Abstract
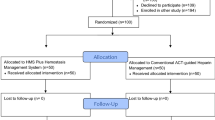
A recent heparin shortage related to an outbreak of African Swine Flu in China led to substantial increase in the use of direct thrombin inhibitors (DTI) as an alternative. We evaluated the safety and efficacy of DTIs by assessing the anticoagulation assays within the initial 48 h of therapy comparing before and during shortage. A retrospective evaluation of bivalirudin and argatroban was conducted at a single center before (May 24, 2018 through August 25, 2019) and during heparin shortage (August 26, 2019 through February 20, 2020). The primary outcome was time to first therapeutic activated partial thromboplastin time (aPTT). Secondary outcomes included the percentage of time in therapeutic aPTT range, in-hospital mortality, incidence of recurrent thrombosis, and hemorrhagic events. Of the 204 patients included in the study, 95 patients [bivalirudin (n = 35), argatroban (n = 60)] were included in the pre-shortage cohort and 109 patients [bivalirudin (n = 68), argatroban (n = 41)] were during shortage. No significant difference was observed in the time to first therapeutic aPTT pre- and during shortage (8.9 h ± 10.8 vs 8.8 h ± 10.2, P = 0.62). Compared to pre-shortage cohort, a greater percentage of time was spent in therapeutic aPTT range within the initial 48 h (32% (0–50) vs. 41.6% (0–63), P = 0.04) during shortage without statistically significant differences in the rates of in-hospital mortality, thrombosis, or bleeding. While the optimal DTI protocol is still be determined, the protocols presented in this study allowed for wide-spread utilization of DTIs during a critical heparin shortage without compromising patient safety and effectiveness, likely reflective of the enhancement of DTI protocols, clinician education, and multidisciplinary collaboration and guidance from pharmacy and hematology.

Similar content being viewed by others
References
Garcia DA, Baglin TP, Weitz JI et al (2012) Parenteral anticoagulants: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141(2 Suppl):e24S-e43S
Linkins LA, Dans AL, Moores LK et al (2012) Treatment and prevention of heparin-induced thrombocytopenia: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141(2 Suppl):e495S-e530S
Kahn SR, Lim W, Dunn AS et al (2012) Prevention of VTE in non-surgical patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141(2 suppl):e195S-e226S
Schünemann HJ, Cushman M, Burnett AE et al (2018) American Society of Hematology 2018 guidelines for management of venous thromboembolism: prophylaxis for hospitalized and nonhospitalized medical patients. Blood Adv 2:3198–3225
Doherty JU, Gluckerman TJ, Hucker WJ et al (2017) 2017 ACC expert consensus decision pathway for periprocedural management of anticoagulation in patients with nonvalvular atrial fibrillation: A report of the American College of Cardiology Clinical Expert Consensus Document Task Force. J Am Coll Cardiol 69:871–898
Koster A, Faraoni D, Levy JH (2018) Argatroban and bivalirudin for perioperative anticoagulation in cardiac surgery. Anesthesiology 128(2):390–400
Salter BS, Weiner MM, Trinh MA et al (2016) Heparin-induced thrombocytopenia: A comprehensive clinical review. J Am Coll Cardiol 67:2519–2532
Vilanova E, Tovar AMF, Mouráo Pas. Imminent risk of a global shortage of heparin caused by the African Swine Fever afflicting the Chinese pig herd. J Thromb Haemost. 2019; 17(2):254-256.
FDA drug shortages. U.S. Food and Drug Administration Website. Available at https://www.fda.gov/drugs/drug-safety-and-availability/drug-shortages. Assessed 15 April 2020.
Rosovsky RP, Barra ME, Roberts RJ et al (2020) When pigs fly: A multidisciplinary approach to navigating a critical heparin shortage. Oncologist 10(25):1–14
Fox ER, McLaughlin MM (2018) ASHP guidelines on managing drug product shortages. Am J Health Syst Pharm 75:1742–1750
Prucnal CK, Jansson PS, Deadmon E et al (2019) Analysis of partial thromboplastin times in patients with pulmonary embolism during the first 48 hours of anticoagulation with unfractionated heparin. Acad Emerg Med 26(6):657–659
Abel EE, Kane-Gill SL, Seybert AL et al (2012) Direct thrombin inhibitors for management of heparin-induced thrombocytopenia in patients receiving renal replacement therapy: comparison of clinical outcomes. Am J Health-Syst Pharm 69:1559–1567
Chanas T, Palkimas S, Maitland HS et al (2019) Evaluation of the use of argatroban or bivalirudin for the management of suspected heparin-induced thrombocytopenia in the setting of continuous renal replacement therapy. Trauma and Intensive Med 10:1–7
Kiser TH, Mann AM, Trujillo TC et al (2011) Evaluation of empiric versus nomogram based direct thrombin inhibitor management in patients with suspected heparin-induced thrombocytopenia. Am J Hematol 86:267–272
Runyan CL, Cabral KP, Riker RR et al (2011) Correlation of bivalirudin dose with creatinine clearance during treatment of heparin-induced thrombocytopenia. Pharmacotherapy 31(9):850–856
Tsu LV, Dager WE (2011) Bivalirudin dosing adjustments for reduced renal function with or without hemodialysis in the management of heparin-induced thrombocytopenia. Ann Pharmacother 45(10):1185–1192
Reichert MG, MacGregor DA, Kincaid EH et al (2003) Excessive argatroban anticoagulation for heparin-induced thrombocytopenia. Ann Pharmacother 37(5):652–654
Rice L, Hursting MJ, Baillie GM et al (2007) Argatroban anticoagulation in obese versus nonobese patients: implications for treating heparin-induced thrombocytopenia. J Clin Pharmacol 47(8):1028–1034
Beiderlinden M, Treschan TA, Görlinger K et al (2007) Argatroban anticoagulation in critically ill patients. Ann Pharmacother 41(5):749–754
Kaatz S, Ahmad D, Spyropoulos AC et al (2015) Definition of clinically relevant non-major bleeding in studies of anticoagulants in atrial fibrillation and venous thromboembolic disease in non-surgical patients: communication from the SSC of the ISTH. J Thromb Haemost 13(11):2119–2126
Benjamini Y, Hochberg Y (1995) Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stastist Soc 57(1):289–300
Keyl C, Zimmer E, Bek MJ et al (2016) Argatroban pharmacokinetics and pharmacodynamics in critically ill cardiac surgical patients with suspected heparin-induced thrombocytopenia. Thromb Haemost 115(6):1081–1089
Dingman JS, Smith ZR, Coba VE et al (2020) Argatroban dosing requirements in extracorporeal life support and other critically ill populations. Thromb Res 27(189):69–76
Vallabhajosyula S, Arora S, Lahewala S et al (2018) Temporary mechanical circulatory support for refractory cardiogenic shock before left ventricular assist device surgery. J Am Heart Assoc 7(22):e010193. https://doi.org/10.1161/JAHA.118.010193
Takayama H, Koeckert M, Soni L et al (2012) Outcomes of mechanical circulatory support for refractory cardiogenic shock in the era of more advanced ventricular assist devices. J Am Coll Cardiol 59(13 supplement):E875
Rivner H, Parmar R, Cardoso R (2017) A meta-analysis of bivalirudin versus argatroban for the treatment of heparin-induced thrombocytopenia. JACC 69(11 Supplement):2064
Gargiulo G, Carrara G, Frigoli E et al (2018) Bivalirudin or heparin in patients undergoing invasive management of acute coronary syndromes. J Am Coll Cardiol 71:1231–1242
Valgimigli M, Frigoli E, Leonardi S, et al., on behalf of the MATRIX Investigators. Bivalirudin or unfractionated heparin in acute coronary syndromes. N Engl J Med 2015;373:997–1009.
Anantha-Narayanan M, Anugula D, Gujjula N et al (2018) Bivalirudin versus heparin in percutaneous coronary intervention—a systematic review and meta-analysis of randomized trials stratified by adjunctive glycoprotein IIb/IIIa strategy. J Thorac Disc 10(6):3341–3360
Lewis BE, Wallis DE, Berkowitz SD et al (2001) Argatroban anticoagulant therapy in patients with heparin-induced thrombocytopenia. Circulation 103(14):1838–1843
Lewis BE, Wallis DE, Leya F et al (2003) Argatroban anticoagulation in patients with heparin-induced thrombocytopenia. Arch Intern Med 163(15):1849–1856
Smythe MA, Koerber JM, Forsyth LL et al (2009) Argatroban dosage requirements and outcomes in intensive care versus non-intensive care patients. Pharmacotherapy. 29(9):1073–1081
Kiser TH, Jung R, MacLaren R et al (2005) Evaluation of diagnostic tests and argatroban or lepirudin therapy in patients with suspected heparin-induced thrombocytopenia. Pharmacotherapy 25(12):1736–1745
Angiomax (bivalirudin) [package insert]. Parsippany, NJ: The Medicines Company; March 2016.
Argatroban [package insert]. Princeton, NJ: Sandoz Inc.; January 2011.
Author information
Authors and Affiliations
Contributions
CSJ and RPR contributed to data collection and critical writing or revising the intellectual content. CSJ, RJR, MEB, HL and RPR contributed significantly to concept and design, analysis, and interpretation of data. All authors reviewed and approved this manuscript.
Corresponding author
Ethics declarations
Conflict of interest
CSJ, RJR, MEB, and HL have no conflicts of interest to declare. RPR received institutional grant from Bristol‐Myers Squibb (BMS) and honoraria for advisory boards from Janssen Pharmaceuticals, Bristol‐Myers Squibb, Dova Pharmaceutical, and Portola, all outside the scope of submitted work.
Disclaimer
These dosing protocols were created by clinical experts for use in inpatients at Massachusetts General Hospital. These algorithms should not replace clinical judgment incorporating patient‐specific factors or institutional, national, or international guidelines or practice
Ethical approval
Rachel P. Rosovsky: institutional grant from Bristol‐Myers Squibb (BMS) and honoraria for advisory boards from Janssen Pharmaceuticals, Bristol‐Myers Squibb, Dova Pharmaceutical, and Portola, all of which are outside the scope of submitted work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ji, C.S., Roberts, R.J., Barra, M.E. et al. Evaluation of direct thrombin inhibitors during a critical heparin shortage. J Thromb Thrombolysis 52, 662–673 (2021). https://doi.org/10.1007/s11239-020-02357-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-020-02357-4