Abstract
Background
On initiation of long-term non-invasive ventilation (NIV), intermittent upper airway obstruction has rarely been described as possibly treatment-induced. Inspiratory pressure effects and the use of an oronasal interface may promote obstructive events in some patients with neuromuscular disease (NMD) and amyotrophic lateral sclerosis (ALS) in particular.
Methods
We evaluated clinical data from 212 patients in whom NIV was initiated using an oronasal mask. Treatment-induced upper airway obstruction (TAO) was defined as an AHI > 5/h along with a relative increase of the AHI in the first treatment night compared to diagnostic sleep studies.
Results
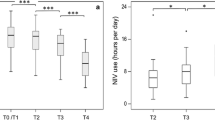
Prevalence of TAO was 14.2% in the entire cohort, 17.0% in patients with NMD (n = 165), 20.4% in the ALS subgroup (n = 93), and 4.3% in non-NMD patients (n = 47). Fixed expiratory positive airway pressure (EPAP, n = 192) was significantly correlated with AHI reduction (r = 0.50; p < 0.001). The inspiratory-expiratory pressure interval (∆PAP, n = 191) showed inverse correlation with the AHI change achieved in the first treatment night (r = − 0.28; p < 0.001). However, ∆PAP and the effective pressure range between EPAP and the highest inspiratory PAP achieved were not predictive of TAO. In patients with ALS, TAO was associated with better bulbar function. Study results were limited by initial EPAP being significantly lower in NMD patients reflecting that sleep apnea was less frequent and severe in this subgroup.
Conclusions
Initiation of NIV using an oronasal interface may be associated with TAO in a subset of patients. Since both EPAP and ∆PAP appear to play a causative role, careful titration of ventilator settings is recommended.

Similar content being viewed by others
References
Teo M, Amis T, Lee S, Falland K, Lambert S, Wheatley J (2011) Equivalence of nasal and oronasal masks during initial CPAP titration for obstructive sleep apnea syndrome. Sleep 34(7):951–955
Teschler H, Stampa J, Ragette R, Konietzko N, Berthon-Jones M (1999) Effect of mouth leak on effectiveness of nasal bilevel ventilatory assistance and sleep architecture. Eur Respir J 14(6):1251–1257
Gonzalez-Bermejo J, Perrin C, Janssens JP, Pepin JL, Mroue G, Leger P et al (2012) Proposal for a systematic analysis of polygraphy or polysomnography for identifying and scoring abnormal events occurring during non-invasive ventilation. Thorax 67(6):546–552
Ebben MR, Narizhnaya M, Segal AZ, Barone D, Krieger AC (2014) A randomised controlled trial on the effect of mask choice on residual respiratory events with continuous positive airway pressure treatment. Sleep Med 15(6):619–624
Bakker JP, Neill AM, Campbell AJ (2012) Nasal versus oronasal continuous positive airway pressure masks for obstructive sleep apnea: a pilot investigation of pressure requirement, residual disease, and leak. Sleep Breath 16(3):709–716
Vrijsen B, Buyse B, Belge C, Testelmans D (2014) Upper airway obstruction during noninvasive ventilation induced by the use of an oronasal mask. J Clin Sleep Med 10(9):1033–1035
Georges M, Attali V, Golmard JL, Morelot-Panzini C, Crevier-Buchman L, Collet JM et al (2016) Reduced survival in patients with ALS with upper airway obstructive events on non-invasive ventilation. J Neurol Neurosurg Psychiatry 87(10):1045–1050
(1999) Clinical indications for noninvasive positive pressure ventilation in chronic respiratory failure due to restrictive lung disease, COPD, and nocturnal hypoventilation--a consensus conference report. Chest 116(2):521–534
Windisch W, Walterspacher S, Siemon K, Geiseler J, Sitter H (2010) Guidelines for non-invasive and invasive mechanical ventilation for treatment of chronic respiratory failure. Published by the German Society for Pneumology (DGP). Pneumologie 64(10):640–652
Cedarbaum JM, Stambler N, Malta E, Fuller C, Hilt D, Thurmond B, Nakanishi A (1999) The ALSFRS-R: a revised ALS functional rating scale that incorporates assessments of respiratory function. BDNF ALS Study Group (Phase III). J Neurol Sci 169(1–2):13–21
Berry RB, Brooks R, Gamaldo CE, Harding SM, Lloyd RM, Marcus CL, Vaughn BV for the American Academy of Sleep Medicine (2015) The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications, Version 2.2. American Academy of Sleep Medicine, Darien http://www.aasmnet.org
BaHammam AS, Singh T, George S, Acosta KL, Barataman K, Gacuan DE (2017) Choosing the right interface for positive airway pressure therapy in patients with obstructive sleep apnea. Sleep Breath 21:569–575
Fanfulla F, Delmastro M, Berardinelli A, Lupo ND, Nava S (2005) Effects of different ventilator settings on sleep and inspiratory effort in patients with neuromuscular disease. Am J Respir Crit Care Med 172(5):619–624
Boentert M, Glatz C, Helmle C, Okegwo A, Young P (2017) Prevalence of sleep apnoea and capnographic detection of nocturnal hypoventilation in amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry. https://doi.org/10.1136/jnnp-2017-316515
Santos C, Braghiroli A, Mazzini L, Pratesi R, Oliveira LV, Mora G (2003) Sleep-related breathing disorders in amyotrophic lateral sclerosis. Monaldi archives for chest disease = Archivio Monaldi per le malattie del torace/Fondazione clinica del lavoro, IRCCS [and] Istituto di clinica tisiologica e malattie apparato respiratorio, Universita di Napoli, Secondo ateneo 59(2):160–5
Guilleminault C, Philip P, Robinson A (1998) Sleep and neuromuscular disease: bilevel positive airway pressure by nasal mask as a treatment for sleep disordered breathing in patients with neuromuscular disease. J Neurol Neurosurg Psychiatry 65(2):225–232
Ramirez A, Khirani S, Aloui S, Delord V, Borel JC, Pepin JL et al (2013) Continuous positive airway pressure and noninvasive ventilation adherence in children. Sleep Med 14(12):1290–1294
Robertson PL, Roloff DW (1994) Chronic respiratory failure in limb-girdle muscular dystrophy: successful long-term therapy with nasal bilevel positive airway pressure. Pediatr Neurol 10(4):328–331
Kirkness JP, Peterson LA, Squier SB, McGinley BM, Schneider H, Meyer A et al (2011) Performance characteristics of upper airway critical collapsing pressure measurements during sleep. Sleep 34(4):459–467
Berry RB, Chediak A, Brown LK, Finder J, Gozal D, Iber C, Kushida CA, Morgenthaler T, Rowley JA, Davidson-Ward SL, NPPV Titration Task Force of the American Academy of Sleep Medicine (2010) Best clinical practices for the sleep center adjustment of noninvasive positive pressure ventilation (NPPV) in stable chronic alveolar hypoventilation syndromes. J Clin Sleep Med 6(5):491–509
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Contributions
VS, CG, MB, AH, AO, and IB were responsible for data collection. MB and VS performed the statistical analyses. MB, VS, and PY prepared the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
PY has received speaker honoraria and financial research support from the Löwenstein Foundation, Bad Ems, Germany. All other authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
This study was approved by the local ethics authority.
Rights and permissions
About this article
Cite this article
Schellhas, V., Glatz, C., Beecken, I. et al. Upper airway obstruction induced by non-invasive ventilation using an oronasal interface. Sleep Breath 22, 781–788 (2018). https://doi.org/10.1007/s11325-018-1640-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-018-1640-8