Abstract
Objective
Previous studies suggest a relationship between sleep disordered breathing (SDB) and lower extremity artery disease (LEAD) though disagreements remain. This study was performed to assess the association between SDB and LEAD in a metaanalysis.
Methods
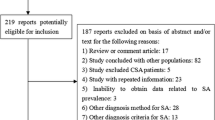
PubMed and Embase databases were searched for observational studies. A random-effects model incorporating between-study heterogeneity was used to pool the data.
Results
The search revealed 7 studies including 152,885 participants. Patients with SDB had higher odds of LEAD (risk ratio [RR] = 1.32, 95% confidence interval [CI] = 1.07 to 1.63, p = 0.01, I 2 = 66%) compared to non-SDB participants. In subgroup analyses, SDB was related to higher odds of LEAD in patients with stroke or diabetes (RR = 3.28, p < 0.001) than in a community-derived population (RR = 1.17, p = 0.08; p for subgroup difference < 0.001). Furthermore, the odds of LEAD was increased in patients with moderate (RR = 1.34, 95% CI = 1.04 to 1.73, p = 0.02) or severe SDB (RR = 1.81, 95% CI = 1.08 to 3.03, p = 0.02), but not in those with mild SDB (RR = 0.94, 95% CI = 0.69 to 1.29, p = 0.71). Differences in study design or methods for LEAD diagnosis did not appear to affect the association between SDB and LEAD.
Conclusions
Patients with SDB have higher odds of LEAD compared to non-SDB participants.




Similar content being viewed by others
References
Javaheri S, Barbe F, Campos-Rodriguez F, Dempsey JA, Khayat R, Malhotra A, Martinez-Garcia MA, Mehra R, Pack AI, Polotsky VY, Redline S, Somers VK (2017) Sleep apnea: types, mechanisms, and clinical cardiovascular consequences. J Am Coll Cardiol 69(7):841–858. https://doi.org/10.1016/j.jacc.2016.11.069
Morsy NE, Farrag NS, Zaki NFW, Badawy AY, Abdelhafez SA, El-Gilany AH, El Shafey MM, Pandi-Perumal SR, Spence DW, BaHammam AS (2019) Obstructive sleep apnea: personal, societal, public health, and legal implications. Rev Environ Health 34(2):153–169. https://doi.org/10.1515/reveh-2018-0068
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM (2013) Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 177(9):1006–1014. https://doi.org/10.1093/aje/kws342
Yoshihisa A, Takeishi Y (2019) Sleep disordered breathing and cardiovascular diseases. J Atheroscler Thromb 26(4):315–327. https://doi.org/10.5551/jat.RV17032
Mehra R (2019) Sleep apnea and the heart. Cleve Clin J Med 86(9 Suppl 1):10–18. https://doi.org/10.3949/ccjm.86.s1.03
Rivera-Perez SJ, Martinez D, Araujo GN, Goncalves SC, Lazzaretti LK, Wainstein RV, Wainstein MV, Ribeiro JP (2019) Severity of obstructive sleep apnea and extension of coronary artery disease. Sleep Breath 23(3):747–752. https://doi.org/10.1007/s11325-018-1769-5
Qu H, Guo M, Zhang Y, Shi DZ (2018) Obstructive sleep apnea increases the risk of cardiac events after percutaneous coronary intervention: a meta-analysis of prospective cohort studies. Sleep Breath 22(1):33–40. https://doi.org/10.1007/s11325-017-1503-8
Wang X, Ouyang Y, Wang Z, Zhao G, Liu L, Bi Y (2013) Obstructive sleep apnea and risk of cardiovascular disease and all-cause mortality: a meta-analysis of prospective cohort studies. Int J Cardiol 169(3):207–214. https://doi.org/10.1016/j.ijcard.2013.08.088
Gerhard-Herman MD, Gornik HL, Barrett C, Barshes NR, Corriere MA, Drachman DE, Fleisher LA, Fowkes FGR, Hamburg NM, Kinlay S, Lookstein R, Misra S, Mureebe L, Olin JW, Patel RAG, Regensteiner JG, Schanzer A, Shishehbor MH, Stewart KJ, Treat-Jacobson D, Walsh ME (2017) 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol 69(11):e71–e126. https://doi.org/10.1016/j.jacc.2016.11.007
Fowkes FG, Aboyans V, Fowkes FJ, McDermott MM, Sampson UK, Criqui MH (2017) Peripheral artery disease: epidemiology and global perspectives. Nat Rev Cardiol 14(3):156–170. https://doi.org/10.1038/nrcardio.2016.179
Kithcart AP, Beckman JA (2018) ACC/AHA versus ESC guidelines for diagnosis and management of peripheral artery disease: JACC guideline comparison. J Am Coll Cardiol 72(22):2789–2801. https://doi.org/10.1016/j.jacc.2018.09.041
Ismaeel A, Brumberg RS, Kirk JS, Papoutsi E, Farmer PJ, Bohannon WT, Smith RS, Eidson JL, Sawicki I, Koutakis P (2018) Oxidative stress and arterial dysfunction in peripheral artery disease. Antioxidants (Basel) 7(10). https://doi.org/10.3390/antiox7100145
Baltzis D, Bakker JP, Patel SR, Veves A (2016) Obstructive sleep apnea and vascular diseases. Compr Physiol 6(3):1519–1528. https://doi.org/10.1002/cphy.c150029
Lavie L (2015) Oxidative stress in obstructive sleep apnea and intermittent hypoxia—revisited—the bad ugly and good: implications to the heart and brain. Sleep Med Rev 20:27–45. https://doi.org/10.1016/j.smrv.2014.07.003
Nachtmann A, Stang A, Wang YM, Wondzinski E, Thilmann AF (2003) Association of obstructive sleep apnea and stenotic artery disease in ischemic stroke patients. Atherosclerosis 169(2):301–307. https://doi.org/10.1016/s0021-9150(03)00195-3
Chen JC, Koo M, Hwang JH (2015) Risks of peripheral arterial occlusive disease in patients with obstructive sleep apnoea: a population-based case-control study. Clin Otolaryngol 40(5):437–442. https://doi.org/10.1111/coa.12393
Shah N, Allison M, Teng Y, Wassertheil-Smoller S, Sotres-Alvarez D, Ramos AR, Zee PC, Criqui MH, Yaggi HK, Gallo LC, Redline S, Kaplan RC (2015) Sleep apnea is independently associated with peripheral arterial disease in the Hispanic Community Health Study/Study of Latinos. Arterioscler Thromb Vasc Biol 35(3):710–715. https://doi.org/10.1161/ATVBAHA.114.304625
Nagayoshi M, Lutsey PL, Benkeser D, Wassel CL, Folsom AR, Shahar E, Iso H, Allison MA, Criqui MH, Redline S (2016) Association of sleep apnea and sleep duration with peripheral artery disease: the Multi-Ethnic Study of Atherosclerosis (MESA). Atherosclerosis 251:467–475. https://doi.org/10.1016/j.atherosclerosis.2016.06.040
Stadler S, Jalili S, Schreib A, Jung B, Zeman F, Boger CA, Heid IM, Arzt M (2018) Association of sleep-disordered breathing with severe chronic vascular disease in patients with type 2 diabetes. Sleep Med 48:53–60. https://doi.org/10.1016/j.sleep.2018.05.001
Wu KL, Kuo CY, Tsai YC, Hung JY, Sheu CC, Yang CJ, Hsu CY, Wu MN, Tsai MJ (2019) CHADS2, CHA2DS2ASc, and new ABCD scores predict the risk of peripheral arterial disease in patients with sleep apnea. J Clin Med 8(2). https://doi.org/10.3390/jcm8020188
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of Observational Studies in Epidemiology (MOOSE) group. JAMA 283(15):2008–2012
Higgins J, Green S (2011) Cochrane handbook for systematic reviews of interventions version 5.1.0. The Cochrane Collaboration. www.cochranehandbook.org. Accessed 30 Oct 2019
Mohammadieh A, Sutherland K, Cistulli PA (2017) Sleep disordered breathing: management update. Intern Med J 47(11):1241–1247. https://doi.org/10.1111/imj.13606
Conte MS, Bradbury AW, Kolh P, White JV, Dick F, Fitridge R, Mills JL, Ricco JB, Suresh KR, Murad MH, Aboyans V, Aksoy M, Alexandrescu VA, Armstrong D, Azuma N, Belch J, Bergoeing M, Bjorck M, Chakfe N, Cheng S, Dawson J, Debus ES, Dueck A, Duval S, Eckstein HH, Ferraresi R, Gambhir R, Garguilo M, Geraghty P, Goode S, Gray B, Guo W, Gupta PC, Hinchliffe R, Jetty P, Komori K, Lavery L, Liang W, Lookstein R, Menard M, Misra S, Miyata T, Moneta G, Munoa Prado JA, Munoz A, Paolini JE, Patel M, Pomposelli F, Powell R, Robless P, Rogers L, Schanzer A, Schneider P, Taylor S, De Ceniga MV, Veller M, Vermassen F, Wang J, Wang S (2019) Global vascular guidelines on the management of chronic limb-threatening ischemia. Eur J Vasc Endovasc Surg 58(1S):S1–S109 e133. https://doi.org/10.1016/j.ejvs.2019.05.006
Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, Tugwell P (2010) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 30 Oct 2019
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558. https://doi.org/10.1002/sim.1186
Patsopoulos NA, Evangelou E, Ioannidis JP (2008) Sensitivity of between-study heterogeneity in meta-analysis: proposed metrics and empirical evaluation. Int J Epidemiol 37(5):1148–1157. https://doi.org/10.1093/ije/dyn065
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634
Joyeux-Faure M, Tamisier R, Borel JC, Millasseau S, Galerneau LM, Destors M, Bailly S, Pepin JL (2018) Contribution of obstructive sleep apnoea to arterial stiffness: a meta-analysis using individual patient data. Thorax 73(12):1146–1151. https://doi.org/10.1136/thoraxjnl-2018-211513
Gunduz C, Basoglu OK, Hedner J, Zou D, Bonsignore MR, Hein H, Staats R, Pataka A, Barbe F, Sliwinski P, Kent BD, Pepin JL, Grote L (2018) Obstructive sleep apnoea independently predicts lipid levels: data from the European Sleep Apnea Database. Respirology 23(12):1180–1189. https://doi.org/10.1111/resp.13372
Priou P, Le Vaillant M, Meslier N, Chollet S, Masson P, Humeau MP, Pigeanne T, Bizieux-Thaminy A, Goupil F, Gagnadoux F (2012) Independent association between obstructive sleep apnea severity and glycated hemoglobin in adults without diabetes. Diabetes Care 35(9):1902–1906. https://doi.org/10.2337/dc11-2538
Kurosawa H, Saisho Y, Fukunaga K, Haraguchi M, Yamasawa W, Kurihara I, Betsuyaku T, Itoh H (2018) Association between severity of obstructive sleep apnea and glycated hemoglobin level in Japanese individuals with and without diabetes. Endocr J 65(1):121–127. https://doi.org/10.1507/endocrj.EJ17-0356
Lombardi C, Pengo MF, Parati G (2019) Obstructive sleep apnea syndrome and autonomic dysfunction. Auton Neurosci 221:102563. https://doi.org/10.1016/j.autneu.2019.102563
Ghadami MR (2018) Hypercoagulability and severe obstructive sleep apnea. JAMA Otolaryngol Head Neck Surg 144(2):175. https://doi.org/10.1001/jamaoto.2017.2761
Toraldo DM, De Benedetto M, Scoditti E, De Nuccio F (2016) Obstructive sleep apnea syndrome: coagulation anomalies and treatment with continuous positive airway pressure. Sleep Breath 20(2):457–465. https://doi.org/10.1007/s11325-015-1227-6
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval and informed consent
This article does not contain any studies with human participants performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 326 kb).
Rights and permissions
About this article
Cite this article
Chen, Y., Li, X., Zhao, L. et al. Association between sleep-disordered breathing and lower extremity artery disease: a meta-analysis. Sleep Breath 25, 227–236 (2021). https://doi.org/10.1007/s11325-020-02096-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-020-02096-z