Abstract
Purpose
The increasing frequency of coexistence of focal segmental glomerulosclerosis (FSGS) and obesity-associated glomerulopathy and the relationship between metabolic syndrome components and chronic kidney disease have been demonstrated in studies. Based on this information, in this study, we aimed to compare FSGS and other primary glomerulonephritis diagnoses in terms of parameters of metabolic syndrome and hepatic steatosis.
Materials and methods
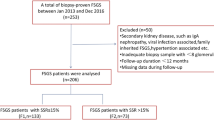
In our study, the data of 44 patients who were diagnosed FSGS through kidney biopsy and 38 patients with any other primary glomerulonephritis diagnoses in our nephrology clinic were retrospectively analyzed. Patients were divided into two groups: FSGS and other primary glomerulonephritis diagnoses, and they were examined in terms of their demographic data, laboratory parameters, body composition measurements, and the presence of hepatic steatosis, as shown using liver ultrasonography.
Results
In the comparative analysis of patients with FSGS and other primary glomerulonephritis diagnoses, with the increase in age increased the risk of FSGS by 1.12 times, the increase in BMI increased the risk of FSGS by 1.67 times, while with the decrease in waist circumference decreased the risk of FSGS by 0.88 times, the decrease in HbA1c decreased the risk of FSGS by 0.12 times, and the presence of hepatic steatosis increased the risk of FSGS by 20.24 times.
Conclusion
The presence of hepatic steatosis, an increase in waist circumference and BMI values, which are body components favoring obesity, and an increase in HbA1c, which is a marker for hyperglycemia and insulin resistance, are greater risk factors for the development of FSGS compared with other primary glomerulonephritis diagnoses.


Similar content being viewed by others
Data Availability
For the availability of the data, the study was carried out with the permission of the relevant authorities and the ethics committee.
References
Rivera F, López-Gómez JM, Pérez-García R, Spanish Registry of Glomerulonephritis (2004) Clinicopathologic correlations of renal pathology in Spain. Kidney Int 66(3):898–904. https://doi.org/10.1111/j.1523-1755.2004.00833.x
Nagata M (2016) Podocyte injury and its consequences. Kidney Int 89(6):1221–1230. https://doi.org/10.1016/j.kint.2016.01.012
Haas M, Meehan SM, Karrison TG, Spargo BH (1997) Changing etiologies of unexplained adult nephrotic syndrome: a comparison of renal biopsy findings from 1976–1979 and 1995–1997. Am J Kidney Dis 30(5):621–631. https://doi.org/10.1016/s0272-6386(97)90485-6
Rosenberg AZ, Kopp JB (2017) Focal segmental glomerulosclerosis. Clin J Am Soc Nephrol 12(3):502–517. https://doi.org/10.2215/CJN.05960616
Kambham N, Markowitz GS, Valeri AM, Lin J, D’Agati VD (2001) Obesity-related glomerulopathy: an emerging epidemic. Kidney Int 59(4):1498–1509. https://doi.org/10.1046/j.1523-1755.2001.0590041498.x
D’Agati VD, Chagnac A, de Vries AP, Levi M, Porrini E, Herman-Edelstein M, Praga M (2016) Obesity-related glomerulopathy: clinical and pathologic characteristics and pathogenesis. Nat Rev Nephrol 12(8):453–471. https://doi.org/10.1038/nrneph.2016.75
-TEMD (2019), Obezite Tanı ve Tedavi Kılavuzu 2019
Loomba R, Sanyal AJ (2013) The global NAFLD epidemic. Nat Rev Gastroenterol Hepatol 10(11):686–690. https://doi.org/10.1038/nrgastro.2013.171
Grundy SM (1998) Hypertriglyceridemia, atherogenic dyslipidemia, and the metabolic syndrome. Am J Cardiol 81(4A):18B-25B. https://doi.org/10.1016/s0002-9149(98)00033-2
Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, Charlton M, Sanyal AJ (2012) The diagnosis and management of non-alcoholic fatty liver disease: practice Guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Hepatology 55(6):2005–2023. https://doi.org/10.1002/hep.25762
Gennuso KP, Gangnon RE, Thraen-Borowski KM, Colbert LH (2015) Dose-response relationships between sedentary behaviour and the metabolic syndrome and its components. Diabetologia 58(3):485–492. https://doi.org/10.1007/s00125-014-3453-z
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC, Jr, International Diabetes Federation Task Force on Epidemiology and Prevention, Hational Heart, Lung, and Blood Institute, American Heart Association, World Heart Federation, International Atherosclerosis Society (2009) Harmonizing the metabolic syndrome: a joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood institute; American heart association; world heart federation; international atherosclerosis society; and international association for the study of obesity. Circulation 120(16):1640–1645. https://doi.org/10.1161/CIRCULATIONAHA.109.192644
Ferraioli G, Soares Monteiro LB (2019) Ultrasound-based techniques for the diagnosis of liver steatosis. World J Gastroenterol 25(40):6053–6062. https://doi.org/10.3748/wjg.v25.i40.6053
Paul J (2020) Recent advances in non-invasive diagnosis and medical management of non-alcoholic fatty liver disease in adult. Egypt Liver J 10:37. https://doi.org/10.1186/s43066-020-00043-x
El Azeem HA, Khalek el SA, El-Akabawy H, Naeim H, Khalik HA, Alfifi AA (2013) Association between nonalcoholic fatty liver disease and the incidence of cardiovascular and renal events. J Saudi Heart Assoc 25(4):239–246. https://doi.org/10.1016/j.jsha.2013.07.004
Targher G (2007) Non-alcoholic fatty liver disease, the metabolic syndrome and the risk of cardiovascular disease: the plot thickens. Diabetic Med 24(1):1–6. https://doi.org/10.1111/j.1464-5491.2007.02025.x
Hamaguchi M, Kojima T, Takeda N, Nagata C, Takeda J, Sarui H, Kawahito Y, Yoshida N, Suetsugu A, Kato T, Okuda J, Ida K, Yoshikawa T (2007) Nonalcoholic fatty liver disease is a novel predictor of cardiovascular disease. World J Gastroenterol 13(10):1579–1584. https://doi.org/10.3748/wjg.v13.i10.1579
Targher G, Chonchol M, Bertolini L, Rodella S, Zenari L, Lippi G, Franchini M, Zoppini G, Muggeo M (2008) Increased risk of CKD among type 2 diabetics with nonalcoholic fatty liver disease. J Am Soc Nephrol 19(8):1564–1570. https://doi.org/10.1681/ASN.2007101155
Yodoshi T, Arce-Clachar AC, Sun Q, Fei L, Bramlage K, Xanthakos SA, Flores F, Mouzaki M (2020) Glomerular hyperfiltration is associated with liver disease severity in children with nonalcoholic fatty liver disease. J Pediatr 222:127–133. https://doi.org/10.1016/j.jpeds.2020.03.038
Chagnac A, Weinstein T, Herman M, Hirsh J, Gafter U, Ori Y (2003) The effects of weight loss on renal function in patients with severe obesity. J Am Soc Nephrol 14(6):1480–1486. https://doi.org/10.1097/01.asn.0000068462.38661.89
Kasiske BL, Crosson JT (1986) Renal disease in patients with massive obesity. Arch Intern Med 146(6):1105–1109
Fletcher EC (1993) Obstructive sleep apnea and the kidney. J Am Soc Nephrol 4(5):1111–1121. https://doi.org/10.1681/ASN.V451111
Satman I, Omer B, Tutuncu Y, Kalaca S, Gedik S, Dinccag N, Karsidag K, Genc S, Telci A, Canbaz B, Turker F, Yilmaz T, Cakir B, Tuomilehto J, TURDEP-II Study Group (2013) Twelve-year trends in the prevalence and risk factors of diabetes and prediabetes in Turkish adults. European J Epidemiol 28(2):169–180. https://doi.org/10.1007/s10654-013-9771-5
Kurella M, Lo JC, Chertow GM (2005) Metabolic syndrome and the risk for chronic kidney disease among nondiabetic adults. J Am Soc Nephrol 16(7):2134–2140. https://doi.org/10.1681/ASN.2005010106
Kaartinen K, Syrjänen J, Pörsti I, Harmoinen A, Huhtala H, Mustonen J (2014) Metabolic syndrome in IgA glomerulonephritis. Nephron extra 4(2):138–145. https://doi.org/10.1159/000365591
Kaartinen K, Syrjänen J, Pörsti I, Harmoinen A, Pasternack A, Huhtala H, Niemelä O, Mustonen J (2007) Insulin resistance and the progression of IgA glomerulonephritis. Nephrol Dial Transplant 22(3):778–783. https://doi.org/10.1093/ndt/gfl704
Yang Y, Wei RB, Wang YD, Zhang XG, Rong N, Tang L, Chen XM (2012) Higher HOMA-IR index and correlated factors of insulin resistance in patients with IgA nephropathy. Clin Nephrol 78(5):353–358. https://doi.org/10.5414/CN107613
Schrauben SJ, Jepson C, Hsu JY, Wilson FP, Zhang X, Lash JP, Robinson BM, Townsend RR, Chen J, Fogelfeld L, Kao P, Landis JR, Rader DJ, Hamm LL, Anderson AH, Feldman HI (2019) Insulin resistance and chronic kidney disease progression, cardiovascular events, and death: findings from the chronic renal insufficiency cohort study. BMC Nephrol 20(1):60. https://doi.org/10.1186/s12882-019-1220-6
Fliser D, Pacini G, Engelleiter R, Kautzky-Willer A, Prager R, Franek E, Ritz E (1998) Insulin resistance and hyperinsulinemia are already present in patients with incipient renal disease. Kidney Int 53(5):1343–1347. https://doi.org/10.1046/j.1523-1755.1998.00898
O’Shaughnessy MM, Hogan SL, Thompson BD, Coppo R, Fogo AB, Jennette JC (2018) Glomerular disease frequencies by race, sex and region: results from the International Kidney Biopsy Survey. Nephrol Dial Transplant 33(4):661–669. https://doi.org/10.1093/ndt/gfx189
Saran R, Li Y, Robinson B, Abbott KC, Agodoa LY, Ayanian J, Bragg-Gresham J, Balkrishnan R, Chen JL, Cope E, Eggers PW, Gillen D, Gipson D, Hailpern SM, Hall YN, He K, Herman W, Heung M, Hirth RA, Hutton D, Jacobsen SJ, Kalantar-Zadeh K, Kovesdy CP, Lu Y, Molnar MZ, Morgenstern H, Nallamothu B, Nguyen DV, O’Hare AM, Plattner B, Pisoni R, Port FK, Rao P, Rhee CM, Sakhuja A, Schaubel DE, Selewski DT, Shahinian V, Sim JJ, Song P, Streja E, Kurella Tamura M, Tentori F, White S, Woodside K, Hirth RA (2016) US renal data system 2015 annual data report: epidemiology of kidney disease in the United States. Am J Kidney Dis 67(3 Suppl 1):S1-305. https://doi.org/10.1053/j.ajkd.2015.12.014
Braun N, Schweisfurth A, Lohöfener C, Lange C, Gründemann C, Kundt G, Gröne HJ (2011) Epidemiology of glomerulonephritis in Northern Germany. Int Urol Nephrol 43(4):1117–1126. https://doi.org/10.1007/s11255-011-9955-4
Ozturk S, Sumnu A, Seyahi N, Gullulu M, Sipahioglu M, Artan S, Bicik Z, Kutlay S, Keles M, Oygar D, Odabas AR, Kayatas M, Dursun B, Sayarlioglu H, Trablus S, Taymez DG, Ozdemir AA, Sahin GM, Altun B, Azak A, Altintepe L, Suleymanlar G, Koc M, Selcuk Y, Kazancioglu R, Erkoc R, Gursu M, Kucuk M, Akcaoglu SA, Yıldız A, Unal A, Akarsu O, Ates K, Cankaya E, Turkmen A (2014) Demographic and clinical characteristics of primary glomerular diseases in Turkey. Int Urol Nephrol 46(12):2347–2355. https://doi.org/10.1007/s11255-014-0838-3
Turkmen A, Sumnu A, Cebeci E, Yazici H, Eren N, Seyahi N, Dilek K, Dede F, Derici U, Unsal A, Sahin G, Sipahioglu M, Gok M, Tatar E, Dursun B, Sipahi S, Yilmaz M, Suleymanlar G, Ulu S, Gungor O, Kutlay S, Bahcebasi ZB, Sahin I, Kurultak I, Turkmen K, Yilmaz Z, Kazancioglu RT, Cavdar C, Candan F, Aydin Z, Oygar DD, Gul CB, Arici M, Paydas S, Taymez DG, Kucuk M, Trablus S, Turgutalp K, Koc L, Sezer S, Duranay M, Bardak S, Altintepe L, Arikan IH, Azak A, Odabas AR, Sahin GM, Ozturk S (2020) Epidemiological features of primary glomerular disease in Turkey: a multicenter study by the Turkish Society of Nephrology Glomerular Diseases Working Group. BMC Nephrol 21(1):481. https://doi.org/10.1186/s12882-020-02134-8
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ozkan, E., Gok, M., Cetinkaya, H. et al. Comparison of focal segmental glomerulosclerosis and other primary glomerulonephrites in terms of parameters of hepatic steatosis and metabolic syndrome. Int Urol Nephrol 55, 2557–2566 (2023). https://doi.org/10.1007/s11255-023-03536-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03536-x