Abstract
Purpose
In this study, we aimed to elucidate the pathophysiology of post-micturition dribble (PMD) through analyzing several variables including pressure flow study (PFS) findings and symptoms questionnaire.
Methods
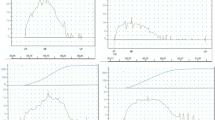
We retrospectively analyzed male patients who visited our department between 2010 and 2020. We used modified international prostate symptom score (m-IPSS), which consists of eight sub-score related to lower urinary tract symptoms (Incomplete Emptying, Frequency, Intermittency, Urgency, Weak Stream, Straining, Nocturia, and PMD) and one question related to quality of life (QOL). Multivariate regression analysis was conducted to evaluate the relationship between PMD and the variables, including age, prostate volume (PV), body mass index, bladder outlet obstruction index (BOOI), bladder contractility index, and bladder voiding efficiency, which were obtained by PFS.
Results
A total of 143 male patients were analyzed. The patients with PMD showed significantly larger PV and higher BOOI, and worse IPSS total and QOL score than those without PMD. Multivariate regression analysis showed that large PV and BOOI were significantly associated with PMD. In Spearman’s correlation analysis, PMD and each m-IPSS sub-score except nocturia had significant positive correlation. Furthermore, Spearman’s correlation analysis showed that PMD and QOL had significant strong positive correlation.
Conclusion
PMD was significantly associated with large PV and BOO evaluated by PFS. Furthermore, PMD significantly exacerbated QOL. The severity of PMD and the other m-IPSS sub-score except nocturia could have intercorrelation with each other.


Similar content being viewed by others
References
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, van Kerrebroeck P, Victor A, Wein A (2002) Standardisation sub-committee of the international continence society. The standardisation of terminology of lower urinary tract function: report from the standardisation sub-committee of the international continence society. Neurourol Urodyn 21(2):167–178. https://doi.org/10.1002/nau.10052
Abranches-Monteiro L, Hamid R, D’Ancona C, Alhasso A, Dmochowski R, Ecclestone H et al (2020) The international continence society (ICS) report on the terminology for male lower urinary tract surgery. Neurourol Urodyn 39(8):2072–2088. https://doi.org/10.1002/nau.24509
Kobayashi K, Fukuta F, Masumori N (2019) Prevalence of post-micturition dribble in Japanese men and its relationship with benign prostatic hyperplasia/lower urinary tract symptoms. Low Urin Tract Symptoms 11(2):O38–O41. https://doi.org/10.1111/luts.12210
Lerner LB, McVary KT, Barry MJ, Bixler BR, Dahm P, Das AK et al (2021) Management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA GUIDELINE PART I-initial work-up and medical management. J Urol 206(4):806–817. https://doi.org/10.1097/JU.0000000000002183
Yang DY, Jeong HC, Ko K, Lee SH, Lee SK, Shin TY et al (2019) Effect of tadalafil 5 mg on post-micturition dribble in men with lower urinary tract symptoms: a multicentre, double-blind, randomized, placebo-controlled trial. BJU Int 124(5):862–869. https://doi.org/10.1111/bju.14849
Matsukawa Y, Majima T, Matsuo K, Funahashi Y, Kato M, Yamamoto T et al (2018) Effects of tadalafil on storage and voiding function in patients with male lower urinary tract symptoms suggestive of benign prostatic hyperplasia: a urodynamic-based study. Int J Urol 25(3):246–250. https://doi.org/10.1111/iju.13489
Matsuo T, Miyata Y, Araki K, Mukae Y, Otsubo A, Ohba K et al (2020) Efficacy of tadalafil therapy and changes in oxidative stress levels in male patients with lower urinary tract symptoms and overactive bladder. Low Urin Tract Symptoms 12(1):47–53. https://doi.org/10.1111/luts.12283
Hanai T, Matsumoto S, Shimizu N, Uemura H, Sugiyama T (2008) Investigation of lower urinary tract symptoms in urological outpatients using original IPSS plus post micturition dribble questionnaire. Nihon Hinyokika Gakkai Zasshi 99(7):723–728. https://doi.org/10.5980/jpnjurol1989.99.723 ((in Japanese))
Schäfer W, Abrams P, Liao L, Mattiasson A, Pesce F, Spangberg A, Sterling AM, Zinner NR, van Kerrebroeck P (2002) International continence society. Good urodynamic practices: uroflowmetry, filling cystometry, and pressure-flow studies. Neurourol Urodyn 21(3):261–274. https://doi.org/10.1002/nau.10066
Kanda Y (2013) Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transpl 48(3):452–458. https://doi.org/10.1038/bmt.2012.244
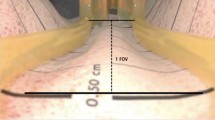
Ishii T, Kambara Y, Yamanishi T, Naya Y, Igarashi T (2014) Urine flow dynamics through prostatic urethra with tubular organ modeling using endoscopic imagery. IEEE J Transl Eng Health Med 2:1800709. https://doi.org/10.1109/JTEHM.2014.2316148
Minagawa T, Daimon H, Ogawa N, Saito T, Suzuki T, Domen T et al (2019) Morphological and clinical evaluation of prostatic urethra using modified sonourethrography with retrograde jelly injection. Low Urin Tract Symptoms 11(2):O4–O10. https://doi.org/10.1111/luts.12203
Paterson J, Pinnock CB, Marshall VR (1997) Pelvic floor exercises as a treatment for post-micturition dribble. Br J Urol 79(6):892–897. https://doi.org/10.1046/j.1464-410x.1997.00180.x
Dorey G, Speakman M, Feneley R, Swinkels A, Dunn C, Ewings P (2004) Pelvic floor exercises for treating post-micturition dribble in men with erectile dysfunction: a randomized controlled trial. Urol Nurs 24(6):490–497, 512
Yokoyama O, Yusup A, Oyama N, Aoki Y, Miwa Y, Akino H (2007) Improvement in bladder storage function by tamsulosin depends on suppression of C-fiber urethral afferent activity in rats. J Urol 177(2):771–775. https://doi.org/10.1016/j.juro.2006.09.076
Yokoyama O, Miwa Y, Oyama N, Aoki Y, Ito H, Tanase K et al (2011) Urethral sensations are related to the development of detrusor overactivity. Low Urin Tract Symptoms 3(2):59–63. https://doi.org/10.1111/j.1757-5672.2011.00096.x
Matsukawa Y, Funahashi Y, Takai S, Majima T, Ogawa T, Narita H, Kato M, Gotoh M (2017) Comparison of silodosin and naftopidil for efficacy in the treatment of benign prostatic enlargement complicated by overactive bladder: a randomized, prospective study (SNIPER study). J Urol 197(2):452–458. https://doi.org/10.1016/j.juro.2016.08.111
Matsukawa Y, Takai S, Majima T, Funahashi Y, Kato M, Yamamoto T et al (2018) Two-year follow up of silodosin on lower urinary tract functions and symptoms in patients with benign prostatic hyperplasia based on prostate size: a prospective investigation using urodynamics. Ther Adv Urol 10(9):263–272. https://doi.org/10.1177/1756287218783646
D’Ancona C, Haylen B, Oelke M, Abranches-Monteiro L, Arnold E, Goldman H, Hamid R, Homma Y, Marcelissen T, Rademakers K, Schizas A, Singla A, Soto I, Tse V, de Wachter S, Herschorn S (2019) Standardisation steering committee ICS and the ICS working group on terminology for male lower urinary tract & pelvic floor symptoms and dysfunction. The international continence society (ICS) report on the terminology for adult male lower urinary tract and pelvic floor symptoms and dysfunction. Neurourol Urodyn 38(2):433–477. https://doi.org/10.1002/nau.23897
Funding
This study has not been funded by any groups.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no financial or non-financial conflict of interest related to this study.
Ethical approval
This study protocol was approved by the Institutional Review Board (IRB) of the Faculty of Medicine in Kindai University (approval number: R02-106). In this retrospective study, IRB admitted that informed consent was waived, and opt-out method was applied to obtain consent on this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hashimoto, M., Shimizu, N., Fujimoto, S. et al. The pressure flow study investigation of pathophysiology of post-micturition dribble in male patients. Int Urol Nephrol 55, 69–74 (2023). https://doi.org/10.1007/s11255-022-03367-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-022-03367-2