RL (2017) Short-term exposure to PM(2.5) and vanadium and changes in asthma gene DNA methylation and lung function decrements among urban children. Respir Res 18:63. https://doi.org/10.1186/s12931-017-0550-9
Katsoulis M, Dimakopoulou K, Pedeli X, Trichopoulos D, Gryparis A, Trichopoulou A, Katsouyanni K (2014) Long-term exposure to traffic-related air pollution and cardiovascular health in a Greek cohort study. Sci Total Environ 490:934–940. https://doi.org/10.1016/j.scitotenv.2014.05.058
Kollias CT, Kontaxakis VP, Havaki-Kontaxaki BJ, Stamouli S, Margariti M, Petridou E (2008) Association of physical and social anhedonia with depression in the acute phase of schizophrenia. Psychopathology 41:365–370. https://doi.org/10.1159/000152378
Lim YH, Kim H, Kim JH, Bae S, Park HY, Hong YC (2012) Air pollution and symptoms of depression in elderly adults. Environ Health Perspect 120:1023–1028. https://doi.org/10.1289/ehp.1104100
Liu W, Yu L, Zhou M, Ye Z, Liang R, Tan Q, Song J, Ma J, Wang D, Wang B, Chen W (2023) Cross-sectional and longitudinal associations between propylene oxide exposure and lung function among Chinese community residents: roles of oxidative DNA damage, lipid peroxidation, and protein carbonylation. Chest 163:1395–1409. https://doi.org/10.1016/j.chest.2022.12.004
Martins MC, Fatigati FL, Véspoli TC, Martins LC, Pereira LA, Martins MA, Saldiva PH, Braga AL (2004) Influence of socioeconomic conditions on air pollution adverse health effects in elderly people: an analysis of six regions in São Paulo, Brazil. J Epidemiol Community Health 58:41–46. https://doi.org/10.1136/jech.58.1.41
McIntyre RS, Woldeyohannes HO, Soczynska JK, Maruschak NA, Wium-Andersen IK, Vinberg M, Cha DS, Lee Y, Xiao HX, Gallaugher LA, Dale RM, Alsuwaidan MT, Mansur RB, Muzina DJ, Carvalho AF, Jerrell JM, Kennedy SH (2016) Anhedonia and cognitive function in adults with MDD: results from the International Mood Disorders Collaborative Project. CNS Spectr 21:362–366. https://doi.org/10.1017/s1092852915000747
Niedzwiecki MM, Rosa MJ, Solano-González M, Kloog I, Just AC, Martínez-Medina S, Schnaas L, Tamayo-Ortiz M, Wright RO, Téllez-Rojo MM, Wright RJ (2020) Particulate air pollution exposure during pregnancy and postpartum depression symptoms in women in Mexico City. Environ Int 134:105325. https://doi.org/10.1016/j.envint.2019.105325
Rautio N, Filatova S, Lehtiniemi H, Miettunen J (2018) Living environment and its relationship to depressive mood: a systematic review. Int J Soc Psychiatry 64:92–103. https://doi.org/10.1177/0020764017744582
Sheffield PE, Speranza R, Chiu YM, Hsu HL, Curtin PC, Renzetti S, Pajak A, Coull B, Schwartz J, Kloog I, Wright RJ (2018) Association between particulate air pollution exposure during pregnancy and postpartum maternal psychological functioning. PLoS ONE 13:e0195267. https://doi.org/10.1371/journal.pone.0195267
Silva RA, West JJ, Zhang Y, Anenberg SC, Lamarque JFO, Shindell DT, Collins WJ, Dalsoren S, Faluvegi G, Folberth G (2013) Global premature mortality due to anthropogenic outdoor air pollution and the contribution of past climate change. Environ Res Lett 8:034005. https://doi.org/10.1088/1748-9326/8/3/034005
Smarr KL, Keefer AL (2011) Measures of depression and depressive symptoms: Beck Depression Inventory-II (BDI-II), Center for Epidemiologic Studies Depression Scale (CES-D), Geriatric Depression Scale (GDS), Hospital Anxiety and Depression Scale (HADS), and Patient Health Questionnaire-9 (PHQ-9). Arthritis Care Res 63(Suppl 11):S454–S466. https://doi.org/10.1002/acr.20556
Szyszkowicz M, Rowe BH (2014) Ambient air pollution and depressive symptoms. PeerJ. https://doi.org/10.7287/peerj.preprints.757v1
Wang Y, Eliot MN, Koutrakis P, Gryparis A, Schwartz JD, Coull BA, Mittleman MA, Milberg WP, Lipsitz LA, Wellenius GA (2014) Ambient air pollution and depressive symptoms in older adults: results from the MOBILIZE Boston study. Environ Health Perspect 122:553–558. https://doi.org/10.1289/ehp.1205909
Wang R, Yang B, Liu P, Zhang J, Liu Y, Yao Y, Lu Y (2020) The longitudinal relationship between exposure to air pollution and depression in older adults. Int J Geriatr Psychiatry 35:610–616. https://doi.org/10.1002/gps.5277
Wang B, Liu W, Yu L, Ye Z, Cheng M, Qiu W, Zhou M, Ma J, Wang X, Yang M, Song J, Chen W (2023) Acrolein exposure impaired glucose homeostasis and increased risk of type 2 diabetes: an urban adult population-based cohort study with repeated measures. Environ Sci Technol 57:7162–7173. https://doi.org/10.1021/acs.est.2c09299
World Health Organization (2018) Depression and other common mental disorders: global health estimate. http://apps.who.int/iris/bitstream/handle/10665/254610/WHO-MSD-MER-2017.2-eng.pdf;jsessionid=9AFDFABE4DFBCB868100C34A39B99CC8?sequence=1. Accesed 16 Sept 2018
Yu L, Liu W, Wang X, Ye Z, Tan Q, Qiu W, Nie X, Li M, Wang B, Chen W (2022) A review of practical statistical methods used in epidemiological studies to estimate the health effects of multi-pollutant mixture. Environ Pollut 306:119356. https://doi.org/10.1016/j.envpol.2022.119356. (Barking, Essex : 1987)
Zare Sakhvidi MJ, Lafontaine A, Lequy E, Berr C, de Hoogh K, Vienneau D, Goldberg M, Zins M, Lemogne C, Jacquemin B (2022) Ambient air pollution exposure and depressive symptoms: findings from the French CONSTANCES cohort. Environ Int 170:107622. https://doi.org/10.1016/j.envint.2022.107622
Zhang Z, Zhao D, Hong YS, Chang Y, Ryu S, Kang D, Monteiro J, Shin HC, Guallar E, Cho J (2019) Long-term particulate matter exposure and onset of depression in middle-aged men and women. Environ Health Perspect 127:77001. https://doi.org/10.1289/ehp4094
Zimmerman M, Martin J, Clark H, McGonigal P, Harris L, Holst CG (2017) Measuring anxiety in depressed patients: a comparison of the Hamilton Anxiety Rating Scale and the DSM-5 Anxious Distress Specifier Interview. J Psychiatr Res 93:59–63. https://doi.org/10.1016/j.jpsychires.2017.05.014
Funding
The study was supported by the Natural Science Foundation of the Anhui Higher Education Institutions of China, Grant Number: KJ2021ZD0037; the Municipal Health Commission Applied Medical Research project of Anhui Hefei, Grant Number: Hwk2023zc003.
Author information
Authors and Affiliations
Contributions
Zhu DM, Ma SS, and Zhu P conceptualized and designed the study. Xie TQ and Zhang Y were responsible for conducting the analyses, preparing the first draft of the manuscript, and preparing the manuscript for submission. Zhu DM was responsible for obtaining funding for the study, supervising the analyses, and editing drafts of the manuscript. Kong H, Guan LZ, Zhang L, and Yu JK were responsible for data collection and initial data preprocessing. All authors contributed to and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Anhui Mental Health Center (AMHC).
Consent for publication
All authors approved the final manuscript and the submission to this journal.
Conflict of interest
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xie, T., Zhang, Y., Kong, H. et al. Association between ambient particulate matters and anhedonia among patients with depression. Environ Sci Pollut Res 31, 4539–4546 (2024). https://doi.org/10.1007/s11356-023-31474-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-023-31474-9