Abstract
Purpose
Despite CKD is common among older patients, and although factors associated with CKD progression have been explored over decades, little is known about the decline of renal function specifically in older individuals.
Methods
We included adult patients with CKD on conservative management in a propensity-score matched study 1:1 older (> 65 year) and young (≤ 65 yr). Factors associated with the slope of the decline of eGFR such as proteinuria, initial eGFR, diabetes, sex, and use of angiotensin-converting enzyme inhibitor/angiotensin receptor block (ACEI/ARB) were analyzed. Inclusion criteria were at least two consultations in the service and an initial eGFR lower than 45 ml/min/m2, in the period between January 2012 and December 2017.
Results
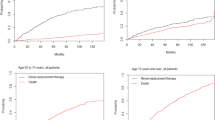
Crude analysis of eGFR decline shows a slower progression of older patients when compared to younger patients in both absolute change [− 2.0 (− 4.5, − 1.0) vs. -3.0 (− 7.0, − 1.0) ml/min/1.73m2, p < 0.001] and slope of eGFR reduction [− 2.2 (− 4.4, − 1.0) vs. 3.1 (− 6.7, − 1.2)) ml/min/1.73m2, p < 0.001]. Patients considered fast progressors (> 5 ml/min/1.73 m2/year decline in eGFR) were less likely to be older (35.2% young vs. 22.0% older, p < 0.001). Adjusted logistic multivariate regression confirmed that older patients had less odds ratio of eGFR decline, independently of the presence of proteinuria, diabetes, ACEI/ARB use, sex, baseline eGFR, baseline phosphate and baseline 25(OH) vitamin D.
Conclusion
Older patients present slower CKD progression even after multiple adjustments. This information should be taken into consideration while treating these patients on conservative management and should be kept in mind while planning dialysis start.



Similar content being viewed by others
Data availability
Data analyzed in the current study is available to authors upon reasonable request.
References
Nations U (2019) Our world is growing older: UN DESA releases new report on ageing. https://www.un.org/development/desa/en/news/population/our-world-is-growing-older.html.
Collaboration GBDCKD (2020) Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 395(10225):709–733. https://doi.org/10.1016/S0140-6736(20)30045-3
Zatz R, Fujihara CK (2002) Mechanisms of progressive renal disease: role of angiotensin II, cyclooxygenase products and nitric oxide. J Hypertens Suppl 20(3):S37-44
Minakuchi H, Wakino S, Urai H, Kurokochi A, Hasegawa K, Kanda T, Tokuyama H, Itoh H (2020) The effect of aldosterone and aldosterone blockade on the progression of chronic kidney disease: a randomized placebo-controlled clinical trial. Sci Rep 10(1):16626. https://doi.org/10.1038/s41598-020-73638-4
Badve SV, Pascoe EM, Tiku A, Boudville N, Brown FG, Cass A, Clarke P, Dalbeth N, Day RO, de Zoysa JR, Douglas B, Faull R, Harris DC, Hawley CM, Jones GRD, Kanellis J, Palmer SC, Perkovic V, Rangan GK, Reidlinger D, Robison L, Walker RJ, Walters G, Johnson DW, Investigators C-FS (2020) Effects of allopurinol on the progression of chronic kidney disease. N Engl J Med 382(26):2504–2513. https://doi.org/10.1056/NEJMoa1915833
Cherney DZI, Dekkers CCJ, Barbour SJ, Cattran D, Abdul Gafor AH, Greasley PJ, Laverman GD, Lim SK, Di Tanna GL, Reich HN, Vervloet MG, Wong MG, Gansevoort RT, Heerspink HJL, investigators D, (2020) Effects of the SGLT2 inhibitor dapagliflozin on proteinuria in non-diabetic patients with chronic kidney disease (DIAMOND): a randomised, double-blind, crossover trial. Lancet Diabetes Endocrinol 8(7):582–593. https://doi.org/10.1016/S2213-8587(20)30162-5
de Boer IH, Zelnick LR, Ruzinski J, Friedenberg G, Duszlak J, Bubes VY, Hoofnagle AN, Thadhani R, Glynn RJ, Buring JE, Sesso HD, Manson JE (2019) Effect of vitamin d and omega-3 fatty acid supplementation on kidney function in patients with type 2 diabetes: a randomized clinical trial. JAMA 322(19):1899–1909. https://doi.org/10.1001/jama.2019.17380
Melamed ML, Horwitz EJ, Dobre MA, Abramowitz MK, Zhang L, Lo Y, Mitch WE, Hostetter TH (2020) Effects of sodium bicarbonate in ckd stages 3 and 4: a randomized, placebo-controlled, multicenter clinical trial. Am J Kidney Dis 75(2):225–234. https://doi.org/10.1053/j.ajkd.2019.07.016
Inker LA, Astor BC, Fox CH, Isakova T, Lash JP, Peralta CA, Kurella Tamura M, Feldman HI (2014) KDOQI US commentary on the 2012 KDIGO clinical practice guideline for the evaluation and management of CKD. Am J Kidney Dis 63(5):713–735. https://doi.org/10.1053/j.ajkd.2014.01.416
O’Hare AM, Choi AI, Bertenthal D, Bacchetti P, Garg AX, Kaufman JS, Walter LC, Mehta KM, Steinman MA, Allon M, McClellan WM, Landefeld CS (2007) Age affects outcomes in chronic kidney disease. J Am Soc Nephrol 18(10):2758–2765. https://doi.org/10.1681/ASN.2007040422
Totoli C, Carvalho AB, Ammirati AL, Draibe SA, Canziani MEF (2019) Associated factors related to chronic kidney disease progression in elderly patients. PLoS ONE 14(7):e0219956. https://doi.org/10.1371/journal.pone.0219956
Kanda E, Ai M, Yoshida M, Kuriyama R, Shiigai T (2013) High serum bicarbonate level within the normal range prevents the progression of chronic kidney disease in elderly chronic kidney disease patients. BMC Nephrol 14:4. https://doi.org/10.1186/1471-2369-14-4
Heras M, Fernandez-Reyes MJ, Sanchez R, Guerrero MT, Molina A, Rodriguez MA, Alvarez-Ude F (2012) Elderly patients with chronic kidney disease: outcomes after 5 years of follow-up. Nefrologia 32(3):300–305. https://doi.org/10.3265/Nefrologia.pre2012.Jan.10994
Shojamoradi MH, Saberi Isfeedvajani M, Mahdavi-Mazdeh M, Ahmadi F, Gatmiri SM, Abbasi Larki R (2014) Chronic kidney disease progression in elderly Iranian patients: a cohort study. Nephrourol Mon 6(5):e20748. https://doi.org/10.5812/numonthly.20748
Chapter 2: Definition, identification, and prediction of CKD progression (2013). Kidney Int Suppl (2011) 3 (1):63–72. https://doi.org/10.1038/kisup.2012.65
Thoemmes F (2012) Propensity score matching in SPSS.
de Zeeuw D, Remuzzi G, Parving HH, Keane WF, Zhang Z, Shahinfar S, Snapinn S, Cooper ME, Mitch WE, Brenner BM (2004) Proteinuria, a target for renoprotection in patients with type 2 diabetic nephropathy: lessons from RENAAL. Kidney Int 65(6):2309–2320. https://doi.org/10.1111/j.1523-1755.2004.00653.x
Chen W, Abramowitz MK (2014) Metabolic acidosis and the progression of chronic kidney disease. BMC Nephrol 15:55. https://doi.org/10.1186/1471-2369-15-55
Chen W, Levy DS, Abramowitz MK (2019) Acid Base Balance and Progression of Kidney Disease. Semin Nephrol 39(4):406–417. https://doi.org/10.1016/j.semnephrol.2019.04.009
Swartling O, Rydell H, Stendahl M, Segelmark M, Trolle Lagerros Y, Evans M (2021) CKD progression and mortality among men and women: a nationwide study in Sweden. Am J Kidney Dis 78(2):190–199. https://doi.org/10.1053/j.ajkd.2020.11.026
Carrero JJ, Hecking M, Ulasi I, Sola L, Thomas B (2017) Chronic kidney disease, gender, and access to care: a global perspective. Semin Nephrol 37(3):296–308. https://doi.org/10.1016/j.semnephrol.2017.02.009
Garcia GG, Iyengar A, Kaze F, Kierans C, Padilla-Altamira C, Luyckx VA (2022) Sex and gender differences in chronic kidney disease and access to care around the globe. Semin Nephrol 42(2):101–113. https://doi.org/10.1016/j.semnephrol.2022.04.001
Mallamaci F, Ruggenenti P, Perna A, Leonardis D, Tripepi R, Tripepi G, Remuzzi G, Zoccali C, Group RS (2011) ACE inhibition is renoprotective among obese patients with proteinuria. J Am Soc Nephrol 22(6):1122–1128. https://doi.org/10.1681/ASN.2010090969
Appel LJ, Wright JT, Jr., Greene T, Kusek JW, Lewis JB, Wang X, Lipkowitz MS, Norris KC, Bakris GL, Rahman M, Contreras G, Rostand SG, Kopple JD, Gabbai FB, Schulman GI, Gassman JJ, Charleston J, Agodoa LY, African American Study of Kidney D, Hypertension Collaborative Research G (2008) Long-term effects of renin-angiotensin system-blocking therapy and a low blood pressure goal on progression of hypertensive chronic kidney disease in African Americans. Arch Intern Med 168(8):832–839. https://doi.org/10.1001/archinte.168.8.832
Tylicki L, Rutkowski P, Renke M, Larczynski W, Aleksandrowicz E, Lysiak-Szydlowska W, Rutkowski B (2008) Triple pharmacological blockade of the renin-angiotensin-aldosterone system in nondiabetic CKD: an open-label crossover randomized controlled trial. Am J Kidney Dis 52(3):486–493. https://doi.org/10.1053/j.ajkd.2008.02.297
Titan SM, M. Vieira J J, Dominguez WV, Barros RT, Zatz R, (2011) ACEI and ARB combination therapy in patients with macroalbuminuric diabetic nephropathy and low socioeconomic level: a double-blind randomized clinical trial. Clin Nephrol 76(4):273–283. https://doi.org/10.5414/cn107013
Anderson S, Rennke HG, Zatz R (1994) Glomerular adaptations with normal aging and with long-term converting enzyme inhibition in rats. Am J Physiol 267(1 Pt 2):F35-43. https://doi.org/10.1152/ajprenal.1994.267.1.F35
Zatz R, Dunn BR, Meyer TW, Anderson S, Rennke HG, Brenner BM (1986) Prevention of diabetic glomerulopathy by pharmacological amelioration of glomerular capillary hypertension. J Clin Invest 77(6):1925–1930. https://doi.org/10.1172/JCI112521
Fu EL, Clase CM, Evans M, Lindholm B, Rotmans JI, Dekker FW, van Diepen M, Carrero JJ (2021) Comparative effectiveness of renin-angiotensin system inhibitors and calcium channel blockers in individuals with advanced ckd: a nationwide observational cohort study. Am J Kidney Dis 77(5):719–729. https://doi.org/10.1053/j.ajkd.2020.10.006
Martinez-Milla J, Garcia MC, Urquia MT, Castillo ML, Arbiol AD, Monteagudo ALR, Mariscal MLM, Figuero SB, Franco-Pelaez JA, Tunon J (2019) Blockade of renin-angiotensin-aldosterone system in elderly patients with heart failure and chronic kidney disease: results of a single-center. Observational Cohort Study Drugs Aging 36(12):1123–1131. https://doi.org/10.1007/s40266-019-00709-1
Pecoits-Filho R, Fliser D, Tu C, Zee J, Bieber B, Wong MMY, Port F, Combe C, Lopes AA, Reichel H, Narita I, Stengel B, Robinson BM, Massy Z, Investigators CK (2019) Prescription of renin-angiotensin-aldosterone system inhibitors (RAASi) and its determinants in patients with advanced CKD under nephrologist care. J Clin Hypertens (Greenwich) 21(7):991–1001. https://doi.org/10.1111/jch.13563
Dos Santos MS, Canale D, Bernardo DRD, Shimizu MHM, Seguro AC, Volpini RA, de Braganca AC (2021) The restoration of vitamin D levels slows the progression of renal ischemic injury in rats previously deficient in vitamin D. Front Med (Lausanne) 8:625647. https://doi.org/10.3389/fmed.2021.625647
Dall’Agnol A, Brondani LA, Cancelier VDA, Camargo EG, Silveiro SP (2020) Lower serum 25-hydroxyvitamin D levels are associated with impaired glomerular filtration rate in type 2 diabetes patients. Ther Adv Endocrinol Metab 11:2042018820930904. https://doi.org/10.1177/2042018820930904
Isakova T, Cai X, Lee J, Mehta R, Zhang X, Yang W, Nessel L, Anderson AH, Lo J, Porter A, Nunes JW, Negrea L, Hamm L, Horwitz E, Chen J, Scialla JJ, de Boer IH, Leonard MB, Feldman HI, Wolf M, Investigators CS (2020) longitudinal evolution of markers of mineral metabolism in patients with CKD: the chronic renal insufficiency cohort (CRIC) study. Am J Kidney Dis 75(2):235–244. https://doi.org/10.1053/j.ajkd.2019.07.022
de Boer IH, Ioannou GN, Kestenbaum B, Brunzell JD, Weiss NS (2007) 25-Hydroxyvitamin D levels and albuminuria in the Third National Health and Nutrition Examination Survey (NHANES III). Am J Kidney Dis 50(1):69–77. https://doi.org/10.1053/j.ajkd.2007.04.015
Zehnder D, Quinkler M, Eardley KS, Bland R, Lepenies J, Hughes SV, Raymond NT, Howie AJ, Cockwell P, Stewart PM, Hewison M (2008) Reduction of the vitamin D hormonal system in kidney disease is associated with increased renal inflammation. Kidney Int 74(10):1343–1353. https://doi.org/10.1038/ki.2008.453
Duayer IF, Duque EJ, Fujihara CK, de Oliveira IB, Dos Reis LM, Machado FG, Graciolli FG, Jorgetti V, Zatz R, Elias RM, Moyses RMA (2021) The protein-independent role of phosphate in the progression of chronic kidney disease. Toxins (Basel). https://doi.org/10.3390/toxins13070503
Radloff J, Latic N, Pfeiffenberger U, Schuler C, Tangermann S, Kenner L, Erben RG (2021) A phosphate and calcium-enriched diet promotes progression of 5/6-nephrectomy-induced chronic kidney disease in C57BL/6 mice. Sci Rep 11(1):14868. https://doi.org/10.1038/s41598-021-94264-8
Shiizaki K, Tsubouchi A, Miura Y, Seo K, Kuchimaru T, Hayashi H, Iwazu Y, Miura M, Battulga B, Ohno N, Hara T, Kunishige R, Masutani M, Negishi K, Kario K, Kotani K, Yamada T, Nagata D, Komuro I, Itoh H, Kurosu H, Murata M, Kuro OM (2021) Calcium phosphate microcrystals in the renal tubular fluid accelerate chronic kidney disease progression. J Clin Invest. https://doi.org/10.1172/JCI145693
Bidulka P, Fu EL, Leyrat C, Kalogirou F, McAllister KSL, Kingdon EJ, Mansfield KE, Iwagami M, Smeeth L, Clase CM, Bhaskaran K, van Diepen M, Carrero JJ, Nitsch D, Tomlinson LA (2020) Stopping renin-angiotensin system blockers after acute kidney injury and risk of adverse outcomes: parallel population-based cohort studies in English and Swedish routine care. BMC Med 18(1):195. https://doi.org/10.1186/s12916-020-01659-x
Witham MD, Lamb EJ (2016) Should chronic metabolic acidosis be treated in older people with chronic kidney disease? Nephrol Dial Transplant 31(11):1796–1802. https://doi.org/10.1093/ndt/gfv344
Ricardo AC, Yang W, Sha D, Appel LJ, Chen J, Krousel-Wood M, Manoharan A, Steigerwalt S, Wright J, Rahman M, Rosas SE, Saunders M, Sharma K, Daviglus ML, Lash JP, Investigators C (2019) Sex-related disparities in CKD progression. J Am Soc Nephrol 30(1):137–146. https://doi.org/10.1681/ASN.2018030296
da Silva SL, Rech DL, de Souza V, Iwaz J, Lemoine S, Dubourg L (2019) Diagnostic performance of creatinine-based equations for estimating glomerular filtration rate in adults 65 years and older. JAMA Intern Med 179(6):796–804. https://doi.org/10.1001/jamainternmed.2019.0223
Coelho VA, Santos GG, Avesani CM, Bezerra CIL, Silva LCA, Lauar JC, Lindholm B, Stenvinkel P, Jacob-Filho W, Noronha IL, Zatz R, Moyses RMA, Elias RM (2020) Design and methodology of the Aging Nephropathy Study (AGNES): a prospective cohort study of elderly patients with chronic kidney disease. BMC Nephrol 21(1):461. https://doi.org/10.1186/s12882-020-02116-w
Acknowledgements
We thank Fatima Libanio for extracting the data from electronic charts.
Funding
There is no funding
Author information
Authors and Affiliations
Contributions
RME conceived the idea; PMRP and LCA collected the data; RZ, RMAM, and RME supervised the research; PMRP, RZ, RMAM and RME discussed and interpreted the results; RME analyzed the data; PMRP, RZ, and RME drafted the manuscript; All authors read and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interest.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pina, P.M.R., Arcon, L.C., Zatz, R. et al. Older patients are less prone to fast decline of renal function: a propensity-matched study. Int Urol Nephrol 55, 3245–3252 (2023). https://doi.org/10.1007/s11255-023-03610-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03610-4