Abstract
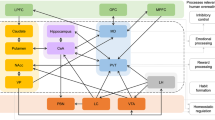
Impulsivity and compulsivity are multidimensional constructs that are increasingly considered determinants of obesity. Studies using functional magnetic resonance imaging (fMRI) have provided insight on how differences in brain response during tasks exploring facets of impulsivity and compulsivity relate to the ingestive behaviors that support the etiology and maintenance of obesity. In this narrative review, we provide an overview of neuroimaging studies exploring impulsivity and compulsivity factors as they relate to weight status. Special focus will be placed on studies examining the impulsivity-related dimensions of attentional bias, delayed gratification and emotion regulation. Discussions of compulsivity within the context of obesity will be restricted to fMRI studies investigating habit formation and response flexibility under shifting contingencies. Further, we will highlight neuroimaging research demonstrating how alterations in neuroendocrine functioning are linked to excessive food intake and may serve as a driver of the impulsive and compulsive behaviors observed in obesity. Research on the associations between brain response with neuroendocrine factors, such as insulin, peptide YY (PYY), leptin, ghrelin and glucagon-like peptide 1 (GLP-1), will be reviewed.

Similar content being viewed by others
References
Field AE, Camargo CA, Ogino S. The merits of subtyping obesity: one size does not fit all. JAMA [Internet]. 2013 Nov 27 [cited 2019 May 22];310(20):2147–8. Available from: http://jama.jamanetwork.com/article.aspx?doi=10.1001/jama.2013.281501
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724.
Wang GJ, Volkow ND, Logan J, Pappas NR, Wong CT, Zhu W, et al. Brain dopamine and obesity. Lancet (London, England) [Internet]. 2001 Feb 3 [cited 2019 May 22];357(9253):354–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11210998. Accessed 22 May 2019.
Burger KS, Berner LA. A functional neuroimaging review of obesity, appetitive hormones and ingestive behavior. Physiol Behav [Internet]. 2014 Sep [cited 2019 May 22];136:121–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24769220. Accessed 22 May 2019.
Bari A, Robbins TW. Inhibition and impulsivity: behavioral and neural basis of response control. Prog Neurobiol. 2013:108, 44–79.
Robbins T, Curran H, de Wit H. Special issue on impulsivity and compulsivity. Psychopharmacology (Berl) [Internet]. 2012 Jan 29 [cited 2019 May 22];219(2):251–2. Available from: http://link.springer.com/10.1007/s00213-011-2584-x. Accessed 22 May 2019.
Giel K, Teufel M, Junne F, Zipfel S, Schag K. Food-Related Impulsivity in Obesity and Binge Eating Disorder—A Systematic Update of the Evidence. Nutrients [Internet]. 2017 Oct 27 [cited 2019 May 22];9(11):1170. Available from: http://www.mdpi.com/2072-6643/9/11/1170. Accessed 22 May 2019.
Michaud A, Vainik U, Garcia-Garcia I, Dagher A. Overlapping Neural Endophenotypes in Addiction and Obesity. Front Endocrinol (Lausanne) [Internet]. 2017 Jun 14 [cited 2019 May 22];8. Available from: http://journal.frontiersin.org/article/10.3389/fendo.2017.00127/full. Accessed 22 May 2019.
Novelle MG, Diéguez C. Unravelling the role and mechanism of adipokine and gastrointestinal signals in animal models in the nonhomeostatic control of energy homeostasis: Implications for binge eating disorder. Eur Eat Disord Rev. 2018.
Dalley JW, Robbins TW. Fractionating impulsivity: neuropsychiatric implications. Nat Rev Neurosci [Internet]. 2017 Mar 1 [cited 2019 May 22];18(3):158–71. Available from: http://www.nature.com/articles/nrn.2017.8. Accessed 22 May 2019.
Cyders MA, Smith GT, Spillane NS, Fischer S, Annus AM, Peterson C. Integration of impulsivity and positive mood to predict risky behavior: development and validation of a measure of positive urgency. Psychol Assess. 2007;19(1):107–18.
Cyders MA, Smith GT. Emotion-based dispositions to rash action: positive and negative urgency. Psychol Bull [Internet]. 2008 Nov [cited 2019 May 22];134(6):807–28. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18954158. Accessed 22 May 2019.
Sinha R. Role of addiction and stress neurobiology on food intake and obesity. Biol Psychol [Internet]. 2018 Jan [cited 2019 May 22];131:5–13. Available from: https://linkinghub.elsevier.com/retrieve/pii/S030105111730087X. Accessed 22 May 2019.
Fineberg NA, Chamberlain SR, Goudriaan AE, Stein DJ, Vanderschuren LJMJ, Gillan CM, et al. New developments in human neurocognition: clinical, genetic, and brain imaging correlates of impulsivity and compulsivity. CNS Spectr [Internet]. 2014 Feb 11 [cited 2019 May 22];19(1):69–89. Available from: https://www.cambridge.org/core/product/identifier/S1092852913000801/type/journal_article. Accessed 22 May 2019.
Wu M, Brockmeyer T, Hartmann M, Skunde M, Herzog W, Friederich HC. Set-shifting ability across the spectrum of eating disorders and in overweight and obesity: a systematic review and meta-analysis. Psychol Med. 2014;44(16):3365–85.
Fagundo AB, de la Torre R, Jiménez-Murcia S, Agüera Z, Granero R, Tárrega S, et al. Executive Functions Profile in Extreme Eating/Weight Conditions: From Anorexia Nervosa to Obesity. Laks J, editor. PLoS One [Internet]. 2012 Aug 21 [cited 2019 Jun 6];7(8):e43382. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22927962. Accessed 22 May 2019.
Kakoschke N, Aarts E, Verdejo-García A. The Cognitive Drivers of Compulsive Eating Behavior. Front Behav Neurosci [Internet]. 2019 Jan 17 [cited 2019 May 22];12:338. Available from: https://www.frontiersin.org/article/10.3389/fnbeh.2018.00338/full. Accessed 22 May 2019.
Lavender JM, Goodman EL, Culbert KM, Wonderlich SA, Crosby RD, Engel SG, et al. Facets of Impulsivity and Compulsivity in Women with Anorexia Nervosa. Eur Eat Disord Rev [Internet]. 2017 Jul [cited 2019 Jun 6];25(4):309–13. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28387426. Accessed 22 May 2019.
García-García I, Horstmann A, Jurado MA, Garolera M, Chaudhry SJ, Margulies DS, et al. Reward processing in obesity, substance addiction and non-substance addiction. Obes Rev. 2014;15(11):853–69.
Stice E, Burger K. Neural vulnerability factors for obesity. Clin Psychol Rev [Internet]. 2019 Mar [cited 2019 May 22];68:38–53. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30587407. Accessed 22 May 2019.
García-García I, Narberhaus A, Marqués-Iturria I, Garolera M, Rădoi A, Segura B, et al. Neural Responses to Visual Food Cues: Insights from Functional Magnetic Resonance Imaging. Eur Eat Disord Rev [Internet]. 2013 Mar [cited 2019 Jun 6];21(2):89–98. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23348964. Accessed 22 May 2019.
Chow MSM, Wu SL, Webb SE, Gluskin K, Yew DT. Functional magnetic resonance imaging and the brain: A brief review. World J Radiol [Internet]. 2017 Jan 28 [cited 2019 May 22];9(1):5–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28144401. Accessed 22 May 2019.
Ugurbil K. What is feasible with imaging human brain function and connectivity using functional magnetic resonance imaging. Philos Trans R Soc B Biol Sci [Internet]. 2016 Oct 5 [cited 2019 May 22];371(1705):20150361. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27574313. Accessed 22 May 2019.
Steward T, Menchon JM, Jiménez-Murcia S, Soriano-Mas C, Fernandez-Aranda F. Neural Network Alterations Across Eating Disorders: A Narrative Review of fMRI Studies. Curr Neuropharmacol [Internet]. 2018 Aug 21 [cited 2019 May 22];16(8):1150–63. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29046154. Accessed 22 May 2019.
Frank GKW. Advances from neuroimaging studies in eating disorders. CNS Spectr [Internet]. 2015 Aug 23 [cited 2019 May 22];20(4):391–400. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25902917. Accessed 22 May 2019.
Berner LA, Brown TA, Lavender JM, Lopez E, Wierenga CE, Kaye WH. Neuroendocrinology of reward in anorexia nervosa and bulimia nervosa: Beyond leptin and ghrelin. Mol Cell Endocrinol [Internet]. 2018 Nov 2 [cited 2019 May 22]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/30395874. Accessed 22 May 2019.
Mobbs O, Crépin C, Thiéry C, Golay A, Van der Linden M. Obesity and the four facets of impulsivity. Patient Educ Couns. 2010;79(3):372–7.
Sellbom KS, Gunstad J. Cognitive Function and Decline in Obesity. Frisardi V, Imbimbo B, editors. J Alzheimer’s Dis. 2012;30(s2):S89–95.
Stoeckel LE, Weller RE, Cook EW, Twieg DB, Knowlton RC, Cox JE. Widespread reward-system activation in obese women in response to pictures of high-calorie foods. Neuroimage [Internet]. 2008 Jun [cited 2019 May 22];41(2):636–47. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18413289
Rothemund Y, Preuschhof C, Bohner G, Bauknecht H-C, Klingebiel R, Flor H, et al. Differential activation of the dorsal striatum by high-calorie visual food stimuli in obese individuals. Neuroimage [Internet]. 2007 Aug 15 [cited 2019 May 22];37(2):410–21. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17566768
McCaffery JM, Haley AP, Sweet LH, Phelan S, Raynor HA, Del Parigi A, et al. Differential functional magnetic resonance imaging response to food pictures in successful weight-loss maintainers relative to normal-weight and obese controls. Am J Clin Nutr [Internet]. 2009 Oct 1 [cited 2019 May 22];90(4):928–34. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19675107. Accessed 22 May 2019.
Castellanos EH, Charboneau E, Dietrich MS, Park S, Bradley BP, Mogg K, et al. Obese adults have visual attention bias for food cue images: evidence for altered reward system function. Int J Obes [Internet]. 2009 Sep 21 [cited 2019 May 22];33(9):1063–73. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19621020. Accessed 22 May 2019.
Batterink L, Yokum S, Stice E. Body mass correlates inversely with inhibitory control in response to food among adolescent girls: an fMRI study. Neuroimage [Internet]. 2010 Oct 1 [cited 2019 May 22];52(4):1696–703. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20510377. Accessed 22 May 2019.
Bruce AS, Holsen LM, Chambers RJ, Martin LE, Brooks WM, Zarcone JR, et al. Obese children show hyperactivation to food pictures in brain networks linked to motivation, reward and cognitive control. Int J Obes. 2010;34(10):1494–500.
Zeeb FD, Floresco SB, Winstanley CA. Contributions of the orbitofrontal cortex to impulsive choice: interactions with basal levels of impulsivity, dopamine signalling, and reward-related cues. Psychopharmacology. 2010;211(1):87–98.
Rolls ET. The Orbitofrontal Cortex and Reward. Cereb Cortex [Internet]. 2000 Mar 1 [cited 2019 May 22];10(3):284–94. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10731223. Accessed 22 May 2019.
Fineberg NA, Potenza MN, Chamberlain SR, Berlin HA, Menzies L, Bechara A, et al. Probing compulsive and impulsive behaviors, from animal models to endophenotypes: a narrative review. Neuropsychopharmacology. 2010;35(3):591–604.
Yokum S, Ng J, Stice E. Attentional Bias to Food Images Associated With Elevated Weight and Future Weight Gain: An fMRI Study. Obesity [Internet]. 2011 Sep 16 [cited 2019 May 22];19(9):1775–83. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21681221. Accessed 22 May 2019.
Marqués-Iturria I, Scholtens LH, Garolera M, Pueyo R, García-García I, González-Tartiere P, et al. Affected connectivity organization of the reward system structure in obesity. Neuroimage [Internet]. 2015 May 1 [cited 2019 Jun 6];111:100–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25687594. Accessed 22 May 2019.
Uddin LQ. Salience processing and insular cortical function and dysfunction. Nat Rev Neurosci. 2015;16(1):55–61.
Martin LE, Holsen LM, Chambers RJ, Bruce AS, Brooks WM, Zarcone JR, et al. Neural Mechanisms Associated With Food Motivation in Obese and Healthy Weight Adults. Obesity [Internet]. 2010 Feb 23 [cited 2019 May 22];18(2):254–60. Available from: http://doi.wiley.com/10.1038/oby.2009.220. Accessed 22 May 2019.
Weygandt M, Mai K, Dommes E, Leupelt V, Hackmack K, Kahnt T, et al. The role of neural impulse control mechanisms for dietary success in obesity. Neuroimage [Internet]. 2013 Dec [cited 2019 May 22];83:669–78. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23867558. Accessed 22 May 2019.
Weygandt M, Mai K, Dommes E, Ritter K, Leupelt V, Spranger J, et al. Impulse control in the dorsolateral prefrontal cortex counteracts post-diet weight regain in obesity. Neuroimage [Internet]. 2015 Apr 1 [cited 2019 May 22];109:318–27. Available from: https://www.sciencedirect.com/science/article/pii/S1053811914010799. Accessed 22 May 2019.
Francis LA, Susman EJ. Self-regulation and rapid weight gain in children from age 3 to 12 years. Arch Pediatr Adolesc Med. 2009;163(4):297–302.
Seeyave DM, Coleman S, Appugliese D, Corwyn RF, Bradley RH, Davidson NS, et al. Ability to delay gratification at age 4 years and risk of overweight at age 11 years. Arch Pediatr Adolesc Med. 2009;163(4):303.
Stoeckel LE, Murdaugh DL, Cox JE, Cook EW, Weller RE. Greater impulsivity is associated with decreased brain activation in obese women during a delay discounting task. Brain Imaging Behav. 2013;7(2):116–28.
Steward T, Picó-Pérez M, Mata F, Martínez-Zalacaín I, Cano M, Contreras-Rodríguez O, et al. Emotion regulation and excess weight: impaired affective processing characterized by dysfunctional insula activation and connectivity. PLoS One. 2016;11(3):1–17. https://doi.org/10.1371/journal.pone.0152150.
Etkin A, Büchel C, Gross JJ. The neural bases of emotion regulation. Nat Rev Neurosci. 2015;16(11):693–700.
Ochsner KN, Silvers JA, Buhle JT. Functional imaging studies of emotion regulation: a synthetic review and evolving model of the cognitive control of emotion. Ann N Y Acad Sci [Internet]. 2012 Mar [cited 2019 May 22];1251(1):E1–24. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23025352. Accessed 22 May 2019.
Bongers P, Jansen A. Emotional Eating Is Not What You Think It Is and Emotional Eating Scales Do Not Measure What You Think They Measure. Front Psychol [Internet]. 2016 [cited 2019 May 22];7. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5143883/. Accessed 22 May 2019.
Martín-Pérez C, Contreras-Rodríguez O, Vilar-López R, Verdejo-García A. Hypothalamic Networks in Adolescents With Excess Weight: Stress-Related Connectivity and Associations With Emotional Eating. J Am Acad Child Adolesc Psychiatry [Internet]. 2018; Available from: https://linkinghub.elsevier.com/retrieve/pii/S0890856718319816. Accessed 22 May 2019.
García-García I, Jurado MÁ, Garolera M, Marqués-Iturria I, Horstmann A, Segura B, et al. Functional network centrality in obesity: A resting-state and task fMRI study. Psychiatry Res Neuroimaging [Internet]. 2015 Sep 30 [cited 2019 Jun 6];233(3):331–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26145769. Accessed 22 May 2019.
Doucet GE, Rasgon N, McEwen BS, Micali N, Frangou S. Elevated Body Mass Index is Associated with Increased Integration and Reduced Cohesion of Sensory-Driven and Internally Guided Resting-State Functional Brain Networks. Cereb Cortex [Internet]. 2017;(January 2017):988–97. Available from: https://academic.oup.com/cercor/article-lookup/doi/10.1093/cercor/bhx008. Accessed 22 May 2019.
Wijngaarden MA, Veer IM, SARB R, van Buchem MA, Willems van Dijk K, Pijl H, et al. Obesity is marked by distinct functional connectivity in brain networks involved in food reward and salience. Behav Brain Res [Internet]. 2015, 287:127–34. https://doi.org/10.1016/j.bbr.2015.03.016.
Volkow ND, Wang G-J, Tomasi D, Baler RD. The Addictive Dimensionality of Obesity. Biol Psychiatry [Internet]. 2013 May 1 [cited 2019 May 22];73(9):811–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23374642
Moore CF, Sabino V, Koob GF, Cottone P. Pathological Overeating: Emerging Evidence for a Compulsivity Construct. Neuropsychopharmacology [Internet]. 2017 Jun 6 [cited 2019 May 22];42(7):1375–89. Available from: http://www.nature.com/articles/npp2016269
Dallman MF, Pecoraro N, Akana SF, La Fleur SE, Gomez F, Houshyar H, et al. Chronic stress and obesity: a new view of "comfort food". Proc Natl Acad Sci U S A [Internet]. 2003 Sep 30 [cited 2019 May 22];100(20):11696–701. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12975524
Parylak SL, Koob GF, Zorrilla EP. The dark side of food addiction. Physiol Behav [Internet]. 2011 Jul 25 [cited 2019 May 22];104(1):149–56. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21557958
Corbit LH, Nie H, Janak PH. Habitual Alcohol Seeking: Time Course and the Contribution of Subregions of the Dorsal Striatum. Biol Psychiatry [Internet]. 2012 Sep 1 [cited 2019 May 22];72(5):389–95. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22440617
Everitt BJ, Robbins TW. Neural systems of reinforcement for drug addiction: from actions to habits to compulsion. Nat Neurosci [Internet]. 2005 Nov 26 [cited 2019 May 22];8(11):1481–9. Available from: http://www.nature.com/articles/nn1579
Contreras-Rodríguez O, Martín-Pérez C, Vilar-López R, Verdejo-Garcia A. Ventral and dorsal striatum networks in obesity: link to food craving and weight gain. Biol Psychiatry [Internet]. 2017;81(9):789–96. https://doi.org/10.1016/j.biopsych.2015.11.020.
Babbs RK, Sun X, Felsted J, Chouinard-Decorte F, Veldhuizen MG, Small DM. Decreased caudate response to milkshake is associated with higher body mass index and greater impulsivity. Physiol Behav [Internet]. 2013 Sep [cited 2019 May 22];121:103–11. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0031938413001017
Baek K, Morris LS, Kundu P, Voon V. Disrupted resting-state brain network properties in obesity: decreased global and putaminal cortico-striatal network efficiency. Psychol Med [Internet]. 2017 Mar [cited 2019 May 22];47(4):585–96. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27804899
Furlong TM, Jayaweera HK, Balleine BW, Corbit LH. Binge-Like Consumption of a Palatable Food Accelerates Habitual Control of Behavior and Is Dependent on Activation of the Dorsolateral Striatum. J Neurosci [Internet]. 2014 Apr 2 [cited 2019 May 22];34(14):5012–22. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24695718
van Steenbergen H, Watson P, Wiers RW, Hommel B, de Wit S. Dissociable corticostriatal circuits underlie goal-directed vs. cue-elicited habitual food seeking after satiation: evidence from a multimodal MRI study. Eur J Neurosci [Internet]. 2017 Jul [cited 2019 May 22];46(2):1815–27. Available from: http://doi.wiley.com/10.1111/ejn.13586
Keiflin R, Janak PH. Dopamine Prediction Errors in Reward Learning and Addiction: From Theory to Neural Circuitry. Neuron [Internet]. 2015 Oct 21 [cited 2019 May 22];88(2):247–63. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26494275
Janssen LK, Duif I, van Loon I, Wegman J, de Vries JHM, Cools R, et al. Loss of lateral prefrontal cortex control in food-directed attention and goal-directed food choice in obesity. Neuroimage [Internet]. 2017 Feb 1 [cited 2019 May 22];146:148–56. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27845255
Mathar D, Neumann J, Villringer A, Horstmann A. Failing to learn from negative prediction errors: Obesity is associated with alterations in a fundamental neural learning mechanism. Cortex [Internet]. 2017 Oct [cited 2019 May 22];95:222–37. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28917135
Koob GF, Volkow ND. Neurobiology of addiction: a neurocircuitry analysis. The Lancet Psychiatry [Internet]. 2016 Aug [cited 2019 May 22];3(8):760–73. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27475769
Rangel A. Regulation of dietary choice by the decision-making circuitry. Nat Neurosci [Internet]. 2013 Dec 22 [cited 2019 May 22];16(12):1717–24. Available from: http://www.nature.com/articles/nn.3561
Mehl N, Morys F, Villringer A, Horstmann A. Unhealthy yet Avoidable-How Cognitive Bias Modification Alters Behavioral and Brain Responses to Food Cues in Individuals with Obesity. Nutrients [Internet]. 2019 Apr 18 [cited 2019 May 22];11(4):874. Available from: https://www.mdpi.com/2072-6643/11/4/874
Kullmann S, Heni M, Linder K, Zipfel S, Häring HU, Veit R, et al. Resting-state functional connectivity of the human hypothalamus. Hum Brain Mapp. 2014.
Contreras-Rodríguez O, Vilar-López R, Andrews ZB, Navas JF, Soriano-Mas C, Verdejo-García A. Altered cross-talk between the hypothalamus and non-homeostatic regions linked to obesity and difficulty to lose weight. Sci Rep. 2017;7(1):1–9.
Volkow ND, Wang G-J, Fowler JS, Telang F. Overlapping neuronal circuits in addiction and obesity: evidence of systems pathology. Philos Trans R Soc Lond B Biol Sci [Internet]. 2008 Oct 12 [cited 2019 May 22];363(1507):3191–200. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18640912
Puig J, Blasco G, Daunis-i-Estadella J, Molina X, Xifra G, Ricart W, et al. Hypothalamic Damage Is Associated With Inflammatory Markers and Worse Cognitive Performance in Obese Subjects. J Clin Endocrinol Metab [Internet]. 2015 Feb [cited 2019 Jun 6];100(2):E276–81. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25423565
Jastreboff AM, Sinha R, Arora J, Giannini C, Kubat J, Malik S, et al. Altered Brain Response to Drinking Glucose and Fructose in Obese Adolescents. Diabetes [Internet]. 2016 Jul [cited 2019 May 22];65(7):1929–39. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27207544
Kullmann S, Heni M, Veit R, Ketterer C, Schick F, Häring HU, et al. The obese brain: association of body mass index and insulin sensitivity with resting state network functional connectivity. Hum Brain Mapp. 2012;33(5):1052–61.
Kullmann S, Heni M, Veit R, Scheffler K, Machann J, Häring H-U, et al. Selective insulin resistance in homeostatic and cognitive control brain areas in overweight and obese adults. Diabetes Care. 2015;38(6):1044–50.
Heni M, Kullmann S, Ketterer C, Guthoff M, Bayer M, Staiger H, et al. Differential effect of glucose ingestion on the neural processing of food stimuli in lean and overweight adults. Hum Brain Mapp [Internet]. 2014 Mar [cited 2019 May 22];35(3):918–28. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23307469
Farooqi IS, Bullmore E, Keogh J, Gillard J, O’Rahilly S, Fletcher PC. Leptin Regulates Striatal Regions and Human Eating Behavior. Science [Internet]. 2007 [cited 2019 May 22];317(5843). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3838941/
Baicy K, London ED, Monterosso J, Wong M-L, Delibasi T, Sharma A, et al. Leptin replacement alters brain response to food cues in genetically leptin-deficient adults. Proc Natl Acad Sci [Internet]. 2007 Nov 13 [cited 2019 May 22];104(46):18276–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17986612
Farooqi IS, Bullmore E, Keogh J, Gillard J, O’Rahilly S, Fletcher PC. Leptin Regulates Striatal Regions and Human Eating Behavior. Science (80- ) [Internet]. 2007 Sep 7 [cited 2019 May 22];317(5843):1355–1355. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17690262
De Silva A, Salem V, Long CJ, Makwana A, Newbould RD, Rabiner EA, et al. The Gut Hormones PYY3–36 and GLP-17-36 amide Reduce Food Intake and Modulate Brain Activity in Appetite Centers in Humans. Cell Metab [Internet]. 2011 [cited 2019 May 22];14(5–2):700. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3267038/
Pannacciulli N, Le DSNT, Salbe AD, Chen K, Reiman EM, Tataranni PA, et al. Postprandial glucagon-like peptide-1 (GLP-1) response is positively associated with changes in neuronal activity of brain areas implicated in satiety and food intake regulation in humans. Neuroimage [Internet]. 2007 Apr 1 [cited 2019 May 22];35(2):511–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17317222
Le DSN, Pannacciulli N, Chen K, Salbe AD, Hill JO, Wing RR, et al. Less activation in the left dorsolateral prefrontal cortex in the reanalysis of the response to a meal in obese than in lean women and its association with successful weight loss. Am J Clin Nutr [Internet]. 2007 Sep 1 [cited 2019 May 22];86(3):573–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17823419
Batterham RL, Ffytche DH, Rosenthal JM, Zelaya FO, Barker GJ, Withers DJ, et al. PYY modulation of cortical and hypothalamic brain areas predicts feeding behaviour in humans. Nature. 2007;450(7166):106–9.
English PJ, Ghatei MA, Malik IA, Bloom SR, Wilding JPH. Food Fails to Suppress Ghrelin Levels in Obese Humans. J Clin Endocrinol Metab [Internet]. 2002 Jun [cited 2019 May 22];87(6):2984–2984. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12050284
Malik S, McGlone F, Bedrossian D, Dagher A. Ghrelin Modulates Brain Activity in Areas that Control Appetitive Behavior. Cell Metab [Internet]. 2008 May [cited 2019 May 22];7(5):400–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18460331
Zhang Y, Ji G, Li G, Hu Y, Liu L, Jin Q, et al. Ghrelin reductions following bariatric surgery were associated with decreased resting state activity in the hippocampus. Int J Obes [Internet]. 2019 Apr 18 [cited 2019 May 22];43(4):842–51. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29915363
Li G, Ji G, Hu Y, Liu L, Jin Q, Zhang W, et al. Reduced plasma ghrelin concentrations are associated with decreased brain reactivity to food cues after laparoscopic sleeve gastrectomy. Psychoneuroendocrinology [Internet]. 2019 Feb [cited 2019 May 22];100:229–36. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30388597
Steward T, Picó-Pérez M, Mestre-Bach G, Martínez-Zalacaín I, Suñol M, Jiménez-Murcia S, et al. A multimodal MRI study of the neural mechanisms of emotion regulation impairment in women with obesity. Transl Psychiatry. 2019;9, 194(1). https://doi.org/10.1038/s41398-019-0533-3.
Preuss H, Pinnow M, Schnicker K, Legenbauer T. Improving Inhibitory Control Abilities (ImpulsE)-A Promising Approach to Treat Impulsive Eating? Eur Eat Disord Rev [Internet]. 2017 Nov 1 [cited 2019 May 23];25(6):533–43. Available from: http://doi.wiley.com/10.1002/erv.2544
Horstmann A. It wasn’t me; it was my brain – Obesity-associated characteristics of brain circuits governing decision-making. Physiol Behav [Internet]. 2017 Jul 1 [cited 2019 May 23];176:125–33. Available from: https://www.sciencedirect.com/science/article/abs/pii/S003193841631109X?via%3Dihub
Vella S-LC, Pai NB. A narrative review of potential treatment strategies for food addiction. Eat Weight Disord - Stud Anorexia, Bulim Obes [Internet]. 2017 Sep 6 [cited 2019 May 23];22(3):387–93. Available from: http://link.springer.com/10.1007/s40519-017-0400-2
Stefanidis A, Oldfield BJ. Neuroendocrine mechanisms underlying bariatric surgery: Insights from human studies and animal models. Journal of Neuroendocrinology. 2017.
Steward T, Mestre-Bach G, Granero R, Sánchez I, Riesco N, Vintró-Alcaraz C, et al. Reduced plasma Orexin-a concentrations are associated with cognitive deficits in anorexia nervosa. Sci Rep. 2019;9(1):7910.
Imperatore R, Palomba L, Cristino L. Role of Orexin-a in hypertension and obesity. Curr Hypertens Rep. 2017;19(4):–34.
Göbel CH, Tronnier VM, Münte TF. Brain stimulation in obesity. Int J Obes. 2017;41(12):1721–7.
Fernandez-Real J-M, Serino M, Blasco G, Puig J, Daunis-i-Estadella J, Ricart W, et al. Gut Microbiota Interacts With Brain Microstructure and Function. J Clin Endocrinol Metab [Internet]. 2015 Dec 1 [cited 2019 Jun 6];100(12):4505–13. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26445114
Funding
This study is a result of the SLT006/17/00246 grant, funded by the Department of Health of the Generalitat de Catalunya by the call “Acció instrumental de programes de recerca orientats en l’àmbit de la recerca i la innovació en salut”. We thank CERCA Programme / Generalitat de Catalunya for institutional support. This work was also supported by Instituto de Salud Carlos III (PI17/01167, PI13/01958, and PI16/00889). CIBER Fisiopatología de la Obesidad y Nutrición (CIBERobn) and CIBER Salud Mental (CIBERsam) are initiatives of ISCIII. C.S-M. is funded by a ‘Miguel Servet’ contract from the Carlos III Health Institute (CPII16/00048). Partial funding support was received by EU (H2020; Eat2beNICE- Ref 728,018).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Trevor Steward and Romina Miranda-Olivos shared first authorship.
Rights and permissions
About this article
Cite this article
Steward, T., Miranda-Olivos, R., Soriano-Mas, C. et al. Neuroendocrinological mechanisms underlying impulsive and compulsive behaviors in obesity: a narrative review of fMRI studies. Rev Endocr Metab Disord 20, 263–272 (2019). https://doi.org/10.1007/s11154-019-09515-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11154-019-09515-x