Abstract
Purpose
This preliminary study aimed to investigate the effects of exergames in a virtual reality environment to improve functional balance during goal-directed functional tasks in postmenopausal women with osteoporosis.
Methods
Twelve volunteer postmenopausal women with osteoporosis were randomly assigned to virtual reality (VRT, n = 6) and conventional multimodal (CMT, n = 6) training groups. The exercise was performed for 6 weeks, 3 days weekly, and 18 sessions. Using a force platform, functional balance assessments were made through four dynamic tasks, including performance-based limits of stability (LOS), curve tracking (CT), sit-to-stand (STS), and turning before and after 18 sessions of treatment. Each task’s time-dependent center of pressure (COP) variables was separately calculated via Kistler-Mars software.
Results
The COP variables of LOS and CT tasks were significantly improved after 6 weeks of CMT and VRT (P ≤ 0.05). In the VRT group, the rising index (P < 0.00), COP sway velocity in STS, and Turn sway were significantly reduced (P < 0.05). Following the VRT, the mean difference of forwarding maximum COP excursion increased (P = 0.03), and errors in CT (P = 0.03) significantly decreased.
Conclusion
The VRT and CMT improved the COP sway parameters during weight-shifting tasks. The VRT was more effective than CMT in increasing the ability to control weight-shifting and dynamic functional tasks in postmenopausal women with osteoporosis. This approach in training has suitable potential to provide convenient error feedback learning.
Similar content being viewed by others
Introduction
Primary osteoporosis is a metabolic and systemic disease characterized by decreased bone density and increased bone fragility due to estrogen deficiency [1]. The fall-related fractures threaten the lives of osteoporotic women [2]. Poor postural balance is one of the most critical intrinsic risk factors for falls and fractures [3]. Postural control is more challenging on dynamic tasks. Maintaining an effective relationship between the center of mass and the base of support during dynamic tasks depends on good interaction between somatosensory, central predictive sets, and musculoskeletal systems [4, 5].
The earlier studies have revealed the positive effects of applying conventional balance training protocols on static/dynamic postural balance and quality of life in osteoporotic women [6]. These conventional training programs have limited impacts on reversing the adverse effects of osteoporosis on the motor control system. They cannot easily develop multi-component training plans that simultaneously use all the impressive components of balance behavior, such as muscular, cognitive, and neural subunits. Also, there is a limited capacity of the translational values obtained from conventional multimodal training to functional activities of daily living due to reinforcement of the internal instead of external focus. High-speed, multi-component motion exercise combined with simulated functional tasks promises to improve functional outcomes [7], so exergames seem to have the potential to be a good alternative or supplement to conventional training protocols. Exergame refers to performing some dynamic and goal-specific tasks instructed by video games. In this way, more attention is paid to the goal of the task, so the external focus is augmented; consequently, motor skills will easily advance to the high levels of the rehabilitation pyramid [8].
Specificity, adaptability, reproducibility, accurate assessment of skill, and the safety of therapeutic practice in virtual environments [9] may be superior to conventional therapeutic exercises. The effects of virtual reality training (VRT) on balance variables have been studied in elderly or neurologically impaired people [10, 11]; however, the results are contrasting [12, 13]. Some of these conflicting results are related to the methods used to assess treatment outcomes. From a biomechanical point of view, force plates can show more optimized movement aspects than other functional tests, such as the timed up-and-go test (TUG) [14] and the Berg balance scale (BBS). The force platform is sensitive enough to detect time-coordinated discrepancy of the center of pressure (COP) through dynamic and functional tasks, such as weight-shifting, chair rising, and turning [15]. Therefore, this preliminary study investigated whether exergames in a virtual reality environment improve functional balance on goal-directed functional tasks more than traditional exercise. For this purpose, dynamic balance control and related fluctuations in COP were monitored during functional tasks, including weight shifts, sit-to-stand, and turning. We hypothesized that virtual reality training might improve the ability to control postural balance during dynamic and functional tasks more than conventional multimodal balance training in osteoporotic women.
Methods
This study is a preliminary single-blind, randomized controlled trial. The study was approved by the medical ethics committee of Tarbiat Modares University and was registered with the Iranian Registry of Clinical Trials as IRCT20101017004952N7.
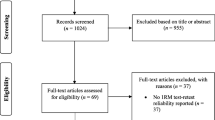
The sample size was estimated according to Toulotte et al.[16], which examined the effect of virtual reality-based exercise programs on balance improvement in senior older adults. The calculation was based on the mean deference of the position of the center of gravity in virtual reality (− 8.1 ± 2.3) and adapted physical activity (− 0.9 ± 0.8) groups, the effect size of 1.87, the alpha of 5%, and power of 80%. Twenty volunteers were recruited from individuals admitted to Baqiyatallah public bone densitometry clinic in Tehran, Iran. The inclusion criteria were: menopause for at least 1 year, T score ≤ − 2.5 at the femoral neck or lumbar regions by world health organization criteria, age 48–65 years, body mass index 22–30 kg/m2, not participating in a regular exercise program (at less 30 min, 2–3 days/week for at least later six months) and femoral neck or lumbar T score ≤ − 2.5. Participants didn’t suffer from visual, vestibular, or major neuromuscular disorders that affect postural balance. The exclusion criteria were unwillingness to participate or cooperate. The training methods and objectives of the study have been fully explained to participants, and they provided written informed consent before entering the study. Figure 1 shows the consort of the allocation procedure. Eight people were excluded for secondary osteoporosis (n = 3), severe osteoarthritis in the knee joint (n = 2), and diabetes (n = 3). Twelve osteoporotic women were randomly enrolled in the conventional multimodal training (CMT, n = 6) and virtual reality (VRT, n = 6) groups. An independent person converted allocation and assignment by blocking randomization using sealed, opaque, and stapled envelopes. One person in the CMT group was reluctant to participate in the study due to the coronavirus pandemic, and she was excluded from the study. The CMT and VRT performed exercises 3 days per week for 6 weeks (18 sessions) under the supervision of a trained physiotherapist. The COP sway was evaluated using the dynamic and weight-shifting tasks before and after training. These tasks included a performance-based limit of stability (LOS), mediolateral tracking curve (CT), sit-to-stand (STS), and turning in level walking (Turn) that were done on the force plate.
Assessment of dynamic and weight-shifting tasks
A computerized force plate recorded the COP sway parameters (9286B, Kistler Co., Winterthur, Switzerland). Pre–post tests were assessed before and after 6 weeks of intervention by an assessor blinded to grouping. The Kistler-Mars software, which supports the Kistler data acquisition system, was used to correctly analyze the characteristics of the postural balance in the tasks. Before the data acquisition, each participant was familiar with the test procedure. Then, each functional task was repeated thrice with one-minute rest in between and 5 min between the assorted tasks in the following order: LOS, CT, STS, and Turn. The test subject's preferred foot positions in LOS, CT, and STS were the same for all three repetitions and were based on the shoulder width while standing during the first test, controlled by recording the foot position on an enclosed special sheet. The examiner stayed close to the participants to protect them from falling.
At the LOS, the participant tried to shift her weight in four completely different directions (forward, backward, right, and left). The test stopped if the trunk flexed, stretched, leaned, or extended shoulders substituted the movement. The reaction time (RT), the COP sway velocity (COPvel), COP directional control (COPdc), COP maximum excursion (COPexc), and maximum body lean (COPlean) were measured [17].
The subject was asked to track a sinusoidal pattern within the CT task. The COP was displayed on the LCD screen to guide the execution of the task. Mean absolute errors (mm), standard deviation (mm), and the area between the reference pattern and the actual COP signal (calculated as the integral of the absolute deviations between the two curves (mm*s)) were determined following tracking the sinusoidal curve.
In the STS examination, the subject performed a vertical upward movement from a bench-adjusted height to keep the hip and knee joints at 90/90. The participant was not allowed to use her hands for support. The weight transfer time (s), rising index (RI), and the average COP sway velocity (mm/s) were scored during STS.
In Turn, the participant was instructed to start walking at least two paces from the force plate, then approach the force plate and perform the 180° rotation on a force plate with the dominant leg. The test ended when the subject returned to the starting point. The time required to complete the 180° Turn in place(s) and the average velocity of the COP sway during the turn time, the turn sway (mm/s), were recorded separately.
Training protocol
Exercises were held one by one in the physiotherapy clinic of Tarbiat Modares University. The duration of training in both groups was set to sixty minutes, 3 days weekly for 6 weeks, and 18 sessions. The training program was established on different days, so the participants in each group were blinded to the training mode of the other group. The exercises in both groups began with five minutes of stretching to warm up. Interval periods were taken into account between activities to avoid declining performance. Both groups followed regular daily activity, nutrition, and medication regimen. The intensity and difficulty of the exercises gradually increased in both groups. In the first 2 weeks, it was done at an easy level; in the second two weeks, it was moderate; in the third 2 weeks, it was done at an advanced level. In the CMT group, the exercise difficulty was adjusted through accessory devices and combined movements, which are explained in Table 1. In the VRT group, the exercise intensity was adjusted by choosing each game’s easy, moderate, and advanced levels.
In both groups, we also measured the 10-point Borg rating of the perceived exertion scale (Borg) which individuals subjectively rate their level of exertion during exercise. In the first 2 weeks of training, we determined the scale of 2–3 for light intensity; in the second 2 weeks, 4–5 for moderate intensity; and in the third two weeks, 6–7 for hard intensity.
Virtual reality training
At the VRT group, the strength balancing exercises were carried out with the help of Xbox 360 games and a Kinect camera (Microsoft, Redmond, WA, USA). The Kinect tracks the participant’s body position and provides feedback if they properly do the task. Eighteen minutes of Your shape: fitness evolved, Kinect sport one, and Kinect Adventures games were selected in which the muscles of the lower extremities, upper limbs, and torso were more involved, in parallel with increasing the difficulty of the task in the game (Fig. 2a). For safety, activity was monitored, but no physical assistance was given. Monitor, Xbox console, and Kinect sensor were set at a 2 m height from the ground and away from the participant's gesture. Verbal commands for the video games had been supplied earlier than the training beginning. Once every six sessions, the difficulty level increased according to the software's instructions.
The site of the monitor, Xbox kinect, and console and samples of body motions in VRT, the movement of the dominant upper limb during discus throw (a); the samples of body motion in standing at the CMT (b). Note the similar movement patterns in the CMT with those that occurred on discus throw in the VRT
GYM Games exercises were selected in your shape, including virtual smash, light race, and stack ‘em up. Each stage was repeated four times in a 2 min trial. At virtual smash, the displayed boxes were accidentally destroyed. In the light race, the participant was asked to bring the feet toward the highlights on the anterior, posterior, left, and right sides by the closer foot. In stack ‘em up, the subject was asked to empty the boxes assembled on the board according to the software instructions by shifting and tilting the upper limb into the highlight chambers. The foam was used under the feet in the stack ‘em up at the third stage.
In Kinect Sport 1, the subjects were done bowling, bump bash (shift position to avoid collision with things thrown), soccer sets (to simulate foot and hand movement in the proprioceptive neuromuscular facilitation (PNF) patterns), sprinting in place (hip and knee flexion movements on the swing leg and balance maintenance on the standing leg as well as continuous reciprocal upper limbs movements), and discus throw (movement of the upper extremity of the dominant arm and the rotational movements of the trunk to simulate the motion of the throw). Finally, in the Kinect adventure game and at the free play section, the participants completed three parts of this game: reflex ridge, rally ball, and 20,000 leaks.
Conventional multimodal training protocol
In the CMT group, conventional strength-balance exercises were considered the same duration as VRT in three positions: sitting, standing, and walking. The time required for sustaining a position was two minutes, and a break of 30 s between each task. Two sets of 10 repetitions were adjusted separately for the left and right sides. The free weights, elastic bands, body blade, SWISS ball (75 cm in diameter), Swedish wall bar, Buso ball, foams, and weighted vests were used for exercise progression. According to the subject's tolerance, these elements were gradually absorbed in the advanced sessions. The exercises in the first 2 weeks were defined as an easy level, the second fourteen days as an intermediate level, and the third fourteen days as an advanced level (Table 1). A sample of movement patterns in CMT at standing (advanced stage) was provided (Fig. 2b).
Statistical analysis
After confirming the data distribution normality using the Shapiro–Wilk test, each group used the paired t-test for pre–post evaluation. The independent sample t-test was performed to compare the difference of changes in the variables between the two training groups. Statistical analysis was performed by SPSS version 19 (IBM, Armonk, NY, USA), and the significance level was set at P ≤ 0.050.
Results
The personal characteristics, including age, height, weight, BMI, and femoral neck /lumbar BMD, showed no significant difference between the groups (P > 0.05) (Table 2).
The effect of two types of exercise on the LOS is illustrated in Table 3. After 18 sessions of CMT, the forward RT was 0.52 s less than the before treatment, which was statistically significant (P = 0.014, effect size = 2.06). In the right direction, the COPexc, COPdc, and COPlean were 22.26 mm, 12.24°, and 1.36°, significantly higher than the baseline values (P = 0.033, effect size = 1.41; P < 0.001, effect size = 4.6; P = 0.035,effect size = 1.46; respectively). In the left direction, the COPvel, COPexc, and COPlean were 17.48 mm/s, 15.83 mm, and 1.25° C, respectively. They showed a significant increase relative to baseline values (P = 0.028, effect size = 1.59; P < 0.001, effect size = 2.2; P = 0.019, effect size = 1.87; respectively). After 6 weeks of intervention in the VRT group, the forward RT was decreased by 2.3 s (P < 0.001, effect size = 2.1), and the forward COPvel increased by about 4.80 mm/s (P < 0.001, effect size = 1.38). The backward COPdc was 13.26 degrees greater than before treatment (P = 0.021, effect size = 1.24). In the right and left directions, COPexc (Pright = 0.022, effect size = 1.57, Pleft = 0.016, effect size = 1.37), COP dc(Pright = 0.001, effect size = 2.02, Pleft = 0.001, effect size = 2.60) and COPlean (Pright = 0.044, effect size = 1.06, Pleft = 0.010, effect size = 1.60) were significantly intensified compared to baseline values. The independent t-test showed that the mean difference of the forward RT was 0.52 in CMT and 0.23 in VRT, and this difference between the two groups was significant (P = 0.028, effect size = 1.56) (Fig. 3a). The mean difference of the COPexc in the VRT group indicates an improvement of 10.75 mm, and the difference between the two groups was significant (P = 0.034, effect size = 1.53) (Fig. 3b). The mean difference of forwarding COPdc was 7.5 degrees higher in the VRT group and − 7.6 degrees lower in the CMT group from each baseline value. This difference was also significant between the two groups (P = 0.038, effect size = 1.53) (Fig. 3c).
The mean differences of forwarding reaction time (a), maximum excursion (b), directional control (c) at LOS task, and absolute errors (d) and area of error (e) at sinusoidal curve tracking task between two groups. CMT: Conventional multimodal training. VRT: Virtual reality training # significant difference between two groups
After 18 sessions of intervention, in the curve tracking via mediolateral weight-shifting, the CMT group showed a decrease in the values of the SD of the absolute error from 44.4 ± 6.1 to 32.66 ± 4.8 mm, which was significant (P < 0.001, effect size = 1.38; Table 3 and Fig. 3d). After the VRT training, the mean/SD of absolute errors (P < 0.001, effect size = 1.06 and 1.75, respectively) and the area (P = 0.016, effect size = 1.60) significantly decreased compared to the baseline value (Table 3 and Fig. 3d, e). CMT showed a difference of − 4.5 mm in the mean of absolute error, while VRT training had a difference of − 24.61 compared to the baseline value. This difference was significant between the two groups (P = 0.022, effect size = 2.47). The area in the CMT group decreased by − 127.99 mm*s, while in the VRT group, it decreased by about − 448.59 mm*s, which was a statistically significant difference between groups (P = 0.045, effect size = 1.60).
In the VRT group during STS (Table 3), the RI significantly decreased from 66.41 ± 2.13 to 56.55 ± 4.89% of body weight (P < 0.001, effect size = 1.70). The COP sway velocity after VRT was markedly reduced from 183.16 ± 6.82 to 146.59 ± 30.86 mm/s (P = 0.010, effect size = 1.46). Regardless of the greater effect of VRT on the quantified parameters, the independent t-test indicated that neither of the two methods had a greater impact on COP-dependent parameters in this task (P > 0.05).
In the Turn task and after training by the VRT, the mean COP sway velocity at the moment of 180 degrees of turning on the dominant leg decreased significantly from 166.64 ± 20.63 to 125.9 ± 21.93 (P = 0.012, effect size = 1.57). Still, this difference was not significant compared to the CMT group (Table 3).
Discussion
This preliminary study aimed to evaluate the practical outcomes of performing active exercises in a virtual reality platform (VRT group) on the balance parameters and simultaneously compare these results with conventional multimodal balance training (CMT group) in osteoporotic women.
Based on the study outcome, at the LOS task, both training modes improved the degree of freedom about COP fluctuations by improving COPvel at forward (VRT) and left (CMT) directions, COPdc at backward (CMT), right (CMT and VRT), and left (VRT) directions. After training, both groups’ SD of the absolute error reduction revealed better control of the COP displacements around the reference line. The RI and COP sway velocity in STS and the sway velocity in Turn were significantly changed only in the VRT group. These parameters didn't reach a significant level after CMT. Decreasing the values of RI after VRT could reflect the lesser forward bending of the trunk after training.
Although the results of this study should be cautiously generalized due to the small sample size, VR training seems more effective than CMT in improving the balance status during weight shifts to forward and lateral directions. The improvement of the forward COPexc and COPdc indicates that VRT had helped osteoporosis women move the COP with greater freedom to the anterior edges of the stability area. Regarding the RT values, the CMT decreased the time interval between the onset of the motor reaction and the issuance of a motor command in the same direction. The results of the CT indicated that the participants in the VRT group could control the voluntary displacement of COP more consistently with the reference curve than the CMT. It was determined by reducing the mean of absolute error and area more than the values illustrated after CMT. Forming the proper error feedback learning provided in the VRT significantly affected the subject's performance in the functional tests.
Both training protocols potently improved the quality of time-dependent COP dispersions at weight-shifting tasks. In dynamic tasks, STS and Turn, the osteoporotic women in the VRT group seem to have attained the proper synergistic ability to control COP fluctuations on the functional base of support to float the position of body segments more exquisitely. These physiological changes in motor control behavior were expected following the motor learning process [18] and adaptability [19].
Adaptability and trainability in the locomotor system provide the capability to the motor control system to accommodate different exercise therapy protocols to optimize motor responses that may cause to decrease the risk of falling in functional activities. The factors that inform the appropriate motor commands are muscle strength and somatosensory functions [20]. Proper neuromuscular coordination [21] and cognitive factors affect predictive sets within the central nervous system [22]. Although both types of protocols have effectively improved COP-related parameters, VRT has been more effective due to rehabilitation codes defined in the motion complexity model and the simultaneous use of several subsystems involved in balance control [8]. This effectiveness could be due to the similarity of VRT with real functional activities and their greater attractiveness to participants. Various visual, auditory, and motivating feedback from VRT directs attention to the intended execution of the functional movement in a suitable manner, which is usually not well-formed in conventional methods. During VRT, the user interacts with the game scenario, and the sensory, cognitive, psychological, and motor functions are stimulated [23,24,25]. It will be more challenging to acquire functional motor skills in traditional exercises where the internal focus is reinforced than in the goal of the task.
In contrast, targeted functional exercises such as VRT use rehabilitation codes, such as cognition, being active, feedback, repetition, and learning more appropriately to reinforce the external focus further, making goal achievement easier for skills [26]. Due to the simulation of the real environment, these exercises can effectively learn and control movements and ultimately transfer motor experiences to new environmental challenges [27]. In addition, the user training of these games at home must be mentioned. Tele-physiotherapy and purposeful training programs can be applied in critical situations like corona pandemic [28, 29]. In line with the present study, Duque et al. revealed that after 6 weeks of exercises in virtual reality environments, LOS was significantly increased in 30 elderly volunteers in the age range of 78 compared with age-matched controls [13]. In a pilot study, Pluchino et al. showed that virtual reality balance training (Wii fit balance) had ameliorated COP fluctuations in the frontal and sagittal planes but had no significant superior outcome to other training modes [30].
In Bieryla’s pilot study, 3 weeks of Xbox Kinect motion-based exercise modified Berg balance and the Fullerton advanced balance scale in ten seniors with an average age of 70 [31]. Babadi and Daneshmandi compared the effects of 9 weeks of VRT with conventional balance training in 36 older adults. In their study and using functional reach test, single leg stance with open/closed eyes, Fullerton advance balance test, and TUG, the same results were recorded after both types of interventions when comparison was made with controls [32].
Visual feedback provided to the participant in the assessment (LOS and CT) and practice methods (VRT) used in this study may impact the results. According to Gold–Berg’s theory, motor pathways, such as the cerebellum, peritoneal lobe of the brain, and the external pre-motor cortex, will dominate when voluntary human movements are directed according to external commands [33]. In contrast, well-learned and self-generated movements in humans cause dominant activity in other parts of the central nerves, such as the basal ganglia and supplementary motor area [34, 35]. STS and Turn tasks are more self-generating movements. There was no visual feedback for the guidance of movement; in this way, the COP-related parameters of these two tasks didn’t reach a significant level at this period of intervention, so neither method was superior to the other.
To comply with ethical principles, this study selected the control group as the CMT group. Perhaps one of the most important limitations in this study is related to restrictions on the degree of freedom in head and neck movements imposed by the nature of the exergames. In virtual reality training, subjects should limit their gaze on the monitor to provide proper visual and auditory feedback, so the somatosensory inputs from head-neck and vestibular systems are confined to excursions on frontal plane. Conversely, the freedom of movement at the head–neck and eyes provided in CMT had a substantial role in forming good righting reflexes at dynamic postural control. So it is suggested that the efficacy of VRT and CMT is examined on the vestibular system via a sensory organization test to clarify better their possible effects on righting reflexes, especially at levels 5 and 6 of this test. A larger sample size and a follow-up assessment are required to enhance external validity. It is suggested that future studies follow the results at least one month later to compare the consistency of the interventions performed on balance factors of functional motor skills. Evaluation of muscle synergy and co-contraction by electromyography can effectively recognize the motor control changes following VRT, which is recommended in future studies.
Conclusion
Both conventional multimodal exercise therapy and VR training effectively improved functional motor skills. The COP sway results showed that the 18 virtual reality training sessions were comparable to CMT in improving postural control during weight-shifting on a fixed support surface. This conclusion is especially significant when transferring weight to the front and lateral edges of the base of support.
References
Young LY, Holland EG (1995) Applied therapeutics: the clinical use of drugs. Applied Therapeutics. Inc, Vancouver, WA, pp 15–16
Uusi-Rasi K, Karinkanta S, Tokola K, Kannus P, Sievänen H (2019) Bone mass and strength and fall-related fractures in older age. J Osteoporos 2019:1–6
Kiel DP, Schmader K, Lin F (2018) Falls in older persons: risk factors and patient evaluation. UpToDate Inc., UpToDate Waltham
Hsu WL, Chen CY, Tsauo JY, Yang RS (2014) Balance control in elderly people with osteoporosis. J Formos Med Assoc 113(6):334–339
Pollock AS, Durward BR, Rowe PJ, Paul JP (2000) What is balance? Clin Rehabil 14(4):402–406
Otero M, Esain I, González-Suarez ÁM, Gil SM (2017) The effectiveness of a basic exercise intervention to improve strength and balance in women with osteoporosis. Clin Interv Aging 12:505
Hawley JA (2008) Specificity of training adaptation: time for a rethink? J Physiol 586(1):1–2
Lederman E (2010) Neuromuscular rehabilitation in manual and physical therapies: principles to practice: Churchill Livingstone/Elsevier, Amstradam
Porras DC, Siemonsma P, Inzelberg R, Zeilig G, Plotnik M (2018) Advantages of virtual reality in the rehabilitation of balance and gait: systematic review. Neurology 90(22):1017–1025
Kamińska MS, Miller A, Rotter I, Szylińska A, Grochans E (2018) The effectiveness of virtual reality training in reducing the risk of falls among elderly people. Clin Interv Aging 13:2329
Dockx K, Bekkers EM, Van den Bergh V, Ginis P, Rochester L, Hausdorff JM et al (2016) Virtual reality for rehabilitation in Parkinson’s disease. Cochrane Database Sys Rev. https://doi.org/10.1002/14651858.CD010760.pub2
Booth V, Masud T, Connell L, Bath-Hextall F (2014) The effectiveness of virtual reality interventions in improving balance in adults with impaired balance compared with standard or no treatment: a systematic review and meta-analysis. Clin Rehabil 28(5):419–431
Duque G, Boersma D, Loza-Diaz G, Hassan S, Suarez H, Geisinger D et al (2013) Effects of balance training using a virtual-reality system in older fallers. Clin Interv Aging 8:257
Bonaiuti D, Shea B, Iovine R, Negrini S, Welch V, Kemper HH et al (1996) Exercise for preventing and treating osteoporosis in postmenopausal women. Cochrane database of systematic reviews. John Wiley and Sons Ltd, Chichester
Blaszczyk JW (2016) The use of force-plate posturography in the assessment of postural instability. Gait Posture 44:1–6
Toulotte C, Toursel C, Olivier N (2012) Wii Fit® training vs Adapted Physical Activities: which one is the most appropriate to improve the balance of independent senior subjects? A randomized controlled study. Clin Rehabilitat 26(9):827–835
Rezaei MK, Torkaman G, Bahrami F, Bayat N (2021) Are weight shifting and dynamic control strategies different in postmenopausal women with and without type-I osteoporosis? Exp Gerontol 154:111529
Seidler RD (2004) Multiple motor learning experiences enhance motor adaptability. J Cogn Neurosci 16(1):65–73
Mulder T, Hochstenbach J (2001) Adaptability and flexibility of the human motor system: implications for neurological rehabilitation. Neural Plast 8(1–2):131–140
Qiu F, Cole MH, Davids K, Hennig E, Silburn P, Netscher H et al (2012) Enhanced somatosensory information decreases postural sway in older people. Gait Posture 35(4):630–635
Lord SR, Castell S (1994) Physical activity program for older persons: effect on balance, strength, neuromuscular control, and reaction time. Arch Phys Med Rehabil 75(6):648–652
Rogge A-K, Röder B, Zech A, Nagel V, Hollander K, Braumann K-M et al (2017) Balance training improves memory and spatial cognition in healthy adults. Sci Rep 7(1):1–10
Plante TG, Frazier S, Tittle A, Babula M, Ferlic E, Riggs E (2003) Does virtual reality enhance the psychological benefits of exercise? J Human Mov Stu 45(6), 485–507
Qian J, McDonough DJ, Gao Z (2020) The Effectiveness of virtual reality exercise on individual’s physiological, psychological and rehabilitative outcomes: a systematic review. Int J Environ Res Public Health 17(11):4133
Costa MTS, Vieira LP, de Oliveira BE, Oliveira LM, Maillot P, Vaghetti CAO et al (2019) Virtual reality-based exercise with exergames as medicine in different contexts: a short review clinical practice and epidemiology in mental health. CPEMH 15:15
Van Vliet PM, Wulf G (2006) Extrinsic feedback for motor learning after stroke: what is the evidence? Disabil Rehabil 28(13–14):831–840
Slater M, Howell J, Steed A, Pertaub DP, Garau M (2000) Acting in virtual reality. In proceedings of the third international conference on collaborative virtual environments, pp 103–110
Schröder J, Van Criekinge T, Embrechts E, Celis X, Van Schuppen J, Truijen S et al (2019) Combining the benefits of tele-rehabilitation and virtual reality-based balance training: a systematic review on feasibility and effectiveness. Disabil Rehabil Assist Technol 14(1):2–11
Pastora-Bernal JM, Martín-Valero R, Barón-López FJ, Estebanez-Pérez MJ (2017) Evidence of benefit of telerehabitation after orthopedic surgery: a systematic review. J Med Internet Res 19(4):e6836
Pluchino A, Lee SY, Asfour S, Roos BA, Signorile JF (2012) Pilot study comparing changes in postural control after training using a video game balance board program and two standard activity-based balance intervention programs. Arch Phys Med Rehabil 93(7):1138–1146
Bieryla KA (2016) Xbox Kinect training to improve clinical measures of balance in older adults: a pilot study. Aging Clin Exp Res 28(3):451–457
Babadi SY, Daneshmandi H (2021) Effects of virtual reality versus conventional balance training on balance of the elderly. Exp Gerontol 153:111498
Hackney ME, Lee HL, Battisto J, Crosson B, McGregor KM (2015) Context-dependent neural activation: internally and externally guided rhythmic lower limb movement in individuals with and without neurodegenerative disease. Front Neurol 6:251
Debaere F, Wenderoth N, Sunaert S, Van Hecke P, Swinnen SP (2003) Internal vs external generation of movements: differential neural pathways involved in bimanual coordination performed in the presence or absence of augmented visual feedback. Neuroimage 19(3):764–776
Goldberg G (1985) Supplementary motor area structure and function: review and hypotheses. Behav Brain Sci 8(4):567–588
Acknowledgements
We gratefully acknowledge all participants who participated in this study.
Funding
This project was supported by a grant from the Medical Sciences Faculty of Tarbiat Modares University, Tehran, Iran. We received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Study conception and design: GT, MKR. Acquisition of data: GT, MKR, NB. Analysis and interpretation of data: GT, MKR, FB. Drafting of the manuscript: GT, MKR, FB, NB. Critical revision: GT, MKR.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement and Informed consent
The study was approved by the Tarbiat Modares University Research Ethics Board (Project number: IR.MODARES.REC.1397.050) and was conducted in compliance with the standards set by the Declaration of Helsinki. All participants provided informed written consent prior to their participation in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rezaei, M.K., Torkaman, G., Bahrami, F. et al. The effect of six week virtual reality training on the improvement of functional balance in women with type-I osteoporosis: A preliminary study. Sport Sci Health 19, 185–194 (2023). https://doi.org/10.1007/s11332-022-01018-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11332-022-01018-8