Abstract
Background
Obstructive sleep apnea–hypopnea syndrome (OSAHS) is a common respiratory disease with potential lethality. At present, the commonly used treatment method is continuous positive airway pressure ventilation, but with the prolongation of the course of the disease, the effect of single ventilation on the improvement of oxidative stress levels is not good. Lipoic acid is a commonly used antioxidant in clinics. In this paper, lipoic acid combined with continuous positive airway pressure ventilation is used to explore whether it has a better therapeutic effect on patients.
Aim
To probe into the clinical efficacy of lipoic acid combined with continuous positive airway pressure ventilation in the therapy of OSAHS.
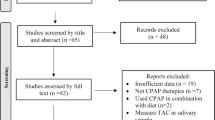
Methods
82 patients with OSAHS who were cured in our hospital from March 2021 to September 2022 were prospectively collected as subjects. Based on different treatment methods, patients were grouped into a control group (43 cases) and an observation group (39 cases). The control group was treated with continuous positive airway pressure (CPAP), and the observation group was treated with lipoic acid based on control group. The therapeutic effects were measured by apnea hypopnea index (AHI), oxygen saturation (SpO2), mean oxygen saturation (MSpO2), serum malondialdehyde (MDA), superoxide dismutase (SOD), hypoxia inducible factor-1α (HIF-1α) levels, peripheral blood γ-aminobutyric acid, melatonin levels.
Results
The clinical effectiveness of the observation group was better (P < 0.05). After treatment, AHI, the levels of MDA and HIF-1α in the observation group were lower and SpO2, MSpO2 and the level of SOD, γ- aminobutyric acid, and melatonin were higher than those in the control group (P < 0.05). The levels of γ- aminobutyric acid and melatonin were negatively correlated with the severity of symptoms, ESS, and AIS scores (P < 0.05).
Conclusions
The clinical effect of lipoic acid combined with CPAP in the treatment of OSAHS is better, and it has a positive effect on the levels of γ-aminobutyric acid and melatonin in peripheral blood.
Lipoic acid was added to the original method for treatment, and the therapeutic effect was greatly improved.






Similar content being viewed by others
Data availability
We can also provide specific data and materials upon request.
References
Cepeda FX, Virmondes L, Rodrigues S, Dutra-Marques ACB, Toschi-Dias E, Ferreira-Camargo FC, Hussid MF, Rondon MUP, Alves MJNN, Trombetta IC (2019) Identifying the risk of obstructive sleep apnea in metabolic syndrome patients: diagnostic accuracy of the Berlin Questionnaire. PLoS ONE 14(5):e0217058
Kayabasi S, Hizli O, Yildirim G (2019) The association between obstructive sleep apnea and hearing loss: a cross-sectional analysis. Eur Arch Otorhinolaryngol 276(8):2215–2221
Swami SS, Aye SL, Trivedi Y, Bolgarina Z, Desai HN, Senaratne M, Mohammed L (2023) From snoring to soaring: unveiling the positive effects of continuous positive airway pressure ventilation on cardiovascular health in patients with obstructive sleep apnoea through a systematic review. Cureus 15(9):e45076
Abuyassin B, Badran M, Ayas NT, Laher I (2019) The antioxidant α-lipoic acid attenuates intermittent hypoxia-related renal injury in a mouse model of sleep apnea. Sleep 42(6):zsz066
Sueviriyapan N, Granados-Fuentes D, Simon T, Herzog ED, Henson MA (2021) Modelling the functional roles of synaptic and extra-synaptic γ-aminobutyric acid receptor dynamics in circadian timekeeping. J R Soc Interface 18(182):20210454
Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK, Marcus CL, Mehra R, Parthasarathy S, Quan SF, Redline S, Strohl KP, Davidson Ward SL, Tangredi MM, American Academy of Sleep Medicine (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the scoring of sleep and associated events Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med 8(5):597–619
Wang W, Zheng Y, Li M, Lin S, Lin H (2021) Recent advances in studies on the role of neuroendocrine disorders in obstructive sleep apnea-hypopnea syndrome-related atherosclerosis. Nat Sci Sleep 27(13):1331–1345
Baillieul S, Dekkers M, Brill AK, Schmidt MH, Detante O, Pépin JL, Tamisier R, Bassetti CLA (2022) Sleep apnoea and ischaemic stroke: current knowledge and future directions. Lancet Neurol 21(1):78–88
Sun HL, Sun BL, Chen DW, Chen Y, Li WW, Xu MY, Shen YY, Xu ZQ, Wang YJ, Bu XL (2019) Plasma α-synuclein levels are increased in patients with obstructive sleep apnea syndrome. Ann Clin Transl Neurol 6(4):788–794
Ma XR, Wang Y, Sun YC (2019) Imbalance of osteoprotegerin/receptor activator of nuclear factor-κB ligand and oxidative stress in patients with obstructive sleep apnea-hypopnea syndrome. Chin Med J (Engl) 132(1):25–29
Gleeson M, McNicholas WT (2022) Bidirectional relationships of comorbidity with obstructive sleep apnoea. Eur Respir Rev 31(164):210256
Ghadiri M, Grunstein RR (2020) Clinical side effects of continuous positive airway pressure in patients with obstructive sleep apnoea. Respirology 25(6):593–602
Hillman DR (2022) Is continuous positive airway pressure all there is? Alternative perioperative treatments for obstructive sleep apnea. Anesthesiology 137(1):1–3
Wimms AJ, Kelly JL, Turnbull CD, McMillan A, Craig SE, O’Reilly JF, Nickol AH, Hedley EL, Decker MD, Willes LA, Calverley PMA, Benjafield AV, Stradling JR, Morrell MJ, MERGE trial investigators (2020) Continuous positive airway pressure versus standard care for the treatment of people with mild obstructive sleep apnoea (MERGE): a multicentre, randomised controlled trial. Lancet Respir Med 8(4):349–358
Badran M, Abuyassin B, Golbidi S, Ayas N, Laher I (2019) Alpha lipoic acid improves endothelial function and oxidative stress in mice exposed to chronic intermittent hypoxia. Oxid Med Cell Longev 2019:4093018
Jiang XM, Yamamoto K, Tsuchiya T, Sofuni A, Mukai S, Nagakawa Y, Itoi T (2018) Magnetic compression anastomosis for biliary obstruction after partial hepatectomy. Endoscopy 50(6):E144–E145
Ogura T, Okuda A, Miyano A, Kamiyama R, Nishioka N, Higuchi K (2018) Double intrahepatic bile duct puncture: a pitfall during endoscopic ultrasound-guided hepaticogastrostomy. Endoscopy 50(8):E195–E196
Wang W, Feng Y, Aimaiti Y, Jin X, Mao X, Li D (2018) TGFβ signaling controls intrahepatic bile duct development may through regulating the Jagged1-Notch-Sox9 signaling axis. J Cell Physiol 233(8):5780–5791
Fatemeh G, Sajjad M, Niloufar R, Neda S, Leila S, Khadijeh M (2022) Effect of melatonin supplementation on sleep quality: a systematic review and meta-analysis of randomized controlled trials. J Neurol 269(1):205–216
Gaspar LS, Hesse J, Yalçin M, Santos B, Carvalhas-Almeida C, Ferreira M, Moita J, Relógio A, Cavadas C, Álvaro AR (2021) Long-term continuous positive airway pressure treatment ameliorates biological clock disruptions in obstructive sleep apnea. EBioMedicine 65:103248
Vasey C, McBride J, Penta K (2021) Circadian rhythm dysregulation and restoration: the role of melatonin. Nutrients 13(10):3480
Hohor S, Mandanach C, Maftei A, Zugravu CA, Oțelea MR (2023) Impaired melatonin secretion, oxidative stress and metabolic syndrome in night shift work. Antioxidants (Basel) 12(4):959
Cipolla-Neto J, Amaral FGD (2018) Melatonin as a hormone: new physiological and clinical insights. Endocr Rev 39(6):990–1028
Amaral FGD, Cipolla-Neto J (2018) A brief review about melatonin, a pineal hormone. Arch Endocrinol Metab 62(4):472–479
Funding
Self-funded research project of the Health Commission of Guangxi Zhuang Autonomous Region (Z20201467).
Guangxi Zhuang Autonomous Region Health Department,Z20201467,Rihua Wang
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethic approval and consent to participate
This study was approved by the Ethics Committee of Jiangbin Hospital of Guangxi Zhuang Autonomous Region, and informed consent was obtained from the patients.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, R., Bao, Y., Song, P. et al. To observe the clinical effect of lipoic acid combined with continuous positive airway pressure ventilation in treating obstructive sleep apnea–hypopnea syndrome and its effect on peripheral blood γ-aminobutyric acid and melatonin levels. Sleep Breath (2024). https://doi.org/10.1007/s11325-024-03012-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11325-024-03012-5