Abstract
Purpose
Hypocitraturia is an important cause of urolithiasis. Exploring the characteristics of the gut microbiome (GMB) of hypocitriuria urolithiasis (HCU) patients can provide new ideas for the treatment and prevention of urolithiasis.
Methods
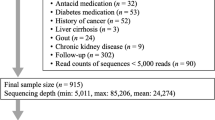
The 24 h urinary citric acid excretion of 19 urolithiasis patients was measured, and patients were divided into the HCU group and the normal citrate urolithiasis (NCU) group. The 16 s ribosomal RNA (rRNA) was used to detect GMB composition differences and construct operational taxonomic units (OTUs) coexistence networks. The key bacterial community was determined by Lefse analysis, Metastats analysis and RandomForest analysis. Redundancy analysis (RDA) and Pearson correlation analysis visualized the correlation between key OTUs and clinical features and then established the disease diagnosis model of microbial-clinical indicators. Finally, PICRUSt2 was used to explore the metabolic pathway of related GMB in HCU patients.
Results
The alpha diversity of GMB in HCU group was increased and Beta diversity analysis suggested significant differences between HCU and NCU groups, which was related to renal function damage and urinary tract infection. Ruminococcaceae_ge and Turicibacter are the characteristic bacterial groups of HCU. Correlation analysis showed that the characteristic bacterial groups were significantly associated with various clinical features. Based on this, the diagnostic models of microbiome-clinical indicators in HCU patients were constructed with the areas under the curve (AUC) of 0.923 and 0.897, respectively. Genetic and metabolic processes of HCU are affected by changes in GMB abundance.
Conclusion
GMB disorder may be involved in the occurrence and clinical characteristics of HCU by influencing genetic and metabolic pathways. The new microbiome-clinical indicator diagnostic model is effective.







Similar content being viewed by others
References
Zuckerman JM, Assimos DG (2009) Hypocitraturia: pathophysiology and medical management. Rev Urol 11(3):134–144
Sakhaee K et al (2011) Nephrolithiasis-associated bone disease: pathogenesis and treatment options. Kidney Int 79(4):393–403
Arrabal-Polo MA et al (2013) Importance of citrate and the calcium : citrate ratio in patients with calcium renal lithiasis and severe lithogenesis. BJU Int 111(4):622–627
Lan Y et al (2021) Glycine suppresses kidney calcium oxalate crystal depositions via regulating urinary excretions of oxalate and citrate. J Cell Physiol 236(10):6824–6835
Osis G et al (2019) Regulation of renal NaDC1 expression and citrate excretion by NBCe1-A. Am J Physiol Renal Physiol 317(2):F489–F501
Siener R et al (2013) The role of Oxalobacter formigenes colonization in calcium oxalate stone disease. Kidney Int 83(6):1144–1149
Ormanji MS, Rodrigues FG, Heilberg IP (2020) Dietary recommendations for bariatric patients to prevent kidney stone formation. Nutrients 12(5):1442
Pak CY et al (1985) Long-term treatment of calcium nephrolithiasis with potassium citrate. J Urol 134(1):11–19
Tian L et al (2022) Lactiplantibacillus plantarum J-15 reduced calcium oxalate kidney stones by regulating intestinal microbiota, metabolism, and inflammation in rats. FASEB J 36(6):e22340
Piper HG et al (2017) Severe gut microbiota dysbiosis is associated with poor growth in patients with short bowel syndrome. JPEN J Parenter Enteral Nutr 41(7):1202–1212
Mortera P et al (2013) Ca2+-citrate uptake and metabolism in Lactobacillus casei ATCC 334. Appl Environ Microbiol 79(15):4603–4612
Martino GP et al (2016) Aroma compounds generation in citrate metabolism of Enterococcus faecium: genetic characterization of type I citrate gene cluster. Int J Food Microbiol 218:27–37
Miller AW et al (2019) Inhibition of urinary stone disease by a multi-species bacterial network ensures healthy oxalate homeostasis. Kidney Int 96(1):180–188
Rognes T et al (2016) VSEARCH: a versatile open source tool for metagenomics. PeerJ 4:e2584
Chen S et al (2018) fastp: an ultra-fast all-in-one FASTQ preprocessor. Bioinformatics 34(17):i884–i890
Edgar RC (2013) UPARSE: highly accurate OTU sequences from microbial amplicon reads. Nat Methods 10(10):996–998
Hagerty SL et al (2020) An empirically derived method for measuring human gut microbiome alpha diversity: demonstrated utility in predicting health-related outcomes among a human clinical sample. PLoS One 15(3):e0229204
Mori AS, Isbell F, Seidl R (2018) β-diversity, community assembly, and ecosystem functioning. Trends Ecol Evol 33(7):549–564
White JR, Nagarajan N, Pop M (2009) Statistical methods for detecting differentially abundant features in clinical metagenomic samples. PLoS Comput Biol 5(4):e1000352
Segata N et al (2011) Metagenomic biomarker discovery and explanation. Genome Biol 12(6):R60
Capblancq T et al (2018) Evaluation of redundancy analysis to identify signatures of local adaptation. Mol Ecol Resour 18(6):1223–1233
Speiser JL et al (2019) A comparison of random forest variable selection methods for classification prediction modeling. Expert Syst Appl 134:93–101
Douglas GM, Beiko RG, Langille M (2018) Predicting the functional potential of the microbiome from marker genes using PICRUSt. Methods Mol Biol 1849:169–177
Parks DH et al (2014) STAMP: statistical analysis of taxonomic and functional profiles. Bioinformatics 30(21):3123–3124
Wang LL et al (2020) A novel approach for the forensic diagnosis of drowning by microbiological analysis with next-generation sequencing and unweighted UniFrac-based PCoA. Int J Legal Med 134(6):2149–2159
Pérez-Enciso M, Tenenhaus M (2003) Prediction of clinical outcome with microarray data: a partial least squares discriminant analysis (PLS-DA) approach. Hum Genet 112(5–6):581–592
Sanapareddy N et al (2012) Increased rectal microbial richness is associated with the presence of colorectal adenomas in humans. ISME J 6(10):1858–1868
Xu Z et al (2020) Gut microbiome reveals specific dysbiosis in primary osteoporosis. Front Cell Infect Microbiol 10:160
Hong SY et al (2023) The role of microbiome: a novel insight into urolithiasis. Crit Rev Microbiol 49(2):177–196
Robijn S et al (2011) Hyperoxaluria: a gut-kidney axis. Kidney Int 80(11):1146–1158
Ticinesi A, Nouvenne A, Meschi T (2019) Gut microbiome and kidney stone disease: not just an Oxalobacter story. Kidney Int 96(1):25–27
Tasian G, Miller A, Lange D (2019) Antibiotics and kidney stones: perturbation of the gut-kidney axis. Am J Kidney Dis 74(6):724–726
Goraya N et al (2019) Urine citrate excretion as a marker of acid retention in patients with chronic kidney disease without overt metabolic acidosis. Kidney Int 95(5):1190–1196
Goraya N et al (2019) Urine citrate excretion identifies changes in acid retention as eGFR declines in patients with chronic kidney disease. Am J Physiol Renal Physiol 317(2):F502–F511
Song Y et al (2016) Potassium citrate decreases urine calcium excretion in patients with hypocitraturic calcium oxalate nephrolithiasis. Urolithiasis 44(2):145–148
Strohmaier WL, Seilnacht J, Schubert G (2012) Urinary stone formers with hypocitraturia and ‘normal’ urinary pH are at high risk for recurrence. Urol Int 88(3):294–297
Zhao E et al (2021) Intestinal dysbacteriosis leads to kidney stone disease. Mol Med Rep. https://doi.org/10.3892/mmr.2020.11819
Wang L et al (2022) Preventive effects of the Rehmannia glutinosa Libosch and Cornus officinalis Sieb herb couple on chronic kidney disease rats via modulating the intestinal microbiota and enhancing the intestinal barrier. Front Pharmacol 13:942032
Ho HJ et al (2021) SGLT-1-specific inhibition ameliorates renal failure and alters the gut microbial community in mice with adenine-induced renal failure. Physiol Rep 9(24):e15092
Liu Y et al (2020) The relationship between gut microbiota and short chain fatty acids in the renal calcium oxalate stones disease. FASEB J 34(8):11200–11214
Chen R et al (2022) Gut microbiota diversity in middle-aged and elderly patients with end-stage diabetic kidney disease. Ann Transl Med 10(13):750
Wang X et al (2022) Modified Baihu decoction therapeutically remodels gut microbiota to inhibit acute gouty arthritis. Front Physiol 13:1023453
Tang R et al (2018) 16S rRNA gene sequencing reveals altered composition of gut microbiota in individuals with kidney stones. Urolithiasis 46(6):503–514
Amatjan M et al (2023) A novel approach based on gut microbiota analysis and network pharmacology to explain the mechanisms of action of Cichorium intybus L. formula in the improvement of hyperuricemic nephropathy in rats. Drug Des Devel Ther 17:107–128
Chen H et al (2022) Establishment and analysis of a disease risk prediction model for the systemic lupus erythematosus with random forest. Front Immunol 13:1025688
Ouyang D et al (2022) Prognostic analysis of pT1-T2aN0M0 cervical adenocarcinoma based on random survival forest analysis and the generation of a predictive nomogram. Front Oncol 12:1049097
Yu M et al (2022) Understanding the gut-kidney axis in antineutrophil cytoplasmic antibody-associated vasculitis: an analysis of gut microbiota composition. Front Pharmacol 13:783679
Jiang Q et al (2018) Altered gut microbiome promotes proteinuria in mice induced by Adriamycin. AMB Express 8(1):31
Pak CY (1994) Citrate and renal calculi: an update. Miner Electrolyte Metab 20(6):371–377
Leslie SW, Sajjad H, Bashir K (2023) 24-Hour Urine testing for nephrolithiasis: interpretation guideline. Treasure Island (FL)
Adak A, Khan MR (2019) An insight into gut microbiota and its functionalities. Cell Mol Life Sci 76(3):473–493
Baruch SB et al (1975) Renal metabolism of citrate. Med Clin North Am 59(3):569–582
Mycielska ME, James EN, Parkinson EK (2022) Metabolic alterations in cellular senescence: the role of citrate in ageing and age-related disease. Int J Mol Sci 23(7):3652
Mohammadi A et al (2022) Genetic polymorphisms and kidney stones around the globe: a systematic review and meta-analysis. Front Genet 13:913908
Jv M et al (2023) Genetic mutation of SLC6A20 (c.1072T > C) in a family with nephrolithiasis: a case report. Open Med (Wars) 18(1):20230648
Ullah I et al (2022) Association study of CLDN14 variations in patients with kidney stones. Open Life Sci 17(1):81–92
Funding
This research was funded by the Natural Science Foundation of Fujian Province (2022J01273, 2020J01222), and the Training Project of Young Talents in Fujian Provincial Health System (2019-ZQNB-9).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, J., Chen, G., Chen, H. et al. Exploring the characteristics of gut microbiome in patients of Southern Fujian with hypocitraturia urolithiasis and constructing clinical diagnostic models. Int Urol Nephrol 55, 1917–1929 (2023). https://doi.org/10.1007/s11255-023-03662-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03662-6