Abstract
Purposes
The prevalence of sleep-disordered breathing (SDB) is high in patients with heart failure (HF), while the prevalence of SDB in HF with different left ventricular ejection fractions (LVEF) has rarely been reported. We aimed to explore the prevalence and clinical characteristics of SDB in patients with HF having different LVEF.
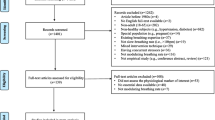
Methods
Patients with stable HF were consecutively enrolled. All patients underwent portable overnight cardiorespiratory polygraphy and echocardiography. According to their LVEF, the patients were divided into the HFrEF (HF with reduced EF, EF < 40%), HFmrEF (HF with mid-range EF, 40 ≤ EF < 50), and HFpEF groups (HF with preserved EF, EF ≥ 50%). The prevalence and clinical data of SDB among the 3 groups were then compared.
Results
A total of 252 patients, including 134 men, were enrolled in the study. The prevalence of SDB in patients with HF was 70%. Obstructive sleep apnea (OSA) was diagnosed in 48% and central sleep apnea (CSA) in 22%. The prevalence of SDB in the HFrEE, HFmrEF, and HFpEF groups was 86%, 86%, and 62%, respectively (P = 0.001). The prevalence of OSA among the 3 groups was 42%, 47%, and 49%, respectively (P = 0.708), while the prevalence of CSA among the 3 groups was 44%, 40%, and 13% (P < 0.001). Logistic regression analysis revealed that age and BMI were independent risk factors for OSA in patients with HF, while LVEF and smoking were independent risk factors for CSA in patients with HF. Correlational analyses revealed that LVEF was negatively correlated with apnea–hypopnea index (AHI) (r = -0.309, P < 0.001) and central apnea index (CAI) ( r = -0.558, P < 0.001), while there was no significant correlation with obstructive apnea index (OAI). The ROC curve revealed that LVEF could predict the occurrence of CSA and SDB, with AUC = 0.683 (95%CI 0.600–0.767, P < 0.001) and AUC = 0.630 (95%CI 0.559–0.702, P = 0.001), but not of OSA.
Conclusions
SDB was highly common in HF, and the prevalence of SDB was different in HF with different LVEF, mainly due to the difference in cardiac functions. The prevalence and severity of SDB in HFrEF and HFmrEF were significantly higher than those in HFpEF, which was mainly related to the increase in CSA. When HFmrEF was similar to HFrEF in cardiac functions, the prevalence, type, and severity of SDB were similar between the two groups. Changes in LVEF had a significant impact on CAI, but not on OAI. LVEF can predict the occurrence of CSA and SDB to a certain extent.


Similar content being viewed by others
References
Kasai T (2012) Sleep apnea and heart failure. J Cardiol 60(2):78–85. https://doi.org/10.1016/j.jjcc.2012.05.013
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, Gonzalez-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 18(8):891–975. https://doi.org/10.1002/ejhf.592
Sanchez-De-La-Torre M, Campos-Rodriguez F, Barbe F (2013) Obstructive sleep apnoea and cardiovascular disease. Lancet Respir Med 1(1):61–72. https://doi.org/10.1016/S2213-2600(12)70051-6
White LH, Bradley TD (2013) Role of nocturnal rostral fluid shift in the pathogenesis of obstructive and central sleep apnoea. J Physiol 591(5):1179–1193. https://doi.org/10.1113/jphysiol.2012.245159
Elias RM, Bradley TD, Kasai T, Motwani SS, Chan CT (2012) Rostral overnight fluid shift in end-stage renal disease: relationship with obstructive sleep apnea. Nephrol Dial Transplant 27(4):1569–1573. https://doi.org/10.1093/ndt/gfr605
Redolfi S, Yumino D, Ruttanaumpawan P, Yau B, Su MC, Lam J, Bradley TD (2009) Relationship between overnight rostral fluid shift and Obstructive Sleep Apnea in nonobese men. Am J Respir Crit Care Med 179(3):241–246. https://doi.org/10.1164/rccm.200807-1076OC
Oldenburg O, Bitter T, Wiemer M, Langer C, Horstkotte D, Piper C (2009) Pulmonary capillary wedge pressure and pulmonary arterial pressure in heart failure patients with sleep-disordered breathing. Sleep Med 10(7):726–730. https://doi.org/10.1016/j.sleep.2008.08.004
Javaheri S, Barbe F, Campos-Rodriguez F, Dempsey JA, Khayat R, Javaheri S, Malhotra A, Martinez-Garcia MA, Mehra R, Pack AI, Polotsky VY, Redline S, Somers VK (2017) Sleep apnea: types, mechanisms, and clinical cardiovascular consequences. J Am Coll Cardiol 69(7):841–858. https://doi.org/10.1016/j.jacc.2016.11.069
Herrscher TE, Akre H, Overland B, Sandvik L, Westheim AS (2011) High prevalence of sleep apnea in heart failure outpatients: even in patients with preserved systolic function. J Card Fail 17(5):420–425. https://doi.org/10.1016/j.cardfail.2011.01.013
Sekizuka H, Osada N, Miyake F (2013) Sleep disordered breathing in heart failure patients with reduced versus preserved ejection fraction. Heart Lung Circ 22(2):104–109. https://doi.org/10.1016/j.hlc.2012.08.006
Oldenburg O, Lamp B, Faber L, Teschler H, Horstkotte D, Topfer V (2007) Sleep-disordered breathing in patients with symptomatic heart failure: a contemporary study of prevalence in and characteristics of 700 patients. Eur J Heart Fail 9(3):251–257. https://doi.org/10.1016/j.ejheart.2006.08.003
Geib T, Plappert N, Roth T, Popp R, Birner C, Maier LS, Pfeifer M, Arzt M (2015) Prevalence of sleep-disordered breathing-related symptoms in patients with chronic heart failure and reduced ejection fraction. Can J Cardiol 31(7):839–845. https://doi.org/10.1016/j.cjca.2015.02.025
Yumino D, Wang H, Floras JS, Newton GE, Mak S, Ruttanaumpawan P, Parker JD, Bradley TD (2009) Prevalence and physiological predictors of sleep apnea in patients with heart failure and systolic dysfunction. J Card Fail 15(4):279–285. https://doi.org/10.1016/j.cardfail.2008.11.015
Javaheri S, Parker TJ, Liming JD, Corbett WS, Nishiyama H, Wexler L, Roselle GA (1998) Sleep apnea in 81 ambulatory male patients with stable heart failure. Types and their prevalences, consequences, and presentations. Circulation 97(21):2154–2159. https://doi.org/10.1161/01.cir.97.21.2154
Chan J, Sanderson J, Chan W, Lai C, Choy D, Ho A, Leung R (1997) Prevalence of sleep-disordered breathing in diastolic heart failure. Chest 111(6):1488–1493. https://doi.org/10.1378/chest.111.6.1488
Bitter T, Faber L, Hering D, Langer C, Horstkotte D, Oldenburg O (2009) Sleep-disordered breathing in heart failure with normal left ventricular ejection fraction. Eur J Heart Fail 11(6):602–608. https://doi.org/10.1093/eurjhf/hfp057
Schulz R, Blau A, Borgel J, Duchna HW, Fietze I, Koper I, Prenzel R, Schadlich S, Schmitt J, Tasci S, Andreas S (2007) Sleep apnoea in heart failure. Eur Respir J 29(6):1201–1205. https://doi.org/10.1183/09031936.00037106
Cowie MR, Gallagher AM (2017) Sleep disordered breathing and heart failure: What does the future hold? JACC Heart Fail 5(10):715–723. https://doi.org/10.1016/j.jchf.2017.06.016
Brack T, Thuer I, Clarenbach CF, Senn O, Noll G, Russi EW, Bloch KE (2007) Daytime Cheyne-Stokes respiration in ambulatory patients with severe congestive heart failure is associated with increased mortality. Chest 132(5):1463–1471. https://doi.org/10.1378/chest.07-0121
Cowie MR, Woehrle H, Wegscheider K, Angermann C, D’Ortho MP, Erdmann E, Levy P, Simonds AK, Somers VK, Zannad F, Teschler H (2015) Adaptive servo-ventilation for central sleep apnea in systolic heart failure. N Engl J Med 373(12):1095–1105. https://doi.org/10.1056/NEJMoa1506459
Orr JE, Ayappa I, Eckert DJ, Feldman JL, Jackson CL, Javaheri S, Khayat RN, Martin JL, Mehra R, Naughton MT, Randerath WJ, Sands SA, Somers VK, Badr MS (2021) Research priorities for patients with heart failure and central sleep apnea. An official american thoracic society research statement. Am J Respir Crit Care Med 203(6):e11–e24. https://doi.org/10.1164/rccm.202101-0190ST
Cabac-Pogorevici I, Revenco V (2021) Heart failure and central sleep apnea in the era of implantable recorders. Anatol J Cardiol 25(4):216–224. https://doi.org/10.5152/AnatolJCardiol.2021.63668
Srivastava PK, Hsu JJ, Ziaeian B, Fonarow GC (2020) Heart failure with mid-range ejection fraction. Curr Heart Fail Rep 17(1):1–8. https://doi.org/10.1007/s11897-019-00451-0
Cho DH, Yoo BS (2021) Current prevalence, incidence, and outcomes of heart failure with preserved ejection fraction. Heart Fail Clin 17(3):315–326. https://doi.org/10.1016/j.hfc.2021.03.002
Dunlay SM, Roger VL, Redfield MM (2017) Epidemiology of heart failure with preserved ejection fraction. Nat Rev Cardiol 14(10):591–602. https://doi.org/10.1038/nrcardio.2017.65
Hogg K, Swedberg K, Mcmurray J (2004) Heart failure with preserved left ventricular systolic function; epidemiology, clinical characteristics, and prognosis. J Am Coll Cardiol 43(3):317–327. https://doi.org/10.1016/j.jacc.2003.07.046
Vasan RS, Levy D (2000) Defining diastolic heart failure: a call for standardized diagnostic criteria. Circulation 101(17):2118–2121. https://doi.org/10.1161/01.cir.101.17.2118
Borlaug BA (2014) The pathophysiology of heart failure with preserved ejection fraction. Nat Rev Cardiol 11(9):507–515. https://doi.org/10.1038/nrcardio.2014.83
Kampani G, Sen MK, Suri JC, Sharma M (2010) Prevalence and profile of sleep disordered breathing amongst patients with congestive heart failure. Indian J Sleep Med 5(4):120–127. https://doi.org/10.5005/ijsm-5-4-120
Ding N, Ni BQ, Zhang XL, Zha WJ, Hutchinson SZ, Lin W, Huang M, Zhang SJ, Wang H (2014) Elimination of central sleep apnea by cardiac valve replacement: a continuous follow-up study in patients with rheumatic valvular heart disease. Sleep Med 15(8):880–886. https://doi.org/10.1016/j.sleep.2014.02.007
Erman MK, Stewart D, Einhorn D, Gordon N, Casal E (2007) Validation of the ApneaLink for the screening of sleep apnea: a novel and simple single-channel recording device. J Clin Sleep Med 3(4):387–392
Cho JH, Kim HJ (2017) Validation of ApneaLink Plus for the diagnosis of sleep apnea. Sleep Breath 21(3):799–807. https://doi.org/10.1007/s11325-017-1532-3
Acknowledgements
The authors gratefully acknowledge the doctors Dan Huang, Xin Wang, Yaowu Liu, and Gaoliang Yan of Zhongda Hospital affiliated to Southeast University for helping to examine the patients.
Funding
This work was supported by Natural Science Foundation of Jiangsu Province (No. BK20210231). The sponsor had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interests
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest, or non-financial interest in the subject matter or materials discussed in this manuscript.
Ethical approval
This study was approved by the institutional ethics committee for clinical research of Zhongda Hospital affiliated to the Southeast University (Ethical No.: 2020ZDSYLL278-P01). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Study registration
This study was registered in the Chinese Clinical Trial Registry (No.: ChiCTR2100047256).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, T., Yu, Fc., Wei, Q. et al. Prevalence and clinical characteristics of sleep-disordered breathing in patients with heart failure of different left ventricular ejection fractions. Sleep Breath 27, 245–253 (2023). https://doi.org/10.1007/s11325-022-02611-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-022-02611-4