Abstract
Adipose tissue, including white adipose tissue (WAT), brown adipose tissue (BAT), and beige adipose tissue, is vital in modulating whole-body energy metabolism. While WAT primarily stores energy, BAT dissipates energy as heat for thermoregulation. Beige adipose tissue is a hybrid form of adipose tissue that shares characteristics with WAT and BAT. Dysregulation of adipose tissue metabolism is linked to various disorders, including obesity, type 2 diabetes, cardiovascular diseases, cancer, and infertility. Both brown and beige adipocytes secrete multiple molecules, such as batokines, packaged in extracellular vesicles or as soluble signaling molecules that play autocrine, paracrine, and endocrine roles. A greater understanding of the adipocyte secretome is essential for identifying novel molecular targets in treating metabolic disorders. Additionally, microRNAs show crucial roles in regulating adipose tissue differentiation and function, highlighting their potential as biomarkers for metabolic disorders. The browning of WAT has emerged as a promising therapeutic approach in treating obesity and associated metabolic disorders. Many browning agents have been identified, and nanotechnology-based drug delivery systems have been developed to enhance their efficacy. This review scrutinizes the characteristics of and differences between white, brown, and beige adipose tissues, the molecular mechanisms involved in the development of the adipocytes, the significant roles of batokines, and regulatory microRNAs active in different adipose tissues. Finally, the potential of WAT browning in treating obesity and atherosclerosis, the relationship of BAT with cancer and fertility disorders, and the crosstalk between adipose tissue with circadian system and circadian disorders are also investigated.
Similar content being viewed by others
1 Introduction
Recent extensive research has revealed that adipose tissue (AT) is not merely an inert fat storage tissue but also a complex organ that plays a fundamental role in controlling food intake, whole-body energy homeostasis, insulin sensitivity, blood pressure, angiogenesis, inflammation, and immunity by secreting various hormones and adipokines from different adipocytes [1,2,3,4]. AT is considered one of the largest complex endocrine organs in the body, with numerous potential therapeutic applications against obesity and related metabolic diseases [5]. It contains a complex mixture of cells, with one-third being mature adipocytes and two-thirds consisting of numerous cell types collectively known as the stromal vascular fraction. The latter fraction comprises a heterogeneous population of precursor cells and provides a rich source of mesenchymal stem cells (MSCs), which can be easily isolated from human AT. However, other cell types can be found in the fraction, such as pre-adipocytes, fibroblasts, endothelial progenitor cells (EPCs), pericytes, monocytes/macrophages, vascular smooth muscle cells, leukocytes, T-cells, and erythrocytes [6]. These cells form an effective communication network that regulates the activity and function of AT reservoirs.
Our previous studies have highlighted the importance of understanding the heterogeneity of AT and its impact on health [7,8,9]. Based on their color, ATs in mammals have been classified into three types: white AT (WAT), brown AT (BAT), and beige (brite, brown-in-white, brown-like) AT (beige AT). WAT is primarily involved in energy storage; whereas BAT is predominantly responsible for non-shivering thermogenesis, beige AT expends energy to generate heat during cold exposure (cold-induced thermogenesis). This review focuses on the differential properties of white, brown, and beige ATs, the molecular mechanisms underlying the development of adipocytes, and the significant roles of batokines and regulatory miRNAs in different ATs. In addition, it scrutinizes WAT browning by various agents as a therapeutic target against obesity and related metabolic disorders such as atherosclerosis, cancer, and fertility. Finally, the relationship of BAT with cancer and infertility and the crosstalk between AT, circadian system, and circadian disorders will be studied.
2 White, brown, and beige adipose tissue
The expansion of WAT begins shortly after birth [10]. WAT is found throughout the body and is classified into two groups: visceral WAT (vWAT) depot and subcutaneous WAT (sWAT) depot [11]. Lineage tracing experiments have shown that white adipocytes arise from embryonic mesothelial cells, and the segregation of visceral and subcutaneous adipocytes occurs during late embryogenesis [12]. Morphologically, WAT is typically characterized by large unilocular/large lipid droplets, limited mitochondria, and ivory or yellowish color. WAT is mainly composed of unilocular adipocytes named white adipocytes [13]. Following overeating or low energy intake, WAT can capture free fatty acids (FFAs) and glucose from blood plasma and convert them into triglycerides (TGs). Adipose TG lipase (ATGL) catalyzes the first stage of lipolysis of cytoplasmic triacylglycerols in WAT [14, 15]. Therefore, WAT supplies energy during fasting and regulates energy homeostasis. WAT is highly innervated with afferent and efferent sympathetic nerves; but has no parasympathetic innervation [16]. In the case of obesity, hyperplasia, hypertrophy, secretion of vasoconstrictors, and immune cell infiltration are observed in WAT [17]. BAT is formed and differentiated before birth to protect newborns from cold [18, 19]. BAT is present and active in human adults, and its activity is decreased in various pathological states such as obesity, diabetes, and aging [20]. Human BAT is in the supraclavicular, axillary, neck, periaortic, paravertebral, perirenal, and mediastinal regions [5, 21]. In mice, BAT is mostly in the interscapular region [22]. In humans, BAT comprises a small portion of AT and vanishes from most parts of the body with age, remaining only around deeper organs [23]. BAT is considered to have a high degree of vascularization and sympathetic innervation [24]. Compared to WAT, BAT has significantly high mitochondrial content and macroscopically appears brown due to heme cofactors in the mitochondrial enzyme cytochrome oxidase [25]. BAT is mainly composed of brown adipocytes that contain large amounts of multilocular/small lipid droplets of various sizes. Brown adipocytes are small and polygonal, unlike white adipocytes [26].
BAT preserves body temperature by a process known as non-shivering thermogenesis, dissipating energy in the form of heat. Thermogenesis is mediated through brown adipocyte-specific uncoupling protein 1 (UCP1), also called thermogenin, in response to adrenergic signaling via the sympathetic nervous system [27]. Upon exposure to a cold stimulus, sympathetic neurons release noradrenaline (NADR) from the synapse region. NADR attaches to several β-adrenergic receptors (ARs) (classically β3-AR but also β1- and β2-AR [28, 29]) on the brown adipocyte. Activation of β-ARs triggers a signaling cascade that leads to lipolysis of TG stores and release of fatty acids (FAs) and, finally, activation of UCP1 [27] (Fig. 1). UCP1 protein is located in the inner mitochondrial membrane (IMM) and transports H+ ions across the IMM in the presence of FAs and glucose, leading to the uncoupling of cellular respiration and ATP synthesis, thereby releasing heat instead of ATP production [27, 30] (Fig. 1). Thus, BAT plays a natural anti-obesity role. However, the precise mechanism of function of UCP1 is not well understood as direct methods are unavailable [31].
BAT activation and molecular mechanism of UCP1 function studied by McNeill et al. [27] (with permission). Upon exposure to a cold stimulus, sympathetic neurons release NADR from the synapse region. NADR attaches to several β-ARs on the brown adipocyte, activating adenylyl cyclase (AC) and converting ATP to cyclic adenosine 3′,5′-monophosphate (cAMP) which, in turn, causes protein kinase A (PKA) activation. PKA induces the lipolysis of TG stores and the release of fatty acids (FAs), which are the primary substrate for the thermogenesis process; these attach to and activate the UCP1 protein in the IMM. Utilizing the electrochemical proton gradient of the electron transport train, the UCP1 protein transports H+ ions across the IMM. This leads to uncoupling cellular respiration from ATP synthesis, releasing heat instead of ATP production. FFAs are transported into the brown adipocyte via fatty acid transport protein (FATP), fatty acid binding protein (FABP), and a cluster of differentiation 36 (CD36). Glucose is also transported into the brown adipocyte via the glucose transporters (GLUT1/4). Uptake of circulating FFA and glucose helps the regeneration of intracellular TG stores. Moreover, glucose substrate enters the tricarboxylic acid cycle (TCA, also known as the Krebs or citric acid cycle) via the glycolysis process. C1–4, complex 1–4; CoQ, co-enzyme Q; Cyto C, cytochrome C; e−, electron; H+, hydrogen ion
White adipocytes express several enriched genetic markers, including LPL, G3PHD, ASC1, Tcf21, Hoxc8, Hoxc9, and TLE3 [32,33,34]. As a major endocrine organ, WAT also secretes hormones such as adiponectin, leptin, resistin, and cytokines such as tumor necrosis factor-alpha (TNF-α), IL-6, and monocyte chemotactic protein-1 (MCP-1), which play a role in regulating whole-body metabolism, insulin resistance, and low-grade systemic inflammation connected with obesity [35, 36]. In addition to UCP1, Cidea, PPARA, Pgc1a, Prdm16 [36], LHX8, Zic1 [33], Eva1, Pdk4, Ebf3, and Hspb7 [37, 38] have also been described as BAT-specific genetic markers [20, 32]. UCP1 is nearly undetectable in WAT, but the UCP2 isoform is expressed in parts of WAT [39]. The main genetic markers for BAT and WAT are listed in Table 1.
Recent studies have shown that beige adipocytes expressing key thermogenic factor UCP1 can develop in WAT in response to certain environmental, genetic, or pharmacological stimuli [40]. These adipocytes were named beige (brite, brown-in-white, brown-like) adipocytes as a group distinct from WAT and BAT [20, 37]. Beige adipocytes arise from sWAT depots in response to β-adrenergic stimulation, diet, or exposure to cold via a reversible process called browning or beiging [20]. However, after the stimulus is withdrawn, beige adipocytes change their expression profile and display white adipocyte features again [41]. Factors such as increasing age, obesity, and metabolic disorders are related to loss of BAT (whitening process) and decreased capacity to induce browning of WAT [20]. Evolutionarily, beige adipocytes are most similar to white adipocytes, as both originate from myogenic transcription factor 5 (Myf5)-negative mesodermal stem cells [37, 42] and functionally, they are most similar to brown adipocytes, as they can convert chemical energy into heat under certain stimuli [41].
Although beige and white adipocytes have the same origin, they appear to have distinct transcriptional profiles and metabolic roles [43]. In mice, beige adipocytes are interspersed within sWAT depots. In adult humans, these adipocytes are located in the cervical and supraclavicular regions [44]. Like brown adipocytes, beige adipocytes are characterized by multilocular /multiple small lipid droplets with variable size, high mitochondrial content, and the expression of thermogenic genes such as UCP1, Pgc1a, PPARA, and Cidea [20, 36, 45, 46]. In addition to thermogenic gene expression, beige adipocytes express unique surface markers PAT2 and P2RX5 [34, 47] and genetic markers Epsti1, Tmem26 [20, 32, 48], Cd137 [37], HOX9a, TBX1 [37], CITED1 [38], TNFRSF9 [49], and Shox2 [50]. The principal differences between the three types of AT are summarized in Table 1.
3 Origin of white, brown, and beige adipocytes
The mesenchymal and tissue stem cell committee of the International Society for Cellular Therapy (ISCT) has established standards to describe human MSCs used in research and clinical applications [61]. These standards include (1) the ability of MSCs to adhere to the plastic surface under standard cell culture conditions, (2) multipotency, indicating the capability to differentiate into mature adipocytes, osteoblasts, chondroblasts, and myoblast cells, and expression of cell surface molecular markers such as CD73, CD90 and CD105, while lacking expression of CD11b, CD14, CD19, CD34, CD45, c-kit, CD79a and human leukocyte antigen-DR (HLA-DR). MSCs can be isolated from various tissues, with AT being a particularly abundant and readily available source of mature stem cells that can differentiate along numerous pathways into both adipogenic and myogenic lineages (Fig. 2).
Origin of white, brown, and beige adipocytes. Several sources have been identified for the isolation of mesenchymal stem cells (MSCs), which have a multipotent capacity to differentiate into the mesodermal lineage. The differentiation of MSCs into brown, white, and beige adipocytes is regulated by their essential transcription factors. Brown adipocytes and skeletal muscles are formed from Myf5+ progenitor cells. In contrast, white adipocytes are formed from Myf5+ and Myf5− progenitor cells. The origin of beige adipocytes is still unknown, but evidence suggests that they are formed from Myf5− progenitor cells or transdifferentiation from mature white adipocytes
White adipocytes, predominantly with an adipogenic lineage, mainly arise from myogenic transcription factor 5 negative (Myf5−) progenitor cells [45]. However, the development of white adipocytes is highly complex, as they can also arise from Myf5+ progenitor cells [62]. The adipogenic lineage can be induced by several factors, including bone morphogenetic proteins (BMPs), transforming growth factor-beta (TGF-β), fibroblast growth factor 1 and 2 (FGF1 and 2), insulin-like growth factor 1 (IGF-1), activin, IL-17, and others [62]. Moreover, the expression of transcription factor TCF21, as a unique regulator in preadipocytes, induces differentiation into the white lineage and inhibits differentiation into the myogenic lineage [63, 64]. Brown adipocytes and myocytes, with a myogenic lineage, originate from myogenic transcription factor 5 positive (Myf5+) progenitor cells. Myf5+ is a main myogenic regulatory factor [45, 65]. The Myf5+ progenitor cells turn into brown preadipocytes by BMP7 [66], PR domain containing 16 (PRDM16) [67], and early B-cell transcription factor 2 (EBF2) [68]. Inducing these markers has been shown to result in increased expression of BAT-specific markers, including peroxisome proliferator-activated receptor gamma (PPARγ), PPARγ coactivator 1 alpha (PGC1α), and CCAAT/enhancer-binding proteins (C/EBPs) in collaboration with the transcriptional co-regulator PR domain containing 16 (PRDM16) [69].
In the ultimate stage of differentiation, preadipocytes are changed into mature adipocytes using specific factors [69, 70]. BMPs are essential for the development of adipocytes. BMP7 induces the expression of the thermogenic protein UCP1, leading to the development of a brown or beige lineage [71, 72]. In addition to the white lineage, BMP4 is also related to the beige lineage, and its excessive expression increases UCP1 levels [73]. β-adrenergic signaling is another essential factor for brown and beige lineage development. PPARγ, a significant regulator of adipogenesis, is involved in the maturation and activity of all three types of adipocytes [64, 74]. It also interferes with β-adrenergic-induced brown adipocyte thermogenesis [75]. PGC1α is a significant regulator of BAT metabolism, which is strongly activated after cold exposure, leading to increased activity of several transcription factors, including PPARs [76]. Additionally, PGC1α enhances fatty acid oxidation, mitochondrial biogenesis, and UCP1 activity in brown adipocytes [76, 77]. The bidirectional cell fate switch between brown adipocytes and skeletal myoblasts is controlled by the transcriptional regulator PRDM16. Key players in the repression or activation of the PRDM16 factor [78] are known to be the transcription factors MyoD and Myf5. The PRDM16-C/EBPβ complex induces PPARγ expression in myogenic precursors, activating adipogenic genes in brown adipocytes [79]. Thus, PPARγ, PGC1α, and PRDM16 are three essential factors for achieving the brown adipocyte phenotype [80]. EBF2 controls brown pre-adipose cell identity and is an elective marker of brown and beige adipogenic precursor cells [68, 81].
The source of beige adipocytes is still not clear. Evidence suggests that they may originate from Myf5− progenitor cells or through transdifferentiation from pre-existing mature white adipocytes [82, 83]. White adipocytes can differentiate into beige adipocytes under cold exposure, by β3-adrenergic agonists, PPARγ agonists, FGF21, irisin, and natriuretic peptides [74, 84].
4 Secretory factors of brown/beige adipocytes: endocrine, paracrine, and autocrine
Although research on BAT focuses primarily on its energy expenditure properties as a potential pathway to treat metabolic imbalances, new studies also target the autocrine, paracrine, and endocrine functions of brown/beige adipocytes [85]. Currently, new treatment approaches are focusing on brown/beige adipocytes; identifying the main secretory factors of these cells and characterizing their secretory roles is crucial in discovering novel therapeutic candidates against metabolic disorders such as obesity, type 2 diabetes, and cardiovascular diseases [45, 86]. However, there is still no comprehensive understanding of the brown/beige adipocyte secretomes, and further research in this field is necessary [86]. Regulatory molecules secreted by brown/beige adipocytes, known as brown adipokines or batokines [86], include diverse signaling molecules such as metabolites, lipids, peptides, or microRNAs. These batokines (1) act on the cell that secretes them (autocrine role), which may have positive or negative effects on their thermogenic activity, (2) act on adjacent cells (paracrine role), or (3) are released into the circulation to affect distant cells (endocrine role) [87, 88]. According to several studies from different laboratories, when small amounts of healthy BAT are transplanted into rodent models of obesity and insulin resistance, it improves the recipients' metabolic profiles, weight, and even fecundity [88, 89]. It is likely that factors secreted by BAT may explain their healthy systemic effects. These discoveries highlight the potential of brown adipokines in the treatment of possible metabolic disorders. The following will describe the batokines secreted by brown/beige adipocytes with autocrine, paracrine, and endocrine effects and their tissue targets. The types of these batokines and their tissue targets are shown in Fig. 3.
Comprehensive representation of the diverse range of endocrine, paracrine, and autocrine factors secreted by brown/beige adipocytes and their target tissues. A Brown/beige adipocytes secrete endocrine factors that may signal distant tissues, including the liver, brain, pancreas, heart, bone, and WAT. B Brown/beige adipocytes secrete factors with paracrine roles, which act on the bone, vascular system, nervous, and immune cells contained in BAT and beige ATs. C Brown/beige adipocytes secrete peptidic and non-peptidic molecules with autocrine function, leading to a positive (+) or negative (-) effect on BAT thermogenic activity. Factors with a positive function increase mitochondrial activity and the level of UCP1 protein, while factors with a negative function lead to the whitening of BAT, increased lipid droplet size, reduced mitochondrial number, and impaired UCP1 induction
Lipokine 12,13-dihydroxy-9Z-octadecenoic acid (12,13-diHOME)
This non-peptidic autocrine factor is secreted by brown adipocytes in response to cold-induced activation of biosynthesis enzymes [90]. 12,13-diHOME operates as a stimulator of BAT activity by increasing the uptake of TGs into brown adipocytes. As a therapeutic agent, this lipokine resolves hypertriglyceridemia in patients with metabolic syndrome and diabetes [90].
Prostaglandins and prostaglandin-related molecules
Prostaglandins released by brown/beige adipocytes lead to BAT activation and WAT browning. For example, prostaglandin E2, an autocrine factor positively affecting brown/beige adipocyte activity, induces WAT browning in mice and trans-differentiation of human white adipocytes to beige adipocytes [91]. Cyclooxygenase-2 and lipocalin prostaglandin D synthase (L-PGDS) are necessary for prostaglandin synthesis. L-PGDS is produced in BAT and has a positive relationship with BAT activity. The absence of this significant autocrine factor impairs BAT activation and WAT browning [91].
Adenosine
Adenosine is secreted by activated brown adipocytes via sympathetic responses and, as an autocrine factor, promotes the lipolysis process, which is crucial for thermogenic activation [92]. In addition to its autocrine effects, adenosine causes WAT browning [92].
Endocannabinoids
Endocannabinoids function as negative autocrine regulators that control the β3-adrenergic pathway-induced BAT thermogenic activation and WAT browning [93, 94].
Soluble form of the low-density lipoprotein receptor relative LR11 (sLR11)
sLR11, one of the negative regulators of thermogenesis, is derived from brown/beige adipocytes [95]. sLR11 attaches directly to the BMP receptor and thus disturbs its downstream signaling pathway, resulting in a reduced thermogenesis process in a cell-autonomous state [95]. This mechanism has been suggested to minimize extreme energy wastage [95].
Growth differentiation factor-8 (GDF-8/myostatin)
Following stimulation of starvation-related neural circuits, GDF-8/myostatin is secreted by brown adipocytes [96]. As an endocrine factor, GDF-8 controls the function of skeletal muscles [86, 97]. Moreover, as an essential negative autocrine factor, it regulates WAT browning and BAT thermogenic activity [98, 99]. Myostatin deficiency leads to enhanced differentiation of cells into brown adipocytes and insulin sensitivity [96].
Follistatin
This soluble glycoprotein batokine is upregulated in brown adipocytes exposed to cold. Unlike GDF-8, follistatin positively affects thermogenic activity [98, 100].
Bone morphogenetic protein (BMP)
Several BMP members regulate adipocyte differentiation and thermogenesis, influencing white/beige/brown adipogenesis through various mechanisms [43]. BMP7 is mainly generated by stromal vascular cells in AT [66, 101]. Autocrine/paracrine signaling of BMP7 induces the expression of PRDM16 and PGC1α factors in adipose progenitors and leads to the commitment of mesenchymal progenitor cells to brown and beige adipocyte lineages [66, 102]. BMP7 shows significant activity in promoting brown/beige adipocyte differentiation and thermogenesis processes in vivo and in vitro, and thus, offers a possible new therapeutic approach to treating obesity [66]. BMP4 regulates white and beige adipocyte differentiation [103].
Mature brown adipocytes release the BMP8b batokine in response to noradrenergic-mediated thermogenic stimulus, cold exposure, and nutritional factors such as HFD [104]; it can be used as a novel therapeutic target in obesity and obesity-related disorders. BMP8b promotes BAT responsiveness to β3-adrenergic receptor stimulation and activates p38 MAP kinase signaling through key intracellular effectors such as Smad1, Smad5, and Smad8 [104]. By inhibiting AMP-activated protein kinase (AMPK), BMP8b may have a possible endocrine function in the ventromedial hypothalamus of the brain [104, 105]. BMP8b targets the vascular system through its paracrine action and, with its autocrine action on beige/brown adipocytes, releases neuregulin-4 (NRG4), improving sympathetic innervation [86]. Also, BMP8b is associated with BAT thermogenesis and the regulation of thermogenesis in human newborns [106].
SLIT2-C
SLIT2-C (a cleaved form of the SLIT2 protein) is an autocrine factor positively affecting BAT activity. SLIT2-C boosts AT thermogenesis by inducing PKA signaling downstream of the β-adrenergic receptor pathway, leading to increased energy expenditure and improved glucose homeostasis [107, 108]. Recently, many studies have shown that circulating SLIT2 levels are negatively correlated with metabolic markers of diabetes mellitus [108]. Besides its autocrine action, SLIT2-C may also have an endocrine effect on the browning/beiging of WAT [107].
Peptidase M20 domain containing 1 (PM20D1)
PM20D1 is expressed in UCP1+ adipocytes and is secreted upon exposure to cold. It catalyzes the biosynthesis of N-fatty acyl amino acids (N-FAAAs) from free long-chain FAs and free amino acids [109]. PM20D1 is involved in energy homeostasis as a UCP1-independent endogenous mitochondrial uncoupler, which increases cellular respiration [109].
Chemerin
Chemerin is involved in lipid metabolism in an autocrine manner. Its expression in BAT decreases during cold exposure but increases in response to an HFD in mice [110]. Chemokine-like receptor 1 (CMKLR1) and G protein-coupled receptor-1 (GPCR-1), two well-known chemerin receptors, are expressed in brown adipocytes [111].
Endothelin-1 (ET-1)
ET-1, as an autocrine factor, is released by brown/beige adipocytes. Via induction of the Ednra/Gq signaling pathway, it has a negative effect on thermogenic activity in brown/beige adipocytes [112].
Vascular endothelial growth factor A (VEGF-A)
VEGF-A is highly expressed in brown adipocytes during cold exposure. VEGF-A promotes macrophage function and induces BAT vascularization by targeting endothelial cells [113]. VEGF-A can also target brown adipocytes as an autocrine factor, essential for BAT activity and thermogenesis [113]. Based on in vivo studies performed in obese mice models, a reduced level of VEGF-A leads to the loss of BAT thermogenic potential [114].
Nitric oxide (NO)
NO generated in brown adipocytes prevents the proliferation and induction of preadipocyte differentiation in primary cultures through NO synthase activities caused by the noradrenergic system [115]. In addition to positive autocrine action, NO plays a paracrine role by targeting vascular cells in BAT [116]. Mineral nitrate also induces NO synthesis, leading to WAT browning [117]. BAT and WAT express metabolically active endothelial (eNOS) and inducible (iNOS) nitric oxide synthases. The deletion of the gene encoding iNos improves BAT function [118, 119] and WAT inflammation [120] and metabolism [121] in mice, suggesting a more complex role of nitric oxide in AT metabolism.
Insulin-like growth factor-1 (IGF-1) and basic fibroblast growth factor-2 (FGF-2)
IGF-1 and FGF-2 secreted by brown adipocytes cause the propagation of preadipocytes in BAT [122]. IGF-1, as a mitogenic peptide, induces the differentiation of brown adipocytes and is mostly secreted by the liver [45]. Thus, IGF-1 acts in an autocrine, paracrine, and endocrine manner [123, 124]. In rodent models of type 1 diabetes, the anti-diabetic activity observed from the transplantation of small amounts of fetal BAT may be due to the secretion of IGF-1 peptide from BAT [124, 125].
Hydrogen peroxide (H2O2)
H2O2 is secreted by brown/beige adipocytes with paracrine effects, acting on vascular cells and suppressing contractility. H2O2 is produced by the NADPH oxidase-4 enzyme, which is extremely expressed in BAT [126].
Angiopoietin-like 8 (ANGPTL8)
In response to cold exposure, ANGPTL8, as a secretory regulatory factor, increases in brown adipocytes and suppresses lipoprotein lipase activity bound to the luminal surface of endothelial cells. The function of ANGPTL8 in BAT thermogenic regulation is unknown [127, 128].
Nerve growth factor (NGF) and S100b
NGF and S100b proteins released by brown adipocytes promote neurite outgrowth upon exposure to cold and enhance sympathetic nerve regeneration in brown and beige ATs [129, 130].
NRG4
NRG4 is an epidermal growth factor (EGF) family member and is more highly expressed in BAT than WAT. Therefore, it is known as an enriched factor in brown adipocytes [131, 132]. NRG4 is highly induced during brown adipocyte differentiation and enhances in response to β-adrenergic receptor activation in brown adipocytes [133]. NRG4 targets the liver by its endocrine activity, leading to increased oxidation of hepatic fatty acids and suppression of hepatic lipogenesis [131], which has positive effects on insulin sensitivity [45]. Non-alcoholic fatty liver disease (NAFLD) and type 2 diabetes mellitus (T2DM) may result from impaired NRG4 signaling. Therefore, these findings introduce NRG4 as a potential therapeutic target [68, 131]. NRG4 promotes nerve terminal branching through its paracrine action inside BATs [134]. NRG4 has also been suggested to increase the browning/beiging of WAT in response to cold exposure [45].
Interleukin-6
IL-6 is secreted by BAT in response to noradrenergic stimulation and cold exposure [86]. By paracrine action, IL-6 targets M2-type macrophages and eosinophils; these local immune cells are associated with increased BAT activity and promote WAT browning [87, 135]. Also, IL-6 targets several cell types, including pancreas, brain, liver, and heart cells [136]. IL-6 shows an endocrine action in improving metabolic health and is positively related to obesity, insulin resistance, and type 2 diabetes [137, 138]. IL-6 secretion by beige adipocytes has positive autocrine effects in WAT browning [137].
Adiponectin
Adiponectin is known as a WAT-derived adipokine. Upon cold exposure, adiponectin is induced in sWAT and promotes sWAT browning via M2-macrophage proliferation. However, it has been reported that adiponectin is also expressed by BAT [45, 139]. In addition to its main function in liver metabolism, adiponectin induces fatty acid oxidation and glucose uptake in skeletal muscles and regulates energy expenditure by affecting the hypothalamus [140].
Meteorin-like (METRNL)
In response to cold, METRNL is expressed as a circulating hormone by brown/beige adipocytes [141]. This batokine increases the penetration and activation of eosinophils. The production of IL-4 and IL-13 by eosinophils leads to the recruitment of M2-type macrophages [141]. Therefore, by recruiting eosinophils and M2-type macrophages, METRNL also increases BAT activity and WAT browning. It is thus considered as having therapeutic potential in the treatment of inflammatory diseases and metabolic disorders [141].
Wingless-related MMTV integration site 10b (WNT10b)
WNT10b is secreted by brown/beige adipocytes and has anabolic effects on bone formation [142]. Additionally, WNT10b ameliorates body weight and insulin sensitivity [143].
Thyroid hormones
Type II thyroxine 5´-deiodinase (DIO2) enzyme changes thyroxine (T4) into an active form of triiodothyronine (T3). DIO2 activity is strongly induced through noradrenergic stimulation. Thus, T3, the first endocrine factor, is crucial for inducing thermogenic activity in brown adipocytes [144].
Fibroblast growth factor 21 (FGF21)
As a member of the endocrine subfamily of FGFs, the adipo-myokine FGF21 is secreted by BAT and targets several organs and tissues, including the heart, brain, liver, pancreas, and WAT. BAT itself can be targeted through the autocrine actions of FGF21 batokine [86]. The various functions of FGF21 include (1) potent cardioprotective effects, (2) pleiotropic effects on hepatic metabolism and sympathetic outflow, (3) as a potent regulator of metabolic pathways with blood glucose-lowering and insulin-sensitizing effects, (4) control of lipolysis pathway in WAT, and (5) promotion of BAT thermogenesis and WAT browning [45, 145]. The specific tissues affected by FGF21 produced by BAT have not yet been fully characterized.
Chemokine (C-X-C motif) Ligand 14 (CXCL14)
In response to thermogenic stimuli, the batokine CXCL14 is secreted by brown adipocytes [146]. CXCL14 targets M2 cells or alternatively activated macrophages (AAMs). This function of CXCL14 highlights the ability of batokines to target immune system cells [86]. CXCL14 also boosts WAT browning and BAT activation [146].
Insulin-like growth factor-binding protein-2 (IGFBP2)
IGFBP2 is known to modulate the functions of IGF-1. IGFBP2 secretion by brown/beige adipocytes may significantly improve metabolic activities and differentiation of preadipocytes [147]. IGFBP2 directly stimulates osteoblast differentiation [148]. This batokine promotes skeletal changes and bone remodeling through its heparin-binding domain. Deletion of the IGFBP2 gene halts bone turnover, suggesting its potential in addressing skeletal abnormalities. [149].
Growth and differentiation factor-15 (GDF-15)
Against thermogenic stimuli, GDF-15 is released by brown/beige adipocytes. GDF-15 inhibits the proinflammatory activity of M1-type macrophages through a paracrine role [86, 150]. GDF-15 has been identified as a systemic marker in diseases ranging from cardiovascular diseases to cancers [86]. GDF-15 exerts anorectic effects via its function in the brainstem and controls energy balance [151, 152]. Thus, GDF-15 plays a role in different pathologies (anorexia, obesity, ischemia, and atherosclerosis) by virtue of its varied modes of action. Also, the endocrine role of GDF-15 will be significant in preventing several metabolic disorders [86, 150].
Ependymin-related protein 1 (EPDR1)
EPDR1 is a newly identified batokine that is released from brown and white adipocytes and is critical for modulating the homeostatic control of energy balance and thermogenic activity of brown adipocytes during the adipogenesis process [153].
Retinol-binding protein 4 (RBP4)
In mice, RBP4 is expressed in BAT that have been either exposed to cold or treated with PPARγ agonists [154]. Also, RBP4 gene expression has been shown in brown adipocytes in vitro [154]. RBP4 might play a key role in WAT browning [155]. In animal and human studies, RBP4 has been associated with systemic insulin resistance, dyslipidemia, type 2 diabetes, cardiometabolic, and other diseases [156]. However, mechanisms linking RBP4, impaired insulin sensitivity, glucose, and lipid metabolism are still not completely understood [156]. Therefore, further studies are needed to gain insight into the role of RBP4 in the initiation and progression of obesity-related diseases.
Phospholipid transfer protein (PLTP)
PLTP is a new batokine that targets the liver and increases circulating bile acids, increasing glucose uptake and BAT thermogenesis [157, 158].
Exosomal microRNAs
BAT activation leads to remarkable shifts in the number of exosomes secreted into circulation and the profile of exosomal miRNAs. Recently, the understanding of BAT has expanded by recognizing the functions of exosomal miRNAs [159, 160]. Specific exosomal miRNAs play a significant role in BAT [161]. For example, miR-92a is an exosomal miRNA that is inversely correlated with the thermogenic activation of BAT and could be applied as a possible serum biomarker to evaluate its functional effect on BAT mass and activity [160]. Additionally, BAT activation leads to the secretion of exosomes containing miR-99b, which exerts hepatic effects by regulating the expression and secretion of FGF21 batokine [159]. Apart from energy expenditure, BAT is believed to modulate body metabolism by regulating other vital organs via exosomal miRNAs. Exosomal miR-132-3p, derived from brown adipocytes, has been shown to downregulate the hepatic expression of lipogenic genes [162]. Hence, the exploration of miRNAs secreted by BAT, WAT, and beige AT, along with a deeper comprehension of their potential functions and specific tissue targets, presents promising avenues for future research. This comprehensive list of miRNAs is further detailed in the following section.
Other factors
A range of factors are released by brown/beige adipocytes in response to different stimuli, including neuromedin B and nesfatin-1 [163]. Neuromedin B and its receptor are highly expressed in AT. Cikes et al. suggested that neuromedin B does not change body weight and glucose homeostasis on a standard diet nor acts as an insulin‑releasing peptide [164]. Neuromedin B receptor disruption impairs adipogenesis in mice and 3T3-L1 cells. Therefore, neuromedin B receptor antagonism may help limit the increase in adiposity due to pre-adipocyte differentiation [165]. Nesfatin-1, a new depot-specific adipokine, is preferentially expressed in human and murine AT depots. Nesfatin-1 protein expression was markedly increased in high-fat-fed mice and decreased in food deprivation [166]. Also, nesfatin-1 promotes brown adipocyte differentiation by activating the mTOR signaling pathway and may be a promising approach for treating obesity [167]. In BAT, centrally acting nesfatin-1 can induce β3-adrenergic stimulation, an important factor for activating thermogenic genes, releasing heat from interscapular BAT, and ultimately increasing energy expenditure [168].
Brown adipocytes also produce biologically active molecules, such as thermogenic modulators like retinaldehyde and retinoic acid. Upon thermogenic activation, additional secretory factors such as FFAs and lactate are released by these adipocytes [133]. Adipokines secreted by AT participate in the metabolic variations of gestational diabetes mellitus (GDM). GDM is the most common metabolic disorder of pregnancy and has significant consequences for maternal and newborn health. Several studies have shown gene and/or protein expression of adipokines adiponectin, leptin, omentin-1, resistin, IL-1β, IL-6, IL-1RA, IL-10, TNF-α, SOCS3, visfatin, apelin, adrenomedullin, and nesfatin-1) in AT between GDM patients and controls at delivery [169]. Serum visfatin is a metabolic biomarker in obese patients with GDM [170].
Overall, brown and beige adipocytes secrete numerous factors that intricately regulate metabolism. Some stimulate AT activity, enhancing TG uptake and inducing thermogenic activity in brown and beige adipocytes. In contrast, certain factors act as negative regulators, suppressing thermogenesis and inhibiting energy wastage. These factors also interact with immune cells, such as macrophages and eosinophils, influencing BAT activity and promoting browning in WAT. They affect the vascular system, impacting BAT vascularization and influencing the differentiation of mesenchymal progenitor cells into brown and beige adipocytes. Some factors also exert endocrine effects, targeting organs like the liver, pancreas, brain, and heart. They control energy balance, regulate blood glucose, and influence insulin sensitivity. Furthermore, they can recruit immune cells, promote BAT activity, and enhance WAT browning, contributing to metabolic health. In response to various stimuli, such as cold exposure and thermogenic activation, brown adipocytes secrete exosomes containing specific miRNAs. These miRNAs are crucial in regulating BAT mass and activity, affecting energy expenditure and lipid metabolism in different tissues.
5 Regulatory microRNAs in adipose tissue
microRNAs are short, non-coding RNA molecules comprising almost 20–22 nucleotides that take part in RNA silencing and adjust the expression of many genes. miRNAs are necessary for the development, identification, and differentiation of adipocytes. Deleting the Dicer enzyme in adipocytes destroys the miRNA processing pathway and ultimately leads to abnormal distribution of adipocytes [159]. microRNAs derived from AT regulate glucose metabolism, thermogenesis, and insulin sensitivity [171, 172]. They have complex relationships with obesity, diabetes, and other obesity-related metabolic diseases such as T2DM and cardiovascular diseases, and they can serve as significant biomarkers for therapeutic purposes. Many microRNAs have been known to regulate important signaling pathways of the adipogenesis process in BAT, beige AT, and WAT by influencing transcription factors that boost or prevent the differentiation of adipocytes [173]. Several microRNAs, such as MiR-193b-365 cluster, MiR-182, MiR-203, MiR-328, MiR-129, MiR-378, MiR-30, MiR-32, and MiR-455, are considered as browning activators, while MiR-106b, MiR-93, MiR-34a, MiR-155, MiR-133, and MiR-27 are known as browning inhibitors (Fig. 4a). Figure 4b shows beiging inhibitor microRNAs (MiR-34a, MiR-155, MiR-133, MiR-27, MiR-125, MiR-378), and beiging promoting microRNAs (MiR-30, MiR-32, MiR-455, MiR-196a, MiR-let-7, MiR-26) in beige AT. An array of microRNAs with adipogenic (MiR-30a, MiR-143, MiR-17, MiR-181) and anti-adipogenic (MiR-107, MiR-103, MiR-27a, MiR-130, MiR-33, MiR-369-5p, MiR-221) properties has been identified in WAT (Fig. 4c) [161, 173,174,175].
Important regulatory microRNAs in BAT, beige AT, and WAT. a Browning inhibiting microRNAs: MiR-106b, MiR-93, MiR-34a, MiR-155, MiR-133, MiR-27. Browning activating microRNAs: MiR-365, MiR-193b, MiR-182, MiR-203, MiR-328, MiR-129, MiR-378, MiR-30, MiR-32, MiR-455. b Beiging inhibiting microRNAs: MiR-34a, MiR-155, MiR-133, MiR-27, MiR-125, MiR-378. Beiging promoting microRNAs: MiR-30, MiR-32, MiR-455, MiR-196a, MiR-let-7, MiR-26. Similar MiRs in BAT and beige AT are shown with a light–dark rectangle. c Anti-adipogenic microRNAs: MiR-107, MiR-103, MiR-27a, MiR-130, MiR-33, MiR-369-5p, MiR-221. Adipogenic microRNAs: MiR-30a, MiR-143, MiR-17, MiR-181
Upon additional energy intake, WAT undergoes dynamic alterations to reflect the equilibrium between energy intake and expenditure. This leads to augmented lipid storage and pre-adipocyte differentiation into mature adipocytes [176]. Pre-adipocyte differentiation is determined by variations in the microRNA expression pattern of WAT, including up-regulated microRNAs (e.g., MiR-103, MiR-107, MiR-143, MiR-26b, MiR-375, MiR-21, MiR-148a, and MiR-30) [173, 177,178,179,180,181] and down-regulated microRNAs (e.g., MiR-221, MiR-155, MiR-210, and MiR-125b) [173, 182, 183]. As the process of adipogenesis in WAT and BAT shows shared pathways, there is an overlap of microRNAs identified in both types of AT but having different effects [184, 185]. EVs, including exosomes and microvesicles, serve as primary carriers transporting microRNAs from producer cells to target cells. Table 2a and b show the functions and targets of each regulatory microRNA in BAT, beige AT, and WAT.
6 Therapeutic applications
Browning research is a rapidly evolving field with the potential to address a range of metabolic and chronic disorders, such as obesity, diabetes, and cardiovascular disease. Browning agents and nanomedicine-based strategies are two promising therapeutic approaches for browning. Browning agents are compounds that can promote the conversion of WAT into BAT. Nanomedicine-based strategies for browning involve the use of nanomaterials to deliver therapeutic agents to BAT with high precision. This allows for targeted and effective treatment of metabolic disorders. In this section, we will review the latest advances in the development and application of browning agents and nanomedicine-based strategies. We will also discuss the implications of browning for atherosclerosis, cancer, fertility, circadian systems, and disorders.
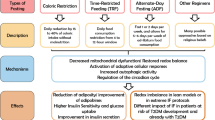
6.1 Browning agents
Beige adipocytes are a kind of adipocyte found in WAT depots, which can acquire a BAT-like phenotype with an augmented capacity for the thermogenic process, a phenomenon known as WAT browning [239]. The expression of important transcription factors such as PRDM16, PPARA, and UCP1 (as a hallmark of thermogenesis) has been observed in WAT [240]. Obesity and diabetes in epidemic proportions are significant worldwide health concerns, and the browning of WAT may hold promise as a target for treating and preventing metabolic disorders, including type 2 diabetes and cardiovascular diseases [241].
A growing number of browning agents [36] have been identified. Table 3 provides a complete list of these agents, extensively evaluated in human and animal models through in vitro and in vivo experiments. Some of the important browning agents to induce browning in WAT or protect against HFD-induced obesity include cold exposure, β-3 adrenergic receptor agonists (CL 316243, BRL 26830A), short-chain fatty acids (butyrate, propionate, acetate), dietary factors and plant-based compounds (capsaicin, resveratrol, berberine, fish oil, green tea extract, cinnamon, quercetin, curcumin, ginsenoside Rb1), nuclear receptors and ligands (farnesoid X receptor, liver X receptors), microRNAs (microRNA-32, microRNA-455), drug agents (thiazolidinediones, prostaglandin E2, gleevec, β-lapachone, SLIT2-C, artepillin C, adrenomedullin 2), inflammatory factors (IL-6, IL-4, IEX-1), hormonal factors (TH, PTH, PTHrP, GLP-1R, leptin, melatonin, NPs, irisin, FNDC4, maternal secretin), genetic factors (PTEN, Cox2, Foxc2, folliculin, Gq, and TGF-β/Smad3 pathway), batokines (FGF21, PTGDS, apelin, BMP7, BMP4, NPM3), exercise, PPAR agonists and signaling (rosiglitazone, ABHD6), metabolites (lactate, BHB, BAIBA, retinoic acid), and other factors (gut microbiota). However, the therapeutic use of browning agents [36] is confronted with various obstacles, and strategies to eliminate side effects and/or undesirable metabolic outcomes will be essential.
6.2 Nanomedicine-based strategies for browning of WAT
Recent advances in nanomedicine have resulted in the development of various strategies for the targeted delivery of browning agents to WAT. The oral administration or injection of browning agents often leads to undesired side effects, making developing tissue-specific drug delivery systems crucial. Various types of nanoparticles, including poly (lactide-co-glycolide) (PLGA), polyethylene glycol, polyethylenimine, lipid nanoparticles, and hepatitis B core (HBc) protein virus-like particles (VLPs), have been utilized for this purpose [242]. One study using ligand-coated resveratrol-encapsulated nanoparticles (L-Rnano) demonstrated the induction of differentiation of adipose stromal cells (ASCs) into beige adipocytes, subsequently leading to WAT browning, 40% reduction in fat mass, improved glucose and cholesterol homeostasis and decreased inflammation in obese C57BL6/J mice after biweekly intravenous administration for five weeks [243] (Fig. 5). These results indicated that the ASC-targeted nanoparticle delivery system of browning agents could be a promising technology in combating obesity and related metabolic disorders with high efficacy and low toxicity.
Illustration of L-Rnano designed to deliver R (resveratrol) to ASCs by Zu et al. [243] (with permission). L-Rnano delivers R into the ASCs through delta decorin receptor and stimulates their differentiation into beige adipocytes, subsequently leading to WAT browning, loss of body fat, and ameliorated metabolic health in HFD-induced obese C57BL/6J mice
Targeted nanoparticles containing rosiglitazone or a prostaglandin E2 analog (16,16-dimethyl PGE2), injected into the vasculature of WAT in mice, were also found to stimulate the browning of WAT and angiogenesis [244]. Transdermal drug delivery systems, such as microneedles and hydrogel patches, have been developed to overcome the challenges of penetrating the skin's intrinsic physiological barrier, resulting in increased delivery efficiency for browning agents [242, 245]. These nanomedicine-based strategies offer great potential for the specific delivery of browning agents to WAT, offering a new method for treating obesity and linked metabolic disorders.
6.3 Browning of WAT as a therapeutic approach to atherosclerosis
Atherosclerosis is a chronic lipid-induced inflammatory disease resulting from atheromatous plaques in medium- and large-sized arteries [246]. Physiological conditions such as cold exposure or β3-adrenergic agonists induce browning of WAT, which leads to an anti-atherogenic profile through the expenditure of FFAs and secretion of adiponectin, FGF21, and apelin [246]. In contrast, in WAT dysfunction in obesity, pro-atherogenic factors, such as FFAs, TNF-α, IL-6, resistin, and leptin, are secreted, which increase the development of atherosclerosis, internal plaque inflammation, and plaque vulnerability [246]. The epicardial AT exhibits a distinct lipid composition and is in close anatomical proximity to the heart tissue [8]. Therefore, WAT browning is considered a potential target in efforts to reduce the expansion of atherosclerotic plaques. Preclinical studies in mice models with preserved hepatic clearance of lipids have shown that browning of WAT by exposure to cold or β3-adrenergic receptor agonists leads to a reduction in the development of atherosclerotic plaques. However, in mice models with impaired hepatic clearance, the development of atherosclerotic lesions and plaque vulnerability is increased [246]. In the mouse model with conserved hepatic lipid clearance, the stimulation of WAT browning promoted by cold exposure, or the use of β3-adrenergic receptor agonists decreases the development of atherosclerotic plaques. In contrast, the growth of atherosclerotic lesions and plaque vulnerability is promoted in the mouse model with impaired hepatic lipid clearance [246]. Clinical studies have shown that people exposed to cold have increased WAT-derived brown-like AT differentiation and have smaller atherosclerotic plaques than people not exposed to cold. However, impaired hepatic clearance of lipids in atherosclerosis has not been investigated in humans [246].
BAT may also exert its effects through indirect mechanisms or by releasing lipid particles that influence systemic metabolism. For instance, in response to cold exposure, murine BAT produces small HDL particles that enhance HDL turnover, potentially affecting cholesterol transport to the liver [247] or modifying HDL's functional composition, which is relevant to atherosclerosis [248]. Recent clinical trials have attempted to detect thinner atherosclerotic lesions in patients with higher BAT activity. Although very few studies have shown a correlation between the induction of WAT browning and atherosclerosis, further research is nonetheless warranted in this exciting field. Strategies to maintain healthy arteries are a serious concern [246]. The study by Shi et al. have revealed that BAT-derived Nrg4 improves atherosclerosis in male mice. Nrg4, as a potential crosstalk factor between BAT and arteries, inhibits endothelial inflammation or adhesion responses, decreases leukocyte homing and macrophage gathering in plaques, improves plaque stability, and thus protects against endothelial injury and atherosclerosis via endothelial ErbB4–Akt–NF-κB signaling pathway. Therefore, Nrg4 may become a novel therapeutic target for atherosclerosis disease [249].
6.4 Brown adipose tissue and cancer
Insulin resistance and chronic inflammation in visceral fat may cause alterations in various molecules, which act on the tumor microenvironment to drive tumor progression [7]. BAT has recently emerged as a potential therapeutic target for cancer. Several studies have proposed that BAT may play a role in cancer-associated cachexia, a condition characterized by muscle wasting and weight loss that is common in cancer patients. However, the complex relationship between BAT and cancer is not yet fully understood. A retrospective study of cancer patients found that BAT was not associated with cachexia or increased mortality [313]. In contrast, another study showed that exosomal miR-155 from gastric cancer cells induced cancer-associated cachexia by suppressing adipogenesis and promoting brown adipose differentiation through C/EPBβ [314]. These findings suggest that the interaction between cancer and BAT may be tumor-specific and context-dependent.
In addition to its potential role in cachexia, BAT has also been implicated in tumor suppression. A recent study showed that cold-induced activation of BAT suppressed tumor growth by inducing a metabolic switch in cancer cells [315]. Another study found that cold-induced brown fat thermogenesis could starve tumor growth [316]. Similarly, a pilot study using FDG PET/CT found a relationship between BAT and breast cancer [317], and a decrease in BAT activity was related to weight gain during chemotherapy in early breast cancer patients [318]. Another study suggested active BAT may protect against cancer cachexia [319].
Overall, these studies indicate that the role of BAT in cancer is complex and may vary depending on the tumor type and stage, as well as other patient-specific factors. More research is needed to fully understand the relationship between BAT and cancer and discover the potential of BAT as a therapeutic goal for cancer.
6.5 Brown adipose tissue and fertility
Numerous studies have identified a connection between disrupted lipid metabolism and fertility issues [320,321,322]. Pink adipocytes are a female-specific cell type created in the mammary glands during pregnancy, lactation, and post-lactation periods from breast sWAT. Their main function is to secrete milk and store substantial amounts of lipids in the mammary glands during these periods. In the end phase of lactation, pink adipocytes turn into white and brown adipocytes [323]. In addition to its role in metabolism and thermoregulation, BAT has also been implicated in fertility. Several studies have investigated the potential link between BAT, ovarian aging, and male and female fertility. One study suggested that AT dysfunction could contribute to ovarian aging and decreased fertility in women [324]. In particular, the authors proposed that pro-inflammatory cytokines secreted by AT may lead to oxidative stress and inflammation in the ovaries, ultimately impairing ovarian function. However, more research is needed to understand the underlying mechanisms and potential therapeutic strategies for protecting ovarian function.
In male fertility, it has been demonstrated that diet-induced obesity can lead to impaired sperm quality and quantity. However, a mouse model study found that transplantation of BAT from lean mice into diet-induced obese mice improved fertility outcomes [325]. This suggests that BAT may have protective effects on male reproductive function. In a female fertility study using rats for investigating the potential use of rutin, a natural flavonoid, in activating BAT and improving outcomes in polycystic ovary syndrome (PCOS) [326], the authors found that rutin treatment increased BAT activity and improved ovarian function in rats with PCOS. Another rat study demonstrated similar results with cold treatment-induced BAT activation in PCOS [327]. BAT xenotransplantation from rats to mice extended the ovarian lifespan of aging mice, potentially by reducing levels of IL-6 and adiponectin to levels similar to those of young mice [328]. These results suggest that BAT may be a therapeutic target for improving reproductive outcomes in women with PCOS.
Finally, a study investigating the role of BAT in thermoregulation in newborn lambs found that fetal thyroidectomy led to decreased BAT activity and impaired thermoregulation [329]. This highlights the importance of BAT in maintaining proper body temperature and suggests that its dysfunction could negatively affect newborn health. Some of the well-known secretory factors produced by BAT include irisin, FGF21, and adiponectin. These factors have been implicated in regulating insulin sensitivity, glucose and lipid metabolism, and cardiovascular function. Interestingly, recent studies have also proposed that some of these secretory factors may directly or indirectly affect female reproductive function, raising the probability that BAT may be involved in regulating fertility [88, 330]. Recent evidence suggests that the secretome of brown adipocytes, including irisin and leptin, may enhance steroidogenesis in human ovarian granulosa cells, revealing potential mechanisms by which BAT can modulate female fertility [331]. These studies show that BAT may play a significant role in reproductive health and could be targeted for therapeutic applications.
6.6 Crosstalk between adipose tissue, circadian system, and circadian disorders
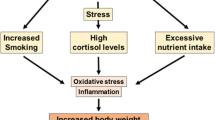
The circadian timing system governs the 24-h physiological rhythms and adapts the body to environmental changes. Disruptions to this system correlate with diverse health issues, including cancer, sleep disorders, behavioral problems, and metabolic disorders [332,333,334]. AT plays a central role in the circadian system by influencing human energy regulation. Circadian rhythms regulate adipose processes such as adipogenesis, lipolysis, WAT browning, BAT thermogenesis, and adipokine secretion. Disrupted circadian rhythms due to factors such as aging, shift work, and light exposure at night contribute to cardiovascular diseases and metabolic disorders such as diabetes, and obesity [332,333,334].
Chronotherapy is a growing field that optimizes treatment by aligning it with human circadian rhythms. It involves timing medications and targeting clock genes using circadian modulators to combat metabolic disorders [333]. Recent research highlights the role of circadian rhythms in human AT dynamics. Studies show that circadian misalignment exacerbates AT reduction in cardiac cachexia, emphasizing the potential benefits of stabilizing circadian rhythms in these cases [335].
BAT influences brain and environmental homeostasis, making it a focus in psychiatry [336]. Light exposure halts BAT thermogenesis, and prolonged daylight correlates with higher human body fat mass [337]. Dysregulated BAT may indirectly contribute to psychiatric disorders and suicide risk [338]. Second-generation antipsychotic drugs, while effective against neuropsychiatric disorders, are linked to metabolic issues, including abnormal weight gain, hyperglycemia, and dyslipidemia, partly due to their effects on BAT and WAT browning [339]. For example, clozapine and lithium lead to inhibition of BAT adipogenesis and weight gain as a side effect [340]. Understanding the intricate interplay between circadian systems, AT, and human metabolic and psychiatric health is crucial and requires further research in this emerging field.
7 Conclusion
Although considerable progress has been made in understanding brown/beige adipocyte secretomes, much is still to be learned about their actions and targets. Batokines, regulatory molecules secreted by brown/beige adipocyte secretomes, include a diversity of signaling molecules, such as metabolites, lipids, peptides, or microRNAs. Since microRNAs are thought to play an important regulatory role in critical genes involved in the differentiation and function of WAT, BAT, and beige ATs, their potential to serve as biomarkers in the maintenance of metabolic processes and as targets in the treatment of obesity-related cardio-metabolic diseases cannot be underestimated. Furthermore, the discovery of new browning agents in recent years represents promising approaches to effective therapies for obesity and associated metabolic disorders. Currently available knowledge suggests that further research is warranted on brown/beige adipocyte secretomes and their potential therapeutic applications.
Availability of data and material
Data and materials used in this review were obtained from published studies and are available from their respective sources as cited in the reference list.
Abbreviations
- AAMs:
-
Alternatively activated macrophages
- ABCA1:
-
Adenosine triphosphate–binding cassette transporter 1
- ABHD6:
-
Alpha/beta-hydrolase domain-containing 6
- AC:
-
Adenylyl cyclase
- ADAM17:
-
ADAM metallopeptidase domain 17
- AdipoR1:
-
Adiponectin receptor 1
- AMPK:
-
AMP-activated protein kinase
- ANGPTL8:
-
Angiopoietin-like 8
- aP2:
-
Adipocyte protein 2
- APCDD1:
-
Adenomatosis polyposis coli downregulated 1
- ARs:
-
Adrenergic receptors
- ASCs:
-
Adipose stromal cells
- ASK1:
-
Apoptosis signal-regulating kinase 1
- AT:
-
Adipose tissue
- ATGL:
-
Adipose triglyceride lipase
- Bace1:
-
Beta-site amyloid precursor protein-cleaving enzyme 1
- BAIBA:
-
Beta-aminoisobutyric acid
- BAT:
-
Brown adipose tissue
- BHB:
-
Beta-hydroxybutyrate
- BMPs:
-
Bone morphogenetic proteins
- C/EBPα:
-
CCAAT/enhancer-binding protein alpha
- C/EBPβ:
-
CCAAT/enhancer-binding protein beta
- C1–4:
-
Complex 1–4
- cAMP:
-
Cyclic adenosine 3′,5′-monophosphate
- CD36:
-
Cluster of differentiation 36
- CDK6:
-
Cell division protein kinase 6
- CMKLR1:
-
Chemokine-like receptor 1
- CoQ:
-
Co-enzyme Q
- Creb:
-
CAMP-response element binding protein
- CXCL14:
-
Chemokine (C-X-C motif) ligand 14
- Cyto C:
-
Cytochrome C
- 12,13-diHOME:
-
Lipokine 12,13-dihydroxy-9Z-octadecenoic acid
- DIO2:
-
Type II thyroxine 5´-deiodinase
- DLL4:
-
Delta-like protein 4
- EBF2:
-
Early B-cell transcription factor 2
- EGF:
-
Epidermal growth factor
- Egr1:
-
Early growth factor response 1
- EPCs:
-
Endothelial progenitor cells
- EPDR1:
-
Ependymin-related protein 1
- ERK5:
-
Extracellular signal-regulated kinase 5
- ET-1:
-
Endothelin-1
- ETS1:
-
E26 transformation–specific-1
- FABP4:
-
Fatty acid-binding protein 4
- FAs:
-
Fatty acids
- Fasn:
-
Fatty acid synthase
- FATP:
-
Fatty acid transport protein
- FBXl19:
-
F-box and leucine-rich repeat protein 19
- FFAs:
-
Free fatty acids
- FGF21:
-
Fibroblast growth factor 21
- Fgfr1:
-
Fibroblast growth factor receptor 1
- FNDC4:
-
Fibronectin type III domain-containing protein
- FXR:
-
Farnesoid X receptor
- GDF-15:
-
Growth differentiation factor-15
- GDF-8:
-
Growth differentiation factor-8
- GDM:
-
Gestational diabetes mellitus
- GLP-1R:
-
Glucagon-like peptide-1 receptor
- GLUT:
-
Glucose transporter
- GPCR-1:
-
G protein-coupled receptor-1
- H2O2 :
-
Hydrogen peroxide
- HBc:
-
Hepatitis B core
- HDL:
-
High-density lipoprotein
- HFD:
-
High-fat diet
- Hif1an:
-
Hypoxia-inducible factor 1 subunit alpha inhibitor
- HLA-DR:
-
Human leukocyte antigen-DR
- HMGA2:
-
High-mobility group AT-hook 2
- Hoxc8:
-
Homeobox C8
- IEX-1:
-
Immediate early response gene X-1
- IFNG:
-
Interferon-gamma
- IGF-1:
-
Insulin-like growth factor 1
- IGF2R:
-
Insulin-like growth factor 2 receptor
- IGFBP2:
-
Insulin-like growth factor-binding protein-2
- IL:
-
Interleukin
- IMM:
-
Inner mitochondrial membrane
- Insig1:
-
Insulin-induced gene 1
- ISCT:
-
International Society for Cellular Therapy
- Klf4:
-
Kruppel-like factor 4
- -PGDS:
-
Lipocalin prostaglandin D synthase
- L-Rnano:
-
Ligand-coated resveratrol-encapsulated nanoparticles
- LXRs:
-
Liver X receptors
- MAP2K5:
-
Mitogen-activated protein kinase 5
- MCP-1:
-
Monocyte chemotactic protein-1
- MEF2D:
-
Myocyte enhancer factor 2D
- METRNL:
-
Meteorin-like
- MMP11:
-
Matrix metalloproteinase 11
- MRI:
-
Magnetic resonance imaging
- MSCs:
-
Mesenchymal stem cells
- Myf5:
-
Myogenic transcription factor 5
- NADR:
-
Noradrenaline
- NAFLD:
-
Non-alcoholic fatty liver disease
- NDUFA4:
-
NADH dehydrogenase (ubiquinone) 1 alpha subcomplex 4
- NGF:
-
Nerve growth factor
- NO:
-
Nitric oxide
- NPM3:
-
Nucleophosmin3
- NRG4:
-
Neuregulin -4
- Oplah:
-
5-Oxoprolinase
- Orp8:
-
Oxysterol-binding protein-related protein 8
- PCOS:
-
Polycystic ovary syndrome
- Pde1b:
-
Phosphodiesterase 1b
- Pdgfr2:
-
Platelet-derived growth factor receptor 2
- PGC1α:
-
Peroxisome proliferator-activated receptor gamma, coactivator 1 alpha
- Pgc1b:
-
Peroxisome proliferator-activated receptor gamma, coactivator 1 beta
- PKA:
-
Protein kinase A
- PLGA:
-
Poly (lactide-co-glycolide)
- PLTP:
-
Phospholipid transfer protein
- PM20D1:
-
Peptidase M20 domain containing 1
- PPARA:
-
Peroxisome proliferator-activated receptor alpha
- PPARγ:
-
Peroxisome proliferator-activated receptor gamma
- PRDM16:
-
PR domain-containing 16
- PTEN:
-
Phosphatase and tensin homolog deleted on chromosome 10
- PTGDS:
-
Prostaglandin D synthase
- PTH:
-
Parathyroid hormone
- PTHrP:
-
Parathyroid hormone-related protein
- RAI14:
-
Retinoic acid-induced protein 14
- RBP4:
-
Retinol-binding protein 4
- Rip140:
-
Receptor-interacting protein 140
- Runx1t1:
-
Runt-related transcription factor 1; translocated to, 1
- SIRT1:
-
Sirtuin 1
- sLR11:
-
Soluble form of the low-density lipoprotein receptor relative LR11
- STAT1:
-
Signal transducer and activator of transcription 1
- sWAT:
-
Subcutaneous WAT
- T2DM:
-
Type 2 diabetes mellitus
- T3:
-
Triiodothyronine
- T4:
-
Thyroxine
- TG:
-
Triglyceride
- TGFBR2:
-
Transforming growth factor beta receptor 2
- TGF-β:
-
Transforming growth factor-beta
- TNF-α:
-
Tumor necrosis factor-alpha
- Tob1:
-
Transducer of ERBB2-1
- UCP1:
-
Uncoupling protein 1
- VEGF-A:
-
Vascular endothelial growth factor A
- VLPs:
-
Virus-like particles
- vWAT:
-
Visceral WAT
- WAT:
-
White adipose tissue
- WNT10b:
-
Wingless-related MMTV integration Site 10b
References
Frei IC, et al. Adipose mTORC2 is essential for arborization of sensory neurons in white adipose tissue and whole-body energy homeostasis. bioRxiv. 2022. https://doi.org/10.1101/2022.03.21.485116.
Sasaki N, Maeda R, Ozono R, Yoshimura K, Nakano Y, Higashi Y. Adipose tissue insulin resistance predicts the incidence of hypertension: The hiroshima study on glucose metabolism and cardiovascular diseases. Hypertens Res. 2022. https://doi.org/10.1038/s41440-022-00987-0.
Inoue O, et al. Single cell transcriptomics identifies adipose tissue CD271+ progenitors for enhanced angiogenesis in limb ischemia. bioRxiv. 2023. https://doi.org/10.1101/2023.02.09.527726.
Castela I, et al. Decreased adiponectin/leptin ratio relates to insulin resistance in adults with obesity. Am J Physiol-Endocrinolo Metabol. 2023. https://doi.org/10.1152/ajpendo.00273.2022.
Soler-Vázquez MC, Mera P, Zagmutt S, Serra D, Herrero L. New approaches targeting brown adipose tissue transplantation as a therapy in obesity. Biochem Pharmacol. 2018. https://doi.org/10.1016/j.bcp.2018.07.022.
Emont MP, et al. A single-cell atlas of human and mouse white adipose tissue. Nature. 2022. https://doi.org/10.1038/s41586-022-04518-2.
Ungefroren H, Gieseler F, Fliedner S, Lehnert H. Obesity and cancer. Horm Mol Biol Clin Invest. 2015. https://doi.org/10.1515/hmbci-2014-0046.
Pezeshkian M, et al. Fatty acid composition of epicardial and subcutaneous human adipose tissue. Metab Syndr Relat Disord. 2009. https://doi.org/10.1089/met.2008.0056.
Ghahremanpour F, Firoozrai M, Darabi M, Zavarei A, Mohebbi A. Adipose tissue trans fatty acids and risk of coronary artery disease: a case-control study. Ann Nutr Metab. 2008. https://doi.org/10.1159/000114291.
Poissonnet CM, Burdi AR, Garn SM. The chronology of adipose tissue appearance and distribution in the human fetus. Early Human Dev. 1984. https://doi.org/10.1016/0378-3782(84)90106-3.
Spalding KL, et al. Impact of fat mass and distribution on lipid turnover in human adipose tissue. Nat Commun. 2017. https://doi.org/10.1038/ncomms15253.
Sanchez-Gurmaches J, Hsiao W-Y, Guertin DA. Highly selective in vivo labeling of subcutaneous white adipocyte precursors with Prx1-Cre. Stem Cell Rep. 2015. https://doi.org/10.1016/j.stemcr.2015.02.008.
Sugihara H, Yonemitsu N, Miyabara S, Yun K. Primary cultures of unilocular fat cells: characteristics of growth in vitro and changes in differentiation properties. Differentiation. 1986. https://doi.org/10.1111/j.1432-0436.1986.tb00381.x.
Wei Wu J, Wang SP, Casavant S, Moreau A, Yang GS, Mitchell GA. Fasting energy homeostasis in mice with adipose deficiency of desnutrin/adipose triglyceride lipase. Endocrinology. 2012. https://doi.org/10.1210/en.2011-1518.
Morak M, et al. Adipose triglyceride lipase (ATGL) and hormone-sensitive lipase (HSL) deficiencies affect expression of lipolytic activities in mouse adipose tissues. Mol Cell Proteomics. 2012. https://doi.org/10.1074/mcp.M111.015743.
Bartness TJ, Liu Y, Shrestha YB, Ryu V. Neural innervation of white adipose tissue and the control of lipolysis. Front Neuroendocrinol. 2014. https://doi.org/10.1016/j.yfrne.2014.04.001.
Galic S, Oakhill JS, Steinberg GR. Adipose tissue as an endocrine organ. Mol Cell Endocrinol. 2010. https://doi.org/10.1016/j.mce.2009.08.018.
Merklin RJ. Growth and distribution of human fetal brown fat. Anat Rec. 1974. https://doi.org/10.1002/ar.1091780311.
Loncar D. Development of thermogenic adipose tissue. Int J Dev Biol. 1991. Available: https://www.ncbi.nlm.nih.gov/pubmed/1814413.
Harms M, Seale P. Brown and beige fat: development, function and therapeutic potential. Nat Med. 2013. https://doi.org/10.1038/nm.3361.
Cypess AM, et al. Anatomical localization, gene expression profiling and functional characterization of adult human neck brown fat. Nat Med. 2013. https://doi.org/10.1038/nm.3112.
Khanna A, Branca RT. Detecting brown adipose tissue activity with BOLD MRI in mice. Magn Reson Med. 2012. https://doi.org/10.1002/mrm.24118.
Frontini A, Cinti S. Distribution and development of brown adipocytes in the murine and human adipose organ. Cell Metab. 2010. https://doi.org/10.1016/j.cmet.2010.03.004.
White JD, Dewal RS, Stanford KI. The beneficial effects of brown adipose tissue transplantation. Mol Aspects Med. 2019. https://doi.org/10.1016/j.mam.2019.06.004.
Fedorenko A, Lishko PV, Kirichok Y. Mechanism of fatty-acid-dependent UCP1 uncoupling in brown fat mitochondria. Cell. 2012. https://doi.org/10.1016/j.cell.2012.09.010.
Frontini A, Cinti S. Distribution and development of brown adipocytes in the murine and human adipose organ. Cell Metab. 2010. https://doi.org/10.1016/j.cmet.2010.03.004.
McNeill BT, Suchacki KJ, Stimson RH. MECHANISMS IN ENDOCRINOLOGY: Human brown adipose tissue as a therapeutic target: warming up or cooling down? Eur J Endocrinol. 2021. https://doi.org/10.1530/EJE-20-1439.
Riis-Vestergaard MJ, et al. Beta-1 and not beta-3 adrenergic receptors may be the primary regulator of human brown adipocyte metabolism. J Clin Endocrinol Metab. 2020. https://doi.org/10.1210/clinem/dgz298.
Blondin DP, et al. Human brown adipocyte thermogenesis is driven by β2-AR stimulation. Cell Metab. 2020. https://doi.org/10.1016/j.cmet.2020.07.005.
Kajimura S, Saito M. A new era in brown adipose tissue biology: molecular control of brown fat development and energy homeostasis. Annu Rev Physiol. 2014. https://doi.org/10.1146/annurev-physiol-021113-170252.
Bertholet AM, Kirichok Y. The mechanism FA-dependent H+ transport by UCP1. Brown Adipose Tissue. 2018. https://doi.org/10.1007/164_2018_138.
de Jong JM, Larsson O, Cannon B, Nedergaard J. A stringent validation of mouse adipose tissue identity markers. Am J Physiol Endocrinol Metab. 2015. https://doi.org/10.1152/ajpendo.00023.2015.
Cheng L, et al. Brown and beige adipose tissue: a novel therapeutic strategy for obesity and type 2 diabetes mellitus. Adipocyte. 2021. https://doi.org/10.1080/21623945.2020.1870060.
Ussar S, et al. ASC-1, PAT2 and P2RX5 are cell surface markers for white, beige, and brown adipocytes. Sci Transl Med. 2014. https://doi.org/10.1126/scitranslmed.3008490.
Medina-Gómez G. Mitochondria and endocrine function of adipose tissue. Best Pract Res Clin Endocrinol Metab. 2012. https://doi.org/10.1016/j.beem.2012.06.002.
Wankhade UD, Shen M, Yadav H, Thakali KM. Novel browning agents, mechanisms, and therapeutic potentials of brown adipose tissue. Biomed Res Int. 2016. https://doi.org/10.1155/2016/2365609.
Wu J, et al. Beige adipocytes are a distinct type of thermogenic fat cell in mouse and human. Cell. 2012. https://doi.org/10.1016/j.cell.2012.05.016.
Sharp LZ, et al. Human BAT possesses molecular signatures that resemble beige/brite cells. PLoS ONE. 2012. https://doi.org/10.1371/journal.pone.0049452.
Mahadik SR, Lele RD, Saranath D, Seth A, Parikh V. Uncoupling protein-2 (UCP2) gene expression in subcutaneous and omental adipose tissue of Asian Indians: Relationship to adiponectin and parameters of metabolic syndrome. Adipocyte. 2012. https://doi.org/10.4161/adip.19671.
Acharya A, et al. miR-26 suppresses adipocyte progenitor differentiation and fat production by targeting Fbxl19. Genes Dev. 2019. https://doi.org/10.1101/gad.328955.119.
Altshuler-Keylin S, et al. Beige adipocyte maintenance is regulated by autophagy-induced mitochondrial clearance. Cell Metab. 2016. https://doi.org/10.1016/j.cmet.2016.08.002.
Merlin J, et al. Could burning fat start with a brite spark? Pharmacological and nutritional ways to promote thermogenesis. Mol Nutr. 2016. https://doi.org/10.1002/mnfr.201500251.
Wang GX, Zhao XY, Lin JD. The brown fat secretome: metabolic functions beyond thermogenesis. Trends Endocrinol Metab. 2015. https://doi.org/10.1016/j.tem.2015.03.002.
Vargas-Castillo A, Torres N, Tovar AR. Endocrine regulation of brown and beige adipose tissue. Cell Endocrinol Health Dis. 2021. https://doi.org/10.1016/B978-0-12-819801-8.00012-0.
Ahmad B, Vohra MS, Saleemi MA, Serpell CJ, Fong IL, Wong EH. Brown/Beige adipose tissues and the emerging role of their secretory factors in improving metabolic health: The batokines. Biochimie. 2021. https://doi.org/10.1016/j.biochi.2021.01.015.
Wang Y-L, Lin S-P, Hsieh PC, Hung S-C. Concomitant beige adipocyte differentiation upon induction of mesenchymal stem cells into brown adipocytes. Biochem Biophys Res Commun. 2016. https://doi.org/10.1016/j.bbrc.2016.08.008.
Garcia RA, Roemmich JN, Claycombe KJ. Evaluation of markers of beige adipocytes in white adipose tissue of the mouse. Nutr Metab (Lond). 2016. https://doi.org/10.1186/s12986-016-0081-2.
Cedikova M, et al. Mitochondria in white, brown, and beige adipocytes. Stem Cells Int. 2016. https://doi.org/10.1155/2016/6067349.
Bartelt A, Heeren J. Adipose tissue browning and metabolic health. Nat Rev Endocrinol. 2014. https://doi.org/10.1038/nrendo.2013.204.
Lidell ME, et al. Evidence for two types of brown adipose tissue in humans. Nat Med. 2013. https://doi.org/10.1038/nm.3017.
Ladoux A, Peraldi P, Chignon-Sicard B, Dani C. Distinct shades of adipocytes control the metabolic roles of adipose tissues: from their origins to their relevance for medical applications. Biomedicine. 2021. https://doi.org/10.3390/biomedicines9010040.
Suchacki KJ, Stimson RH. Nutritional regulation of human brown adipose tissue. Nutrients. 2021. https://doi.org/10.3390/nu13061748.
Giralt M, Villarroya F. White, brown, beige/brite: different adipose cells for different functions? Endocrinology. 2013. https://doi.org/10.1210/en.2013-1403.
Villarroya F, Cereijo R, Gavaldà-Navarro A, Villarroya J, Giralt M. Inflammation of brown/beige adipose tissues in obesity and metabolic disease. J Intern Med. 2018. https://doi.org/10.1111/joim.12803.
Auger C, Kajimura S. Adipose tissue remodeling in pathophysiology. Annu Rev Pathol. 2023. https://doi.org/10.1146/annurev-pathol-042220-023633.
Park A, Kim WK, Bae KH. Distinction of white, beige and brown adipocytes derived from mesenchymal stem cells. World J Stem Cells. 2014. https://doi.org/10.4252/wjsc.v6.i1.33.
Corvera S, Gealekman O. Adipose tissue angiogenesis: impact on obesity and type-2 diabetes. Biochim Biophys Acta. 2014. https://doi.org/10.1016/j.bbadis.2013.06.003.
Lemoine AY, Ledoux S, Larger E. Adipose tissue angiogenesis in obesity. Thromb Haemost. 2013. https://doi.org/10.1160/TH13-01-0073.
Peschechera A, Eckel J. “Browning” of adipose tissue–regulation and therapeutic perspectives. Arch Physiol Biochem. 2013. https://doi.org/10.3109/13813455.2013.796995.
Jespersen NZ, et al. A classical brown adipose tissue mRNA signature partly overlaps with brite in the supraclavicular region of adult humans. Cell Metab. 2013. https://doi.org/10.1016/j.cmet.2013.04.011.
Dominici M, et al. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy. 2006. https://doi.org/10.1080/14653240600855905.
Sanchez-Gurmaches J, Hung C-M, Sparks CA, Tang Y, Li H, Guertin DA. PTEN loss in the Myf5 lineage redistributes body fat and reveals subsets of white adipocytes that arise from Myf5 precursors. Cell Metabol. 2012. https://doi.org/10.1016/j.cmet.2012.08.003.
Lepper C, Fan CM. Inducible lineage tracing of Pax7-descendant cells reveals embryonic origin of adult satellite cells. Genesis. 2010. https://doi.org/10.1002/dvg.20630.
Timmons JA, et al. Myogenic gene expression signature establishes that brown and white adipocytes originate from distinct cell lineages. PNAS. 2007. https://doi.org/10.1073/pnas.0610615104.
Koenen M, Hill MA, Cohen P, Sowers JR. Obesity, adipose tissue and vascular dysfunction. Circ Res. 2021. https://doi.org/10.1161/CIRCRESAHA.121.318093.
Tseng YH, et al. New role of bone morphogenetic protein 7 in brown adipogenesis and energy expenditure. Nature. 2008. https://doi.org/10.1038/nature07221.
Harms MJ, et al. Prdm16 is required for the maintenance of brown adipocyte identity and function in adult mice. Cell Metab. 2014. https://doi.org/10.1016/j.cmet.2014.03.007.
Wang W, et al. Ebf2 is a selective marker of brown and beige adipogenic precursor cells. PNAS. 2014. https://doi.org/10.1073/pnas.1412685111.
Rosen ED, MacDougald OA. Adipocyte differentiation from the inside out. Nat Rev Mol Cell Biol. 2006. https://doi.org/10.1038/nrm2066.
Schulz TJ, Tseng Y-H. Brown adipose tissue: development, metabolism and beyond. Biochem J. 2013. https://doi.org/10.1042/BJ20130457.
Okla M, Ha J-H, Temel RE, Chung S. BMP7 drives human adipogenic stem cells into metabolically active beige adipocytes. Lipids. 2015. https://doi.org/10.1007/s11745-014-3981-9.
Elsen M, et al. BMP4 and BMP7 induce the white-to-brown transition of primary human adipose stem cells. Am J Physiol Cell Physiol. 2014. https://doi.org/10.1152/ajpcell.00290.2013.
Xue R, et al. Role of bone morphogenetic protein 4 in the differentiation of brown fat-like adipocytes. Am J Physiol Endocrinol Metab. 2014. https://doi.org/10.1152/ajpendo.00119.2013.
Chu D-T, Gawronska-Kozak B. Brown and brite adipocytes: Same function, but different origin and response. Biochimie. 2017. https://doi.org/10.1016/j.biochi.2017.04.017.
Lasar D, et al. Peroxisome proliferator activated receptor gamma controls mature brown adipocyte inducibility through glycerol kinase. Cell Rep. 2018. https://doi.org/10.1016/j.celrep.2017.12.067.
Puigserver P, Wu Z, Park CW, Graves R, Wright M, Spiegelman BM. A cold-inducible coactivator of nuclear receptors linked to adaptive thermogenesis. Cell. 1998. https://doi.org/10.1016/S0092-8674(00)81410-5.
Wu Z, et al. Mechanisms controlling mitochondrial biogenesis and respiration through the thermogenic coactivator PGC-1. Cell. 1999. https://doi.org/10.1016/S0092-8674(00)80611-X.
An Y, et al. A molecular switch regulating cell fate choice between muscle progenitor cells and brown adipocytes. Dev Cell. 2017. https://doi.org/10.1016/j.devcel.2017.04.012.
Seale P, et al. PRDM16 controls a brown fat/skeletal muscle switch. Nature. 2008. https://doi.org/10.1038/nature07182.
Seale P, et al. Transcriptional control of brown fat determination by PRDM16. Cell Metab. 2007. https://doi.org/10.1016/j.cmet.2007.06.001.
Rajakumari S, et al. EBF2 determines and maintains brown adipocyte identity. Cell Metab. 2013. https://doi.org/10.1016/j.cmet.2013.01.015.
Rui L. Brown and beige adipose tissues in health and disease. Compr Physiol. 2017. https://doi.org/10.1002/cphy.c170001.
Ikeda K, Maretich P, Kajimura S. The common and distinct features of brown and beige adipocytes. Trends Endocrinol Metab. 2018. https://doi.org/10.1016/j.tem.2018.01.001.
Rosenwald M, Wolfrum C. The origin and definition of brite versus white and classical brown adipocytes. Adipocyte. 2014. https://doi.org/10.4161/adip.26232.
Villarroya J, Cereijo R, Villarroya F. An endocrine role for brown adipose tissue? Am J Physiol Endocrinol Metab. 2013. https://doi.org/10.1152/ajpendo.00250.2013.
Villarroya J, Cereijo R, Gavaldà-Navarro A, Peyrou M, Giralt M, Villarroya F. New insights into the secretory functions of brown adipose tissue. J Endocrinol. 2019. https://doi.org/10.1530/JOE-19-0295.
Villarroya F, Gavaldà-Navarro A, Peyrou M, Villarroya J, Giralt M. The lives and times of brown adipokines. Trends Endocrinol Metab. 2017. https://doi.org/10.1016/j.tem.2017.10.005.
Villarroya F, Cereijo R, Villarroya J, Giralt M. Brown adipose tissue as a secretory organ. Nat Rev Endocrinol. 2017. https://doi.org/10.1038/nrendo.2016.136.
Villarroya F, Giralt M. The beneficial effects of brown fat transplantation: further evidence of an endocrine role of brown adipose tissue. Endocrinology. 2015. https://doi.org/10.1210/en.2015-1423.
Lynes MD, et al. The cold-induced lipokine 12, 13-diHOME promotes fatty acid transport into brown adipose tissue. Nat Med. 2017. https://doi.org/10.1038/nm.4297.
García-Alonso V, et al. Prostaglandin E2 exerts multiple regulatory actions on human obese adipose tissue remodeling, inflammation, adaptive thermogenesis and lipolysis. PLoS ONE. 2016. https://doi.org/10.1371/journal.pone.0153751.
Gnad T, et al. Adenosine activates brown adipose tissue and recruits beige adipocytes via A2A receptors. Nature. 2014. https://doi.org/10.1038/nature13816.
Boon MR, et al. Peripheral cannabinoid 1 receptor blockade activates brown adipose tissue and diminishes dyslipidemia and obesity. FASEB J. 2014. https://doi.org/10.1096/fj.13-247643.
Krott LM, et al. Endocannabinoid regulation in white and brown adipose tissue following thermogenic activation. J Lipid Res. 2016. https://doi.org/10.1194/jlr.M065227.
Whittle AJ, et al. Soluble LR11/SorLA represses thermogenesis in adipose tissue and correlates with BMI in humans. Nat Commun. 2015. https://doi.org/10.1038/ncomms9951.
Steculorum SM, et al. AgRP neurons control systemic insulin sensitivity via myostatin expression in brown adipose tissue. Cell. 2016. https://doi.org/10.1016/j.cell.2016.02.044.
Kong X, et al. Brown adipose tissue controls skeletal muscle function via the secretion of myostatin. Cell Metab. 2018. https://doi.org/10.1016/j.cmet.2018.07.004.
Singh R, Braga M, Pervin S. Regulation of brown adipocyte metabolism by myostatin/follistatin signaling. Front Cell Dev Biol. 2014. https://doi.org/10.3389/fcell.2014.00060.
Braga M, Pervin S, Norris K, Bhasin S, Singh R. Inhibition of in vitro and in vivo brown fat differentiation program by myostatin. Obesity (Silver Spring). 2013. https://doi.org/10.1002/oby.20117.
Singh R, et al. Follistatin targets distinct pathways to promote brown adipocyte characteristics in brown and white adipose tissues. Endocrinology. 2017. https://doi.org/10.1210/en.2016-1607.
Schulz TJ, et al. Brown-fat paucity due to impaired BMP signalling induces compensatory browning of white fat. Nature. 2013. https://doi.org/10.1038/nature11943.
Schulz TJ, et al. Identification of inducible brown adipocyte progenitors residing in skeletal muscle and white fat. Proc Natl Acad Sci U S A. 2011. https://doi.org/10.1073/pnas.1010929108.
Qian SW, et al. BMP4-mediated brown fat-like changes in white adipose tissue alter glucose and energy homeostasis. Proc Natl Acad Sci U S A. 2013. https://doi.org/10.1073/pnas.1215236110.
Whittle AJ, et al. BMP8B increases brown adipose tissue thermogenesis through both central and peripheral actions. Cell. 2012. https://doi.org/10.1016/j.cell.2012.02.066.
Grefhorst A, van den Beukel JC, van Houten ELA, Steenbergen J, Visser JA, Themmen AP. Estrogens increase expression of bone morphogenetic protein 8b in brown adipose tissue of mice. Biol Sex Differ. 2015. https://doi.org/10.1186/s13293-015-0025-y.
Urisarri A, et al. BMP8 and activated brown adipose tissue in human newborns. Nat Commun. 2021. https://doi.org/10.1038/s41467-021-25456-z.
Svensson KJ, et al. A secreted Slit2 fragment regulates adipose tissue thermogenesis and metabolic function. Cell Metab. 2016. https://doi.org/10.1016/j.cmet.2016.01.008.
Kang YE, Choung S, Lee JH, Kim HJ, Ku BJ. The role of circulating Slit2, the one of the newly batokines, in human diabetes mellitus. Endocrinol Metab. 2017. https://doi.org/10.3803/EnM.2017.32.3.383.
Long JZ, et al. The secreted enzyme PM20D1 regulates lipidated amino acid uncouplers of mitochondria. Cell. 2016. https://doi.org/10.1016/j.cell.2016.05.071.
Hansen IR, Jansson KM, Cannon B, Nedergaard J. Contrasting effects of cold acclimation versus obesogenic diets on chemerin gene expression in brown and brite adipose tissues. Biochim Biophys Acta. 2014. https://doi.org/10.1016/j.bbalip.2014.09.003.
Rourke JL, Muruganandan S, Dranse HJ, McMullen NM, Sinal CJ. Gpr1 is an active chemerin receptor influencing glucose homeostasis in obese mice. J Endocrinol. 2014. https://doi.org/10.1530/JOE-14-0069.
Klepac K, et al. The Gq signalling pathway inhibits brown and beige adipose tissue. Nat Commun. 2016. https://doi.org/10.1038/ncomms10895.
Mahdaviani K, Chess D, Wu Y, Shirihai O, Aprahamian TR. Autocrine effect of vascular endothelial growth factor-A is essential for mitochondrial function in brown adipocytes. Metabolism. 2016. https://doi.org/10.1016/j.metabol.2015.09.012.
Shimizu I, et al. Vascular rarefaction mediates whitening of brown fat in obesity. J Clin Invest. 2014. https://doi.org/10.1172/JCI71643.
Nisoli E, Clementi E, Tonello C, Sciorati C, Briscini L, Carruba MO. Effects of nitric oxide on proliferation and differentiation of rat brown adipocytes in primary cultures. Br J Pharmacol. 1998. https://doi.org/10.1038/sj.bjp.0702131.
Villarroya F, Gavaldà-Navarro A, Peyrou M, Villarroya J, Giralt M. Brown adipokines. Brown Adipose Tissue. 2019. https://doi.org/10.1007/164_2018_119.
Roberts LD, et al. Inorganic nitrate promotes the browning of white adipose tissue through the nitrate-nitrite-nitric oxide pathway. Diabetes. 2015. https://doi.org/10.2337/db14-0496.
Becerril S, et al. Deletion of inducible nitric-oxide synthase in leptin-deficient mice improves brown adipose tissue function. PLoS ONE. 2010. https://doi.org/10.1371/journal.pone.0010962.
Vilela VR, et al. Adipocyte-specific Nos2 deletion improves insulin resistance and dyslipidemia through brown fat activation in diet-induced obese mice. Mol Metabol. 2022. https://doi.org/10.1016/j.molmet.2022.101437.
Becerril S, et al. Targeted disruption of the iNOS gene improves adipose tissue inflammation and fibrosis in leptin-deficient ob/ob mice: role of tenascin C. Int J Obes. 2018. https://doi.org/10.1038/s41366-018-0005-5.
Dallaire P, et al. Obese mice lacking inducible nitric oxide synthase are sensitized to the metabolic actions of peroxisome proliferator–activated receptor-γ agonism. Diabetes. 2008. https://doi.org/10.2337/db08-0540.
Pellegrinelli V, Carobbio S, Vidal-Puig AJD. Adipose tissue plasticity: how fat depots respond differently to pathophysiological cues. Diabetologia. 2016. https://doi.org/10.1007/s00125-016-3933-4.
Gunawardana SC, Piston DW. Insulin-independent reversal of type 1 diabetes in nonobese diabetic mice with brown adipose tissue transplant. Am J Physiol Endocrinol Metab. 2015. https://doi.org/10.1152/ajpendo.00570.2014.
Gunawardana SC, Piston DW. Reversal of type 1 diabetes in mice by brown adipose tissue transplant. Diabetes. 2012. https://doi.org/10.2337/db11-0510.
Gunawardana SC, Piston DW. Insulin-independent reversal of type 1 diabetes in nonobese diabetic mice with brown adipose tissue transplant. Am J Physiol Endocrinol Metab. 2015. https://doi.org/10.1152/ajpendo.00570.2014.
Friederich-Persson M, Nguyen Dinh Cat A, Persson P, Montezano AC, Touyz RM. Brown adipose tissue regulates small artery function through NADPH oxidase 4–derived hydrogen peroxide and redox-sensitive protein kinase G-1α. Arterioscler Thromb Vasc Biol. 2017. https://doi.org/10.1161/ATVBAHA.116.308659.
Fu Z, Yao F, Abou-Samra AB, Zhang R. Lipasin, thermoregulated in brown fat, is a novel but atypical member of the angiopoietin-like protein family. Biochem Biophys Res Commun. 2013. https://doi.org/10.1016/j.bbrc.2012.12.025.
Zhang R, Abou-Samra AB. Emerging roles of Lipasin as a critical lipid regulator. Biochem Biophys Res Commun. 2013. https://doi.org/10.1016/j.bbrc.2013.01.129.
Nisoli E, Tonello C, Benarese M, Liberini P, Carruba MJE. Expression of nerve growth factor in brown adipose tissue: implications for thermogenesis and obesity. Endocrinology. 1996. https://doi.org/10.1210/en.137.2.495.
Baudier J, Gentil BJ. The S100B protein and partners in adipocyte response to cold stress and adaptive thermogenesis: Facts, hypotheses, and perspectives. Biomolecules. 2020. https://doi.org/10.3390/biom10060843.
Wang G-X, et al. The brown fat–enriched secreted factor Nrg4 preserves metabolic homeostasis through attenuation of hepatic lipogenesis. Nat Med. 2014. https://doi.org/10.1038/nm.3713.
Pfeifer A. NRG4: an endocrine link between brown adipose tissue and liver. Cell Metabol. 2015. https://doi.org/10.1016/j.cmet.2014.12.008.
Wang G-X, Zhao X-Y, Lin JD. The brown fat secretome: metabolic functions beyond thermogenesis. Trends Endocrinol Metab. 2015. https://doi.org/10.1016/j.tem.2015.03.002.
Rosell M, et al. Brown and white adipose tissues: intrinsic differences in gene expression and response to cold exposure in mice. Am J Physiol Endocrinol Metab. 2014. https://doi.org/10.1152/ajpendo.00473.2013.
Mauer J, et al. Signaling by IL-6 promotes alternative activation of macrophages to limit endotoxemia and obesity-associated resistance to insulin. Nat Immunol. 2014. https://doi.org/10.1038/ni.2865.
Pal M, Febbraio MA, Whitham M. From cytokine to myokine: the emerging role of interleukin-6 in metabolic regulation. Immunol Cell Biol. 2014. https://doi.org/10.1038/icb.2014.16.
Kristóf E, et al. Interleukin-6 released from differentiating human beige adipocytes improves browning. Exp Cell Res. 2019. https://doi.org/10.1016/j.yexcr.2019.02.015.
Stanford KI, et al. Brown adipose tissue regulates glucose homeostasis and insulin sensitivity. J Clin Invest. 2013. https://doi.org/10.1172/JCI62308.
Hui X, et al. Adiponectin enhances cold-induced browning of subcutaneous adipose tissue via promoting M2 macrophage proliferation. Cell Metab. 2015. https://doi.org/10.1016/j.cmet.2015.06.004.
Kubota N, et al. Adiponectin stimulates AMP-activated protein kinase in the hypothalamus and increases food intake. Cell Metab. 2007. https://doi.org/10.1016/j.cmet.2007.06.003.
Rao RR, et al. Meteorin-like is a hormone that regulates immune-adipose interactions to increase beige fat thermogenesis. Cell. 2014. https://doi.org/10.1016/j.cell.2014.03.065.
Rahman S, Lu Y, Czernik PJ, Rosen CJ, Enerback S, Lecka-Czernik B. Inducible brown adipose tissue, or beige fat, is anabolic for the skeleton. Endocrinology. 2013. https://doi.org/10.1210/en.2012-2162.
Wright WS, et al. Wnt10b inhibits obesity in ob/ob and agouti mice. Diabetes. 2007. https://doi.org/10.2337/db06-1339.
Bianco AC, McAninch EA. The role of thyroid hormone and brown adipose tissue in energy homoeostasis. Lancet Diabetes Endocrinol. 2013. https://doi.org/10.1016/S2213-8587(13)70069-X.
Ruan C-C, et al. A2A receptor activation attenuates hypertensive cardiac remodeling via promoting brown adipose tissue-derived FGF21. Cell Metab. 2018. https://doi.org/10.1016/j.cmet.2018.06.013.
Cereijo R, et al. CXCL14, a brown adipokine that mediates brown-fat-to-macrophage communication in thermogenic adaptation. Cell Metab. 2018. https://doi.org/10.1016/j.cmet.2018.07.015.
Boughanem H, Yubero-Serrano EM, López-Miranda J, Tinahones FJ, Macias-Gonzalez M. Potential role of insulin growth-factor-binding protein 2 as therapeutic target for obesity-related insulin resistance. Int J Mol Sci. 2021. https://doi.org/10.3390/ijms22031133.
Xi G, Wai C, DeMambro V, Rosen CJ, Clemmons DR. IGFBP-2 directly stimulates osteoblast differentiation. J Bone Miner Res. 2014. https://doi.org/10.1002/jbmr.2282.
Kawai M, et al. The heparin-binding domain of IGFBP-2 has insulin-like growth factor binding-independent biologic activity in the growing skeleton. Cell Biol. 2011. https://doi.org/10.1074/jbc.M110.193334.
Campderrós L, et al. Brown adipocytes secrete GDF15 in response to thermogenic activation. Obesity (Silver Spring). 2019. https://doi.org/10.1002/oby.22584.
Breit SN, Tsai VW-W, Brown DA. Targeting obesity and cachexia: identification of the GFRAL receptor–MIC-1/GDF15 pathway. Trends Mol Med. 2017. https://doi.org/10.1016/j.molmed.2017.10.005.
Tsai VW, Husaini Y, Sainsbury A, Brown DA, Breit SN. The MIC-1/GDF15-GFRAL pathway in energy homeostasis: implications for obesity, cachexia, and other associated diseases. Cell Metab. 2018. https://doi.org/10.1016/j.cmet.2018.07.018.
Deshmukh AS, et al. Proteomics-based comparative mapping of the secretomes of human brown and white adipocytes reveals EPDR1 as a novel batokine. Cell Metab. 2019. https://doi.org/10.1016/j.cmet.2019.10.001.
Rosell M, et al. Peroxisome proliferator-activated receptors-α and-γ, and cAMP-mediated pathways, control retinol-binding protein-4 gene expression in brown adipose tissue. Endocrinology. 2012. https://doi.org/10.1210/en.2011-1367.
Kiefer FW, et al. Retinaldehyde dehydrogenase 1 coordinates hepatic gluconeogenesis and lipid metabolism. Endocrinology. 2012. https://doi.org/10.1210/en.2011-2104.
Nankam PAN, Blüher M. Retinol-binding protein 4 in obesity and metabolic dysfunctions. Mol Cell Endocrinol. 2021. https://doi.org/10.1016/j.mce.2021.111312.
Gavaldà-Navarro A, Villarroya J, Cereijo R, Giralt M, Villarroya F. The endocrine role of brown adipose tissue: An update on actors and actions. Rev Endocr Metab Disord. 2021. https://doi.org/10.1007/s11154-021-09640-6.
Sponton CH, et al. The regulation of glucose and lipid homeostasis via PLTP as a mediator of BAT–liver communication. EMBO Rep. 2020. https://doi.org/10.15252/embr.201949828.
Thomou T, et al. Adipose-derived circulating miRNAs regulate gene expression in other tissues. Nature. 2017. https://doi.org/10.1038/nature21365.
Chen Y, et al. Exosomal microRNA miR-92a concentration in serum reflects human brown fat activity. Nat Commun. 2016. https://doi.org/10.1038/ncomms11420.
Chen Y, Pan R, Pfeifer A. Regulation of brown and beige fat by microRNAs. Pharmacol Ther. 2017. https://doi.org/10.1016/j.pharmthera.2016.10.004.
Kariba Y, Yoshizawa T, Sato Y, Tsuyama T, Araki E, Yamagata K. Brown adipocyte-derived exosomal miR-132-3p suppress hepatic Srebf1 expression and thereby attenuate expression of lipogenic genes. Biochem Biophys Res Commun. 2020. https://doi.org/10.1016/j.bbrc.2020.05.090.
Verdeguer F, et al. Brown adipose YY1 deficiency activates expression of secreted proteins linked to energy expenditure and prevents diet-induced obesity. Mol Cell Biol. 2015. https://doi.org/10.1128/MCB.00722-15.
Cikes D, et al. Neuropeptide Neuromedin B does not alter body weight and glucose homeostasis nor does it act as an insulin-releasing peptide. Sci Rep. 2022. https://doi.org/10.1038/s41598-022-13060-0.
de Paula GSM, et al. Neuromedin B receptor disruption impairs adipogenesis in mice and 3T3-L1 cells. J Mol Endocrinol. 2019. https://doi.org/10.1530/JME-19-0032.
Ramanjaneya M, et al. Identification of nesfatin-1 in human and murine adipose tissue: a novel depot-specific adipokine with increased levels in obesity. Endocrinology. 2010. https://doi.org/10.1210/en.2009-1358.
Wang Y, et al. Nesfatin-1 promotes brown adipocyte phenotype. Sci Rep. 2016. https://doi.org/10.1038/srep34747.
Levata L, Dore R, Jöhren O, Schwaninger M, Schulz C, Lehnert H. Nesfatin-1 acts centrally to induce sympathetic activation of brown adipose tissue and non-shivering thermogenesis. Horm Metab Res. 2019. https://doi.org/10.1055/a-0985-4272.
Valencia-Ortega J, et al. New insights into adipokines in gestational diabetes mellitus. Int J Mol Sci. 2022. https://doi.org/10.3390/ijms23116279.
Radzicka-Mularczyk S, Zaborowski MP, Brązert J, Pietryga M. Serum visfatin as a metabolic biomarker in obese patients with gestational diabetes mellitus. Minerva Endocrinol. 2021. https://doi.org/10.23736/s2724-6507.20.03280-0.
Icli B, Feinberg MW. MicroRNAs in dysfunctional adipose tissue: cardiovascular implications. Cardiovasc Res. 2017. https://doi.org/10.1093/cvr/cvx098.
Arias N, et al. MicroRNAs involved in the browning process of adipocytes. J Physiol Biochem. 2016. https://doi.org/10.1007/s13105-015-0459-z.
Gharanei S, et al. Regulatory microRNAs in Brown. Brite and White Adipose Tissue Cells. 2020. https://doi.org/10.3390/cells9112489.
Goody D, Pfeifer A. MicroRNAs in brown and beige fat. Biochim Biophys Acta Mol Cell Biol Lipids. 2019. https://doi.org/10.1016/j.bbalip.2018.05.003.
Shamsi F, Zhang H, Tseng YH. MicroRNA Regulation of Brown Adipogenesis and Thermogenic Energy Expenditure. Front Endocrinol (Lausanne). 2017. https://doi.org/10.3389/fendo.2017.00205.
Choe SS, Huh JY, Hwang IJ, Kim JI, Kim JB. Adipose tissue remodeling: its role in energy metabolism and metabolic disorders. Front Endocrinol (Lausanne). 2016. https://doi.org/10.3389/fendo.2016.00030.
Zaragosi L-E, et al. Small RNA sequencing reveals miR-642a-3p as a novel adipocyte-specific microRNA and miR-30 as a key regulator of human adipogenesis. Genome Biol. 2011. https://doi.org/10.1186/gb-2011-12-7-r64.
Ling HY, et al. MicroRNA-375 promotes 3T3-L1 adipocyte differentiation through modulation of extracellular signal-regulated kinase signalling. Clin Exp Pharmacol Physiol. 2011. https://doi.org/10.1111/j.1440-1681.2011.05493.x.
Kang M, Yan L-M, Zhang W-Y, Li Y-M, Tang A-Z, Ou H-SJMBR. Role of microRNA-21 in regulating 3T3-L1 adipocyte differentiation and adiponectin expression. Mol Biol Rep. 2013. https://doi.org/10.1007/s11033-013-2603-6.
Song G, et al. The role of microRNA-26b in human adipocyte differentiation and proliferation. Gene. 2014. https://doi.org/10.1016/j.gene.2013.10.011.
Shi C, et al. miR-148a is associated with obesity and modulates adipocyte differentiation of mesenchymal stem cells through Wnt signaling. Sci Rep. 2015. https://doi.org/10.1038/srep09930.
Xie H, Lim B, Lodish HF. MicroRNAs induced during adipogenesis that accelerate fat cell development are downregulated in obesity. Diabetes. 2009. https://doi.org/10.2337/db08-1299.
Shi C, et al. Adipogenic miRNA and meta-signature miRNAs involved in human adipocyte differentiation and obesity. Oncotarget. 2016. https://doi.org/10.18632/oncotarget.8518.
Price NL, Fernández-Hernando C. miRNA regulation of white and brown adipose tissue differentiation and function. Biochim Biophys Acta. 2016. https://doi.org/10.1016/j.bbalip.2016.02.010.
Youssef EM, Elfiky AM, Abu-Shahba N, Elhefnawi MM. Expression profiling and analysis of some miRNAs in subcutaneous white adipose tissue during development of obesity. Genes Nutr. 2020. https://doi.org/10.1186/s12263-020-00666-0.
Sun L, et al. Mir193b–365 is essential for brown fat differentiation. Nat Cell Biol. 2011. https://doi.org/10.1038/ncb2286.
Dong M, Ye Y, Chen Z, Xiao T, Liu W, Hu F. MicroRNA 182 is a novel negative regulator of adipogenesis by targeting CCAAT/enhancer-binding protein α. Obesity. 2020. https://doi.org/10.1002/oby.22863.
Ma C, et al. miR-182 targeting reprograms tumor-associated macrophages and limits breast cancer progression. Proc Natl Acad Sci. 2022. https://doi.org/10.1073/pnas.2114006119.
Guo X, et al. cAMP-MicroRNA-203-IFNγ network regulates subcutaneous white fat browning and glucose tolerance. Mol Metab. 2019. https://doi.org/10.1016/j.molmet.2019.07.002.
Kim H-J, et al. MicroRNAs are required for the feature maintenance and differentiation of brown adipocytes. Diabetes. 2014. https://doi.org/10.2337/db14-0466.
Wu Y, et al. Identification of miR-106b-93 as a negative regulator of brown adipocyte differentiation. Biochem Biophys Res Commun. 2013. https://doi.org/10.1016/j.bbrc.2013.08.016.
Oliverio M, et al. Dicer1-miR-328-Bace1 signalling controls brown adipose tissue differentiation and function. Nat Cell Biol. 2016. https://doi.org/10.1038/ncb3316.
Fu X, et al. miR-129-5p inhibits adipogenesis through autophagy and may be a potential biomarker for obesity. Int J Endocrinol. 2019. https://doi.org/10.1155/2019/5069578.
Zhang H, et al. Micro RNA-455 regulates brown adipogenesis via a novel HIF 1an-AMPK-PGC 1α signaling network. EMBO Rep. 2015;1:1. https://doi.org/10.15252/embr.201540837.
Cai Z, Liu J, Bian H, Cai J, Guo X. MiR-455 enhances adipogenic differentiation of 3T3-L1 cells through targeting uncoupling protein-1. Life-Sci Lit. 2016. https://doi.org/10.1691/ph.2016.6734.
Pahlavani M, et al. Transcriptomic and microRNA analyses of gene networks regulated by eicosapentaenoic acid in brown adipose tissue of diet-induced obese mice. Biochim Biophys Acta Mol Cell Biol Lipids. 2018. https://doi.org/10.1016/j.bbalip.2018.09.004.
Hu F, et al. miR-30 promotes thermogenesis and the development of beige fat by targeting RIP140. Diabetes. 2015. https://doi.org/10.2337/db14-1117.
Ge X, Sathiakumar D, Lua B, Kukreti H, Lee M, McFarlane C. Myostatin signals through miR-34a to regulate Fndc5 expression and browning of white adipocytes. Int J Obes. 2017. https://doi.org/10.1038/ijo.2016.110.
Pan Y, et al. Adipocyte-secreted exosomal microRNA-34a inhibits M2 macrophage polarization to promote obesity-induced adipose inflammation. J Clin Invest. 2019. https://doi.org/10.1172/JCI123069.
Sun L, Trajkovski M. MiR-27 orchestrates the transcriptional regulation of brown adipogenesis. Metabolism. 2014. https://doi.org/10.1016/j.metabol.2013.10.004.
Kang T, et al. MicroRNA-27 (miR-27) targets prohibitin and impairs adipocyte differentiation and mitochondrial function in human adipose-derived stem cells. J Biol Chem. 2013. https://doi.org/10.1074/jbc.M113.514372.
Kim J, Okla M, Erickson A, Carr T, Natarajan SK, Chung S. Eicosapentaenoic acid potentiates brown thermogenesis through FFAR4-dependent up-regulation of miR-30b and miR-378. J Biol Metabol. 2016. https://doi.org/10.1074/jbc.M116.721480.
Yin H, et al. MicroRNA-133 controls brown adipose determination in skeletal muscle satellite cells by targeting Prdm16. Cell Metab. 2013. https://doi.org/10.1016/j.cmet.2013.01.004.
Chen Y, et al. miR-155 regulates differentiation of brown and beige adipocytes via a bistable circuit. Nat Commun. 2013. https://doi.org/10.1038/ncomms2742.
Zhang Y, Mei H, Chang X, Chen F, Zhu Y, Han X. Adipocyte-derived microvesicles from obese mice induce M1 macrophage phenotype through secreted miR-155. J Mol Cell Biol. 2016. https://doi.org/10.1093/jmcb/mjw040.
Ying W, et al. Adipose tissue macrophage-derived exosomal miRNAs can modulate in vivo and in vitro insulin sensitivity. Cell. 2017. https://doi.org/10.1016/j.cell.2017.08.035.
Mattiske S, Suetani RJ, Neilsen PM, Callen DF. The oncogenic role of miR-155 in breast cancer. Cancer Epidemiol Miomark Prev. 2012. https://doi.org/10.1158/1055-9965.EPI-12-0173.
Ng R, et al. miRNA-32 drives brown fat thermogenesis and trans-activates subcutaneous white fat browning in mice. Cell Rep. 2017. https://doi.org/10.1016/j.celrep.2017.04.035.
Mori M, Nakagami H, Rodriguez-Araujo G, Nimura K, Kaneda Y. Essential role for miR-196a in brown adipogenesis of white fat progenitor cells. PLoS Biol. 2012. https://doi.org/10.1371/journal.pbio.1001314.
Hilton C, et al. MicroRNA-196a links human body fat distribution to adipose tissue extracellular matrix composition. EBioMedicine. 2019. https://doi.org/10.1016/j.ebiom.2019.05.047.
Karbiener M, et al. MicroRNA-26 family is required for human adipogenesis and drives characteristics of brown adipocytes. Stem Cell. 2014. https://doi.org/10.1002/stem.1603.
Rockstroh D, Löffler D, Kiess W, Landgraf K, Körner A. Regulation of human adipogenesis by miR125b-5p. Adipocyte. 2016. https://doi.org/10.1080/21623945.2016.1195044.
Giroud M, et al. miR-125b affects mitochondrial biogenesis and impairs brite adipocyte formation and function. Mol Metab. 2016. https://doi.org/10.1016/j.molmet.2016.06.005.
Giroud M, et al. Let-7i-5p represses brite adipocyte function in mice and humans. Sci Rep. 2016. https://doi.org/10.1038/srep28613.
Koh EH, et al. miR-30a remodels subcutaneous adipose tissue inflammation to improve insulin sensitivity in obesity. Diabetes. 2018. https://doi.org/10.2337/db17-1378.
Chen L, et al. MicroRNA-143 regulates Adipogenesis by modulating the MAP2K5–ERK5 signaling. Sci Rep. 2014. https://doi.org/10.1038/srep03819.
Xihua L, et al. Circulating miR-143-3p inhibition protects against insulin resistance in Metabolic Syndrome via targeting of the insulin-like growth factor 2 receptor. Transl Res. 2019. https://doi.org/10.1016/j.trsl.2018.09.006.
Zhang C, et al. MiR17 improves insulin sensitivity through inhibiting expression of ASK1 and anti-inflammation of macrophages. Biomed Pharmacother. 2018. https://doi.org/10.1016/j.biopha.2018.02.012.
Li H, et al. MiRNA-181a regulates adipogenesis by targeting tumor necrosis factor-α (TNF-α) in the porcine model. PLoS ONE. 2013. https://doi.org/10.1371/journal.pone.0071568.
Virtue AT, et al. The gut microbiota regulates white adipose tissue inflammation and obesity via a family of microRNAs. Sci Transl Med. 2019. https://doi.org/10.1126/scitranslmed.aav1892.
Ahonen MA, et al. miR-107 inhibits CDK6 expression, differentiation, and lipid storage in human adipocytes. Mol Cell Endocrinol. 2019. https://doi.org/10.1016/j.mce.2018.09.007.
Zhang Z, Wu S, Muhammad S, Ren Q, Sun C. miR-103/107 promote ER stress-mediated apoptosis via targeting the Wnt3a/β-catenin/ATF6 pathway in preadipocytes. J Lipid Res. 2018. https://doi.org/10.1194/jlr.M082602.
Li M, Liu Z, Zhang Z, Liu G, Sun S, Sun C. miR-103 promotes 3T3-L1 cell adipogenesis through AKT/mTOR signal pathway with its target being MEF2D. De Gruyter. 2015. https://doi.org/10.1515/hsz-2014-0241.
Frias FDT, et al. Fenofibrate reverses changes induced by high-fat diet on metabolism in mice muscle and visceral adipocytes. J Cell Physiol. 2018. https://doi.org/10.1002/jcp.26203.
Kim SY, et al. miR-27a is a negative regulator of adipocyte differentiation via suppressing PPARγ expression. Biochem Biophys Res Commun. 2010. https://doi.org/10.1016/j.bbrc.2010.01.012.
Yu Y, et al. Adipocyte-derived exosomal MiR-27a induces insulin resistance in skeletal muscle through repression of PPARγ. Theranostics. 2018. https://doi.org/10.7150/thno.22565.
Zhang M, Sun W, Zhou M, Tang Y. MicroRNA-27a regulates hepatic lipid metabolism and alleviates NAFLD via repressing FAS and SCD1. Sci Rep. 2017. https://doi.org/10.1038/s41598-017-15141-x.
Kim C, Lee H, Cho YM, Kwon O-J, Kim W, Lee EK. TNFα-induced miR-130 resulted in adipocyte dysfunction during obesity-related inflammation. FEBS Lett. 2013. https://doi.org/10.1016/j.febslet.2013.10.018.
Yiew NK, et al. A novel role for the Wnt inhibitor APCDD1 in adipocyte differentiation: Implications for diet-induced obesity. J Biol Chem. 2017. https://doi.org/10.1074/jbc.M116.758078.
Rayner KJ, et al. MiR-33 contributes to the regulation of cholesterol homeostasis. Science. 2010. https://doi.org/10.1126/science.1189862.
Price NL, et al. SREBP-1c/MicroRNA 33b genomic loci control adipocyte differentiation. Mol Cell Biol. 2016. https://doi.org/10.1128/MCB.00745-15.
Bork S, Horn P, Castoldi M, Hellwig I, Ho AD, Wagner W. Adipogenic differentiation of human mesenchymal stromal cells is down-regulated by microRNA-369-5p and up-regulated by microRNA-371. Cell Phsiol. 2011. https://doi.org/10.1002/jcp.22557.
Meerson A, Traurig M, Ossowski V, Fleming J, Mullins M, Baier L. Human adipose microRNA-221 is upregulated in obesity and affects fat metabolism downstream of leptin and TNF-α. Diabetologia. 2013. https://doi.org/10.1007/s00125-013-2950-9.
Ahonen MA, et al. Human adipocyte differentiation and composition of disease-relevant lipids are regulated by miR-221-3p. Biochim Biophys Acta Mol Cell Biol Lipids. 2021. https://doi.org/10.1016/j.bbalip.2020.158841.
Peng J, et al. miR-221 negatively regulates inflammation and insulin sensitivity in white adipose tissue by repression of sirtuin-1 (SIRT1). J Cell Biochem. 2018. https://doi.org/10.1002/jcb.26589.
Kim YJ, Hwang SJ, Bae YC, Jung JS. MiR-21 regulates adipogenic differentiation through the modulation of TGF-β signaling in mesenchymal stem cells derived from human adipose tissue. Stem Cell. 2009. https://doi.org/10.1002/stem.235.
He H, et al. miR-148a-3p promotes rabbit preadipocyte differentiation by targeting PTEN. In Vitro Cell Dev Biol Anim. 2018. https://doi.org/10.1007/s11626-018-0232-z.
Tian F, et al. miR-210 in exosomes derived from macrophages under high glucose promotes mouse diabetic obesity pathogenesis by suppressing NDUFA4 expression. J Diabetes Res. 2020. https://doi.org/10.1155/2020/6894684.
Bargut TCL, Souza-Mello V, Aguila MB, Mandarim-de-Lacerda CA. Browning of white adipose tissue: lessons from experimental models. Horm Mol Biol Clin Investig. 2017. https://doi.org/10.1515/hmbci-2016-0051.
Wu J, Cohen P, Spiegelman BM. Adaptive thermogenesis in adipocytes: is beige the new brown? Genes Dev. 2013. https://doi.org/10.1101/gad.211649.112.
Tan CY, Ishikawa K, Virtue S, Vidal-Puig A. Brown adipose tissue in the treatment of obesity and diabetes: Are we hot enough? J Diabetes Investig. 2011. https://doi.org/10.1111/j.2040-1124.2011.00158.x.
Zhang W, Sheng T, Gu Z, Zhang Y. Strategies for browning agent delivery. Pharm Res. 2021. https://doi.org/10.1007/s11095-021-03081-1.
Zu Y, et al. Browning white adipose tissue using adipose stromal cell-targeted resveratrol-loaded nanoparticles for combating obesity. J Control Release. 2021. https://doi.org/10.1016/j.jconrel.2021.03.022.
Xue Y, Xu X, Zhang X-Q, Farokhzad OC, Langer R. Preventing diet-induced obesity in mice by adipose tissue transformation and angiogenesis using targeted nanoparticles. Proc Natl Acad Sci U S A. 2016. https://doi.org/10.1073/pnas.1603840113.
Zhang Y, Yu J, Qiang L, Gu Z. Nanomedicine for obesity treatment. Sci China Life Sci. 2018. https://doi.org/10.1007/s11427-017-9257-1.
Roth CL, Molica F, Kwak BR. Browning of white adipose tissue as a therapeutic tool in the fight against atherosclerosis. Metabolites. 2021. https://doi.org/10.3390/metabo11050319.
Bartelt A, et al. Thermogenic adipocytes promote HDL turnover and reverse cholesterol transport. Nat Commun. 2017. https://doi.org/10.1038/ncomms15010.
Noori M, Darabi M, Rahimipour A, Rahbani M, Abadi NA, Ghatrehsamani K. Fatty acid composition of HDL phospholipids and coronary artery disease. J Clin Lipidol. 2009. https://doi.org/10.1016/j.jacl.2008.11.010.
Shi L, et al. Brown adipose tissue-derived Nrg4 alleviates endothelial inflammation and atherosclerosis in male mice. Nat Metab. 2022. https://doi.org/10.1038/s42255-022-00671-0.
Young P, Arch J, Ashwell M. Brown adipose tissue in the parametrial fat pad of the mouse. FEBS Lett. 1984. https://doi.org/10.1016/0014-5793(84)80822-4.
Cousin B, et al. Occurrence of brown adipocytes in rat white adipose tissue: molecular and morphological characterization. J Cell Sci. 1992. https://doi.org/10.1242/jcs.103.4.931.
Wang X, Wahl R. Responses of the insulin signaling pathways in the brown adipose tissue of rats following cold exposure. PLoS One. 2014. https://doi.org/10.1371/journal.pone.0099772.
Ghorbani M, Himms-Hagen J. Appearance of brown adipocytes in white adipose tissue during CL 316,243-induced reversal of obesity and diabetes in Zucker fa/fa rats. Int J Obes Relat Metab Disord. 1997. https://doi.org/10.1038/sj.ijo.0800432.
Lin HV, et al. Butyrate and propionate protect against diet-induced obesity and regulate gut hormones via free fatty acid receptor 3-independent mechanisms. PLoS ONE. 2012. https://doi.org/10.1371/journal.pone.0035240.
Sahuri-Arisoylu M, et al. Reprogramming of hepatic fat accumulation and’browning’of adipose tissue by the short-chain fatty acid acetate. Int J Obes. 2016. https://doi.org/10.1038/ijo.2016.23.
Baskaran P, Krishnan V, Ren J, Thyagarajan B. Capsaicin induces browning of white adipose tissue and counters obesity by activating TRPV1 channel-dependent mechanisms. Br J Pharmacol. 2016. https://doi.org/10.1111/bph.13514.
Wang S, et al. Resveratrol enhances brown adipocyte formation and function by activating AMP-activated protein kinase (AMPK) α1 in mice fed high-fat diet. Mol Nutr Food Res. 2017. https://doi.org/10.1002/mnfr.201600746.
Liu Z, et al. Resveratrol-induced brown fat-like phenotype in 3T3-L1 adipocytes partly via mTOR pathway. Food Nutr Res. 2020. https://doi.org/10.29219/fnr.v64.3656.
Zhang Z, et al. Berberine activates thermogenesis in white and brown adipose tissue. Nat Commun. 2014. https://doi.org/10.1038/ncomms6493.
Xu Y, et al. Berberine modulates deacetylation of PPARγ to promote adipose tissue remodeling and thermogenesis via AMPK/SIRT1 pathway. Int J Biol Sci. 2021. https://doi.org/10.7150/ijbs.62556.
Kim M, et al. Fish oil intake induces UCP1 upregulation in brown and white adipose tissue via the sympathetic nervous system. Sci Rep. 2015. https://doi.org/10.1038/srep18013.
Chen L-H, et al. Green tea extract induces genes related to browning of white adipose tissue and limits weight-gain in high energy diet-fed rat. Food Nutr Res. 2017. https://doi.org/10.1080/16546628.2017.1347480.
Neyrinck AM, Bindels LB, Geurts L, Van Hul M, Cani PD, Delzenne NM. A polyphenolic extract from green tea leaves activates fat browning in high-fat-diet-induced obese mice. J Nutr Biochem. 2017. https://doi.org/10.1016/j.jnutbio.2017.07.008.
Kwan HY, et al. Cinnamon induces browning in subcutaneous adipocytes. Sci Rep. 2017. https://doi.org/10.1038/s41598-017-02263-5.
Lee SG, Parks JS, Kang HW. Quercetin, a functional compound of onion peel, remodels white adipocytes to brown-like adipocytes. J Nutr Biochem. 2017. https://doi.org/10.1016/j.jnutbio.2016.12.018.
Kuipers EN, et al. Quercetin lowers plasma triglycerides accompanied by white adipose tissue browning in diet-induced obese mice. Int J Mol Sci. 2018. https://doi.org/10.3390/ijms19061786.
Zhao D, et al. Curcumin improves adipocytes browning and mitochondrial function in 3T3-L1 cells and obese rodent model. Royal Society Open Science. 2021. https://doi.org/10.1098/rsos.200974.
Mu Q, et al. Ginsenoside Rb1 promotes browning through regulation of PPARγ in 3T3-L1 adipocytes. Biochem Biophys Res Commun. 2015. https://doi.org/10.1016/j.bbrc.2015.09.064.
Fan Q, et al. Ginsenoside Rb1 facilitates browning by repressing Wnt/β-catenin signaling in 3T3-L1 adipocytes. Med Sci Monit Int Med J Exp Clin Res. 2021. https://doi.org/10.12659/MSM.928619.
Fang S, et al. Intestinal FXR agonism promotes adipose tissue browning and reduces obesity and insulin resistance. Nat Med. 2015. https://doi.org/10.1038/nm.3760.
Miao Y, et al. Liver X receptor β controls thyroid hormone feedback in the brain and regulates browning of subcutaneous white adipose tissue. Proc Natl Acad Sci U S A. 2015. https://doi.org/10.1073/pnas.1519358112.
Kroon T, et al. PPARγ and PPARα synergize to induce robust browning of white fat in vivo. Mol Metabol. 2020. https://doi.org/10.1016/j.molmet.2020.02.007.
García-Alonso V, Clària J. Prostaglandin E2 signals white-to-brown adipogenic differentiation. Adipocyte. 2014. https://doi.org/10.4161/adip.29993.
Choi S-S, et al. PPARγ antagonist Gleevec improves insulin sensitivity and promotes the browning of white adipose tissue. Diabetes. 2016. https://doi.org/10.2337/db15-1382.
Choi WH, Ahn J, Jung CH, Jang YJ, Ha TY. β-Lapachone prevents diet-induced obesity by increasing energy expenditure and stimulating the browning of white adipose tissue via downregulation of miR-382 expression. Diabetes. 2016. https://doi.org/10.2337/db15-1423.
Nishikawa S, et al. Artepillin C, a typical Brazilian propolis-derived component, induces brown-like adipocyte formation in C3H10T1/2 cells, primary inguinal white adipose tissue-derived adipocytes, and mice. PLoS ONE. 2016. https://doi.org/10.1371/journal.pone.0162512.
Zhang H, et al. Intermedin/adrenomedullin 2 polypeptide promotes adipose tissue browning and reduces high-fat diet-induced obesity and insulin resistance in mice. Int J Obes (Lond). 2016. https://doi.org/10.1038/ijo.2016.2.
Zhang S-Y, et al. Adrenomedullin 2 improves early obesity-induced adipose insulin resistance by inhibiting the class II MHC in adipocytes. Diabetes. 2016. https://doi.org/10.2337/db15-1626.
Abdullahi A, Chen P, Stanojcic M, Sadri A-R, Coburn N, Jeschke MGJS. IL-6 signal from the bone marrow is required for the browning of white adipose tissue post burn injury. HHS Public Access. 2017. https://doi.org/10.1097/SHK.0000000000000749.
Nguyen KD, et al. Alternatively activated macrophages produce catecholamines to sustain adaptive thermogenesis. Nature. 2011. https://doi.org/10.1038/nature10653.
Shahid M, et al. IEX-1 deficiency induces browning of white adipose tissue and resists diet-induced obesity. Sci Rep. 2016. https://doi.org/10.1038/srep24135.
Johann K, et al. Thyroid-hormone-induced browning of white adipose tissue does not contribute to thermogenesis and glucose consumption. Cell Rep. 2019. https://doi.org/10.1016/j.celrep.2019.05.054.
Weiner J, et al. Thyroid hormone status defines brown adipose tissue activity and browning of white adipose tissues in mice. Sci Rep. 2016. https://doi.org/10.1038/srep38124.
Weiner J, Hankir M, Heiker JT, Fenske W, Krause K. Thyroid hormones and browning of adipose tissue. Mol Cell Endocrinol. 2017. https://doi.org/10.1016/j.mam.2019.06.004.
Thomas SS, Mitch WE. Parathyroid hormone stimulates adipose tissue browning: a pathway to muscle wasting. Curr Opin Clin Nutr Metab Care. 2017. https://doi.org/10.1097/MCO.0000000000000357.
Beiroa D, et al. GLP-1 agonism stimulates brown adipose tissue thermogenesis and browning through hypothalamic AMPK. Diabetes. 2014. https://doi.org/10.2337/db14-0302.
López M, Diéguez C, Nogueiras R. Hypothalamic GLP-1: the control of BAT thermogenesis and browning of white fat. Adipocyte. 2015. https://doi.org/10.4161/21623945.2014.983752.
Dodd GT, et al. Leptin and insulin act on POMC neurons to promote the browning of white fat. Cell. 2015. https://doi.org/10.1016/j.cell.2014.12.022.
Jiménez-Aranda A, et al. Melatonin induces browning of inguinal white adipose tissue in Zucker diabetic fatty rats. J Pineal Res. 2013. https://doi.org/10.1111/jpi.12089.
Salagre D, et al. Melatonin induces fat browning by transdifferentiation of white adipocytes and de novo differentiation of mesenchymal stem cells. Food Funct. 2022. https://doi.org/10.1039/D1FO04360A.
Bordicchia M, et al. Cardiac natriuretic peptides act via p38 MAPK to induce the brown fat thermogenic program in mouse and human adipocytes. J Clin Invest. 2012. https://doi.org/10.1172/JCI59701.
Liu D, Ceddia RP, Collins S. Cardiac natriuretic peptides promote adipose ‘browning’through mTOR complex-1. Mol Metabol. 2018. https://doi.org/10.1016/j.molmet.2017.12.017.
Zhang Y, et al. Irisin stimulates browning of white adipocytes through mitogen-activated protein kinase p38 MAP kinase and ERK MAP kinase signaling. Diabetes. 2014. https://doi.org/10.2337/db13-1106.
Chen Y, Ding J, Zhao Y, Ju S, Mao H, Peng X-G. Irisin induces white adipose tissue browning in mice as assessed by magnetic resonance imaging. Exp Biol Med. 2021. https://doi.org/10.1177/15353702211006049.
Frühbeck G, et al. FNDC4, a novel adipokine that reduces lipogenesis and promotes fat browning in human visceral adipocytes. Metabolism. 2020. https://doi.org/10.1016/j.metabol.2020.154261.
Xue L, et al. Maternal secretin ameliorates obesity by promoting white adipose tissue browning in offspring. EMBO Rep. 2022. https://doi.org/10.15252/embr.202154132.
Yadav H, Rane SG. TGF-β/Smad3 signaling regulates brown adipocyte induction in white adipose tissue. Front Endocrinol (Lausanne). 2012. https://doi.org/10.3389/fendo.2012.00035.
Kleiner S, et al. FGF21 regulates PGC-1α and browning of white adipose tissues in adaptive thermogenesis. Genes Dev. 2012. https://doi.org/10.1101/gad.177857.111.
Cuevas-Ramos D, Mehta R, Aguilar-Salinas CA. Fibroblast growth factor 21 and browning of white adipose tissue. Front Physiol. 2019. https://doi.org/10.3389/fphys.2019.00037.
Virtue S, et al. A new role for lipocalin prostaglandin d synthase in the regulation of brown adipose tissue substrate utilization. Diabetes. 2012. https://doi.org/10.2337/db12-0015.
Than A, et al. Apelin enhances brown adipogenesis and browning of white adipocytes. J Biol Chem. 2015. https://doi.org/10.1074/jbc.M115.643817.
Zhang Y, Yu M, Dong J, Wu Y, Tian W. Nucleophosmin3 carried by small extracellular vesicles contribute to white adipose tissue browning. J Nanobiotechnol. 2022. https://doi.org/10.1186/s12951-022-01381-1.
Tanimura R, Kobayashi L, Shirai T, Takemasa T. Effects of exercise intensity on white adipose tissue browning and its regulatory signals in mice. Physiol Rep. 2022. https://doi.org/10.14814/phy2.15205.
Ohno H, Shinoda K, Spiegelman BM, Kajimura S. PPARγ agonists induce a white-to-brown fat conversion through stabilization of PRDM16 protein. Cell Metab. 2012. https://doi.org/10.1016/j.cmet.2012.01.019.
Fayyad AM, Khan AA, Abdallah SH, Alomran SS, Bajou K, Khattak MNK. Rosiglitazone enhances browning adipocytes in association with MAPK and PI3-K pathways during the differentiation of telomerase-transformed mesenchymal stromal cells into adipocytes. Int J Mol Sci. 2019. https://doi.org/10.3390/ijms20071618.
Hiradate R, Khalil IA, Matsuda A, Sasaki M, Hida K, Harashima H. A novel dual-targeted rosiglitazone-loaded nanoparticle for the prevention of diet-induced obesity via the browning of white adipose tissue. J Control Release. 2021. https://doi.org/10.1016/j.jconrel.2020.10.002.
Zhao S, et al. α/β-Hydrolase domain 6 deletion induces adipose browning and prevents obesity and type 2 diabetes. Cell Rep. 2016. https://doi.org/10.1016/j.celrep.2016.02.076.
Carrière A, et al. Browning of white adipose cells by intermediate metabolites: an adaptive mechanism to alleviate redox pressure. Diabetes. 2014. https://doi.org/10.2337/db13-1885.
Roberts LD, et al. β-Aminoisobutyric acid induces browning of white fat and hepatic β-oxidation and is inversely correlated with cardiometabolic risk factors. Cell Metab. 2014. https://doi.org/10.1016/j.cmet.2013.12.003.
Wang B, et al. Retinoic acid induces white adipose tissue browning by increasing adipose vascularity and inducing beige adipogenesis of PDGFRα+ adipose progenitors. Cell Discov. 2017. https://doi.org/10.1038/celldisc.2017.36.
Moreno-Navarrete JM, Fernandez-Real JM. The gut microbiota modulates both browning of white adipose tissue and the activity of brown adipose tissue. Rev Endocr Metab Disord. 2019. https://doi.org/10.1007/s11154-019-09523-x.
Wu D, Wang H, Xie L, Hu F. Cross-talk between gut microbiota and adipose tissues in obesity and related metabolic diseases. Front Endocrinol. 2022. https://doi.org/10.3389/fendo.2022.908868.
Eljalby M, et al. Brown adipose tissue is not associated with cachexia or increased mortality in a retrospective study of patients with cancer. Am J Physiol-Endocrinol Metabol. 2023. https://doi.org/10.1152/ajpendo.00187.2022.
Liu Y, et al. Exosomal miR-155 from gastric cancer induces cancer-associated cachexia by suppressing adipogenesis and promoting brown adipose differentiation via C/EPBβ. Cancer Biol Med. 2022. https://doi.org/10.20892/j.issn.2095-3941.2021.0220.
Seki T, et al. Brown-fat-mediated tumour suppression by cold-altered global metabolism. Nature. 2022. https://doi.org/10.1038/s41586-022-05030-3.
Chen Z, Kang Y. Cold snap for cancer: cold-induced brown fat thermogenesis starves tumor growth. Signal Transduct Target Ther. 2023. https://doi.org/10.1038/s41392-022-01284-5.
Cao Q, et al. A pilot study of FDG PET/CT detects a link between brown adipose tissue and breast cancer. BMC Cancer. 2014. https://doi.org/10.1186/1471-2407-14-126.
Ginzac A, et al. A decrease in brown adipose tissue activity is associated with weight gain during chemotherapy in early breast cancer patients. BMC Cancer. 2020. https://doi.org/10.1186/s12885-020-6591-3.
Beijer E, et al. A role of active brown adipose tissue in cancer cachexia? Oncol Rev. 2012. https://doi.org/10.4081/oncol.2012.e11.
Norouzi Z, et al. Free fatty acids from type 2 diabetes mellitus serum remodel mesenchymal stem cell lipids, hindering differentiation into primordial germ cells. Appl Biochem Biotechnol. 2022. https://doi.org/10.1007/s12010-022-04204-z.
Fayezi S, Darabi M, Darabi M, Nouri M, Rahimipour A, Mehdizadeh A. Analysis of follicular fluid total phospholipids in women undergoing in-vitro fertilisation. J Obstet Gynaecol. 2014. https://doi.org/10.3109/01443615.2013.851657.
Giedt MS, et al. Adipose triglyceride lipase promotes prostaglandin-dependent actin remodeling by regulating substrate release from lipid droplets. Development. 2023. https://doi.org/10.1242/dev.201516.
Cinti S. Pink adipocytes. Trends Endocrinol Metab. 2018. https://doi.org/10.1016/j.tem.2018.05.007.
Wu M, et al. Adipose tissue and ovarian aging: Potential mechanism and protective strategies. Ageing Res Rev. 2022. https://doi.org/10.1016/j.arr.2022.101683.
Liu H, Liu X, Wang L, Sheng N. Brown adipose tissue transplantation ameliorates male fertility impairment caused by diet-induced obesity. Obes Res Clin Pract. 2017. https://doi.org/10.1016/j.orcp.2016.06.001.
Hu T, et al. Brown adipose tissue activation by rutin ameliorates polycystic ovary syndrome in rat. J Nutr Biochem. 2017. https://doi.org/10.1016/j.jnutbio.2017.04.012.
Ye R, et al. Brown adipose tissue activation by cold treatment ameliorates polycystic ovary syndrome in rat. Front Endocrinol. 2021. https://doi.org/10.3389/fendo.2021.744628.
Chen LJ, et al. Single xenotransplant of rat brown adipose tissue prolonged the ovarian lifespan of aging mice by improving follicle survival. Aging Cell. 2019. https://doi.org/10.1111/acel.13024.
Schermer SJ, Bird JA, Lomax MA, Shepherd D, Symonds ME. Effect of fetal thyroidectomy on brown adipose tissue and thermoregulation in newborn lambs. Reprod Fertil Dev. 1996. https://doi.org/10.1071/RD9960995.
Zheng Y, et al. Irisin reduces the abnormal reproductive and metabolic phenotypes of PCOS by regulating the activity of brown adipose tissue in mice. Biol Reprod. 2022. https://doi.org/10.1093/biolre/ioac125.
Poretsky L, et al. The effects of irisin and leptin on steroidogenic enzyme gene expression in human granulosa cells: In vitro studies. Metabolism Open. 2023. https://doi.org/10.1016/j.metop.2023.100230.
Albrecht U. The circadian clock, metabolism and obesity. Obes Rev. 2017. https://doi.org/10.1111/obr.12502.
Civelek E, Ozturk Civelek D, Akyel YK, Kaleli Durman D, Okyar A. Circadian dysfunction in adipose tissue: chronotherapy in metabolic diseases. Biology. 2023. https://doi.org/10.3390/biology12081077.
Machado SA, et al. Browning of the white adipose tissue regulation: New insights into nutritional and metabolic relevance in health and diseases. Nutr Metab. 2022. https://doi.org/10.1186/s12986-022-00694-0.
Ma D, Qu Y, Wu T, Liu X, Cai L, Wang Y. Circadian rhythm dysregulation aggravates adipose tissue depletion in heart failure-induced cachexia. 2023. https://doi.org/10.21203/rs.3.rs-3139651/v1.
Meng J-J, et al. Light modulates glucose metabolism by a retina-hypothalamus-brown adipose tissue axis. Cell. 2023. https://doi.org/10.1016/j.cell.2022.12.024.
Kooijman S, et al. Prolonged daily light exposure increases body fat mass through attenuation of brown adipose tissue activity. Proc Natl Acad Sci. 2015. https://doi.org/10.1073/pnas.1504239112.
Sarlon J, Partonen T, Lang UE. Potential links between brown adipose tissue, circadian dysregulation, and suicide risk. Front Neurosci. 2023. https://doi.org/10.3389/fnins.2023.1196029.
Ferreira V, Grajales D, Valverde ÁM. Adipose tissue as a target for second-generation (atypical) antipsychotics: A molecular view. Biochim Biophys Acta (BBA)-Mol Cell Biol Lipids. 2020. https://doi.org/10.1016/j.bbalip.2019.158534.
Oh J-E, et al. Inhibition of mouse brown adipocyte differentiation by second-generation antipsychotics. Exp Mol Med. 2012. https://doi.org/10.3858/emm.2012.44.9.062.
Acknowledgements
SF is thankful to the Alexander von Humboldt Foundation.
Funding
Open Access funding enabled and organized by Projekt DEAL. This study was supported by the Tabriz University of Medical Sciences, Tabriz, Iran (Grant No. 66664).
Author information
Authors and Affiliations
Contributions
This study is part of ZG's Ph.D. dissertation supervised by MD, EA, and SF. MD conceived and designed the study, and ZG wrote the first draft of the manuscript. All authors conducted literature searches, contributed to drafting the manuscript, and provided critical feedback. MD and EA specifically provided substantial revisions to the manuscript. All authors have read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was conducted under the ethics code IR.TBZMED.VCR.REC.1400.135 from Tabriz University of Medical Sciences.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ghesmati, Z., Rashid, M., Fayezi, S. et al. An update on the secretory functions of brown, white, and beige adipose tissue: Towards therapeutic applications. Rev Endocr Metab Disord 25, 279–308 (2024). https://doi.org/10.1007/s11154-023-09850-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11154-023-09850-0