Abstract
Purpose
Many patients with acute coronary syndrome experience problematic or altered sexual function. This aspect of the disease is frequently ignored or overlooked by the healthcare community even though it can strongly influence health-related patient quality of life (HRQoL). Thus, the aim of this study was to compare the effects of a specific cardiac rehabilitation programme focused on aerobic and neuromuscular strength-resistance training to those of a classic rehabilitation programme, both in terms of HRQoL and erectile dysfunction in patients with acute coronary syndrome.
Methods
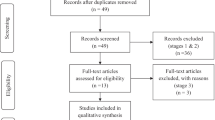
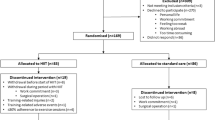
This study reports both secondary and unregistered outcomes from a double-blinded, randomised, and controlled clinical trial. The proposed intervention was based on the completion of a 20-session (10-week) cardiac rehabilitation programme for patients with cardiovascular disease. The patient cohort had been diagnosed with acute coronary syndrome and was recruited at the Cardiology Service of a private tertiary hospital. The outcomes assessed in this study were HRQoL and erectile disfunction assessed at baseline, after the intervention, and at a 6-month follow-up.
Results
A total of 30 participants were randomly allocated to each study arm. The results of the two-way mixed ANOVAs showed significant group × time interactions for all the outcome measures (EQ-5D_index, p = 0.004; EQ-5D_VAS, p = 0.017; QLMI-Q, p ≤ 0.001; and IIEF-5, p = 0.001).
Conclusion
The neuromuscular strength training programme was more effective than the classic strength training programme in terms of increasing the HRQoL and improving erectile dysfunction in patients following acute coronary syndrome, with differences still remaining between these groups at the 6-month follow-up.


Similar content being viewed by others
Data availability
Derived data supporting the findings of this study are available from the corresponding author MLLV on request.
References
Haraldstad, K., Wahl, A., Andenæs, R., Andersen, J. R., Andersen, M. H., Beisland, E., Borge, C. R., Engebretsen, E., Eisemann, M., Halvorsrud, L., Hanssen, T. A., Haugstvedt, A., Haugland, T., Johansen, V. A., Larsen, M. H., Løvereide, L., Løyland, B., Kvarme, L. G., Moons, P., & Norekvål, T. M. (2019). A systematic review of quality of life research in medicine and health sciences. Qual. life Res. Int. J. Qual. Life Asp. Treat. Care Rehabilit., 28(10), 2641–2650. https://doi.org/10.1007/s11136-019-02214-9
WHO. Program of Mental Health: Measuring Quality of Life. WHO/MSA/MNH/PSF/97.4. WHO, Geneva, (1997).
Ralapanawa, U., & Sivakanesan, R. (2021). Epidemiology and the magnitude of coronary artery disease and acute coronary syndrome: a narrative review. J. Epidemiol. Global Health, 11(2), 169–177. https://doi.org/10.2991/jegh.k.201217.001
Mosack, V., Hill, T. J., & Steinke, E. E. (2015). Sexual concerns of cardiac patients: Predictors and the influence of specific sexual activities. Euro. J. Cardiovasc. Nurs., 14(1), 45–52. https://doi.org/10.1177/1474515113517782
DeBusk, R., Drory, Y., Goldstein, I., Jackson, G., Kaul, S., Kimmel, S. E., Kostis, J. B., Kloner, R. A., Lakin, M., Meston, C. M., Mittleman, M., Muller, J. E., Padma-Nathan, H., Rosen, R. C., Stein, R. A., & Zusman, R. (2000). Management of sexual dysfunction in patients with cardiovascular disease: recommendations of the princeton consensus panel. Am. J. Cardiol., 86(2A), 62F-68F. https://doi.org/10.1016/s0002-9149(00)01117-6
Fridlund, B. (2009). Healthy sexual life after a cardiac event: what do we know and what do we do now? Euro. J. Cardiovasc. Nurs., 8(3), 159–160. https://doi.org/10.1016/j.ejcnurse.2009.06.002
Patti, A., Merlo, L., Ambrosetti, M., & Sarto, P. (2021). Exercise-based cardiac rehabilitation programs in heart failure patients. Heart Fail. Clin., 17(2), 263–271. https://doi.org/10.1016/j.hfc.2021.01.007
Gierat-Haponiuk, K., Haponiuk, I., Szalewska, D., Chojnicki, M., Jaworski, R., Niedoszytko, P., Leszczyńska, K., & Bakuła, S. (2015). Effect of complex cardiac rehabilitation on physical activity and quality of life during long-term follow-up after surgical correction of congenital heart disease. Kardiol. Polska, 73(4), 267–273. https://doi.org/10.5603/KP.a2014.0206
Amedro, P., Gavotto, A., Bredy, C., & Guillaumont, S. (2017). Réadaptation cardiaque de l’enfant et l’adulte avec une cardiopathie congénitale [Cardiac rehabilitation for children and adults with congenital heart disease]. Presse Med., 46(5), 530–537. https://doi.org/10.1016/j.lpm.2016.12.001
Lawler, P. R., Filion, K. B., & Eisenberg, M. J. (2011). Efficacy of exercise-based cardiac rehabilitation post-myocardial infarction: a systematic review and meta-analysis of randomized controlled trials. Am. Heart J., 162(4), 571-584.e2. https://doi.org/10.1016/j.ahj.2011.07.017
Long, L., Mordi, I. R., Bridges, C., Sagar, V. A., Davies, E. J., Coats, A. J., Dalal, H., Rees, K., Singh, S. J., & Taylor, R. S. (2019). Exercise-based cardiac rehabilitation for adults with heart failure. Cochrane Database Syst. Rev., 1(1), 003331. https://doi.org/10.1002/14651858.CD003331.pub5
Gadager, B. B., Tang, L. H., Ravn, M. B., Doherty, P., Harrison, A., Christensen, J., & Maribo, T. (2022). Benefits of cardiac rehabilitation following acute coronary syndrome for patients with and without diabetes: a systematic review and meta-analysis. BMC Cardiovasc. Disord., 22(1), 295.
Myer, G. D., Jayanthi, N., Difiori, J. P., Faigenbaum, A. D., Kiefer, A. W., Logerstedt, D., & Micheli, L. J. (2015). Sport specialization, part i: does early sports specialization increase negative outcomes and reduce the opportunity for success in young athletes? Sports Health, 7(5), 437–442. https://doi.org/10.1177/1941738115598747
Mischiati, C. R., Comerford, M., Gosford, E., Swart, J., Ewings, S., Botha, N., Stokes, M., & Mottram, S. L. (2015). Intra and inter-rater reliability of screening for movement impairments: movement control tests from the foundation matrix. J. Sports Sci. Med., 14(2), 427–440.
Zeng, C. Y., Zhang, Z. R., Tang, Z. M., & Hua, F. Z. (2021). Benefits and mechanisms of exercise training for knee osteoarthritis. Front. Physiol., 12, 794062. https://doi.org/10.3389/fphys.2021.794062
Jones, K., Hawke, F., Newman, J., Miller, J. A., Burns, J., Jakovljevic, D. G., Gorman, G., Turnbull, D. M., & Ramdharry, G. (2021). Interventions for promoting physical activity in people with neuromuscular disease. Cochrane Database Syst. Rev., 5(5), CD013544. https://doi.org/10.1002/14651858.CD013544.pub2
Skou, S. T., & Roos, E. M. (2017). Good Life with osteoArthritis in Denmark (GLA:D™): evidence-based education and supervised neuromuscular exercise delivered by certified physiotherapists nationwide. BMC Musculoskelet. Disord., 18(1), 72. https://doi.org/10.1186/s12891-017-1439-y
Ageberg, E., Nilsdotter, A., Kosek, E., & Roos, E. M. (2013). Effects of neuromuscular training (NEMEX-TJR) on patient-reported outcomes and physical function in severe primary hip or knee osteoarthritis: A controlled before-and-after study. BMC musculoskelet. Disord., 14, 232. https://doi.org/10.1186/1471-2474-14-232
Stensrud, S., Roos, E. M., & Risberg, M. A. (2012). A 12-week exercise therapy program in middle-aged patients with degenerative meniscus tears: a case series with 1-year follow-up. J. Orthop. Sports Phys. Ther., 42(11), 919–931. https://doi.org/10.2519/jospt.2012.4165
Eshoj, H. R., Rasmussen, S., Frich, L. H., Hvass, I., Christensen, R., Boyle, E., Jensen, S. L., Søndergaard, J., Søgaard, K., & Juul-Kristensen, B. (2020). Neuromuscular exercises improve shoulder function more than standard care exercises in patients with a traumatic anterior shoulder dislocation: a randomized controlled trial. Orthop. J. Sports Med., 8(1), 2325967119896102. https://doi.org/10.1177/2325967119896102
Ferrer-Sargues, F. J., Fabregat-Andrés, Ó., Martínez-Hurtado, I., Salvador-Coloma, P., Martínez-Olmos, F. J., Lluesma-Vidal, M., Biviá-Roig, G., Segrera-Rovira, M. J., Arguisuelas, M. D., & Valtueña-Gimeno, N. (2020). Effects of neuromuscular training compared to classic strength-resistance training in patients with acute coronary syndrome: a study protocol for a randomized controlled trial. PloS one, 15(12), e0243917. https://doi.org/10.1371/journal.pone.0243917
Fletcher, G. F., Ades, P. A., Kligfield, P., Arena, R., Balady, G. J., Bittner, V. A., Coke, L. A., Fleg, J. L., Forman, D. E., Gerber, T. C., Gulati, M., Madan, K., Rhodes, J., Thompson, P. D., Williams, M. A., American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee of the Council on Clinical Cardiology, Council on Nutrition, Physical Activity and Metabolism, Council on Cardiovascular and Stroke Nursing, and Council on Epidemiology and Prevention. (2013). Exercise standards for testing and training: a scientific statement from the American Heart Association. Circulation, 128(8), 873–934. https://doi.org/10.1161/CIR.0b013e31829b5b44
American College of Sports Medicine, ACSM´s guidelines for exercise testing and prescription 8/E. Ed. Paidotribo. (2019) ISBN 978–84–9910–425–6
Herdman, M., Badia, X., & Berra, S. (2001). El EuroQol-5D: una alternativa sencilla para la medición de la calidad de vida relacionada con la salud en atención primaria [EuroQol-5D: a simple alternative for measuring health-related quality of life in primary care]. Aten. Prim., 28(6), 425–30. https://doi.org/10.1016/s0212-6567(01)70406-4
Velasco, J. A., del Barrio, V., Mestre, M. V., Penas, C., & Ridocci, F. (1993). Validación de un nuevo cuestionario para evaluar la calidad de vida en pacientes postinfarto [Validation of a new questionnaire to evaluate the quality of life in patients after myocardial infarction]. Revista española de cardiologia, 46(9), 552–558.
Hernandez, G., Garin, O., Pardo, Y., Vilagut, G., Pont, À., Suárez, M., Neira, M., Rajmil, L., Gorostiza, I., Ramallo-Fariña, Y., Cabases, J., Alonso, J., & Ferrer, M. (2018). Validity of the EQ-5D-5L and reference norms for the Spanish population. Qual. Life Res. Int. J. Qual. Life Asp. Treat., Care Rehabilit., 27(9), 2337–2348. https://doi.org/10.1007/s11136-018-1877-5
Fernández-de-Las-Peñas, C., Rodríguez-Jiménez, J., Moro-López-Menchero, P., Cancela-Cilleruelo, I., Pardo-Hernández, A., Hernández-Barrera, V., & Gil-de-Miguel, Á. (2022). Psychometric properties of the Spanish version of the EuroQol-5D-5L in previously hospitalized COVID-19 survivors with long COVID. Sci. Rep., 12(1), 12605. https://doi.org/10.1038/s41598-022-17033-1
De Smedt, D., Clays, E., Doyle, F., Kotseva, K., Prugger, C., Pająk, A., Jennings, C., Wood, D., De Bacquer, D., EUROASPIRE Study Group. (2013). Validity and reliability of three commonly used quality of life measures in a large European population of coronary heart disease patients. Int. J. Cardiol., 167(5), 2294–2299. https://doi.org/10.1016/j.ijcard.2012.06.025
Rosen, R. C., Cappelleri, J. C., Smith, M. D., Lipsky, J., & Peña, B. M. (1999). Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int. J. Impot. Res., 11(6), 319–326. https://doi.org/10.1038/sj.ijir.3900472
Mert, K. U., Dural, M., Mert, G. Ö., Iskenderov, K., & Özen, A. (2018). Effects of heart rate reduction with ivabradine on the international index of erectile function (IIEF-5) in patients with heart failure. Aging Male Off. J. Int. Soc. Study Aging Male, 21(2), 93–98. https://doi.org/10.1080/13685538.2017.1369943
Saghaei, M. (2004). Random allocation software for parallel group randomized trials. BMC Med. Res. Methodol., 4, 26. https://doi.org/10.1186/1471-2288-4-26
Faul, F., Erdfelder, E., Buchner, A., & Lang, A. G. (2009). Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav. Res. Methods, 41(4), 1149–1160. https://doi.org/10.3758/BRM.41.4.1149
Cohen, J. (1988). The concepts of power analysis. Statistical power analysis for the behavioral sciences. Hillsdale: Elrbaum.
Carey, R. M., Whelton, P. K., 2017 ACC/AHA Hypertension Guideline Writing Committee. (2018). Prevention, detection, evaluation, and management of high blood pressure in adults: synopsis of the 2017 American college of cardiology/American heart association hypertension guideline. Ann. Intern. Med., 168(5), 351–358. https://doi.org/10.7326/M17-3203
Williams, D. (1999). Life events and career change: Transition psychology in practice, in British psychological society’s occupational psychology conference pp. 01–1999.
Rumsfeld, J. S., Alexander, K. P., Goff, D. C., Jr., Graham, M. M., Ho, P. M., Masoudi, F. A., Moser, D. K., Roger, V. L., Slaughter, M. S., Smolderen, K. G., Spertus, J. A., Sullivan, M. D., Treat-Jacobson, D., Zerwic, J. J., American Heart Association Council on Quality of Care and Outcomes Research, Council on Cardiovascular and Stroke Nursing, Council on Epidemiology and Prevention, Council on Peripheral Vascular Disease, and Stroke Council. (2013). Cardiovascular health: the importance of measuring patient-reported health status: a scientific statement from the American Heart Association. Circulation, 127(22), 2233–2249. https://doi.org/10.1161/CIR.0b013e3182949a2e
Whalley, B., Rees, K., Davies, P., Bennett, P., Ebrahim, S., Liu, Z., West, R., Moxham, T., Thompson, D. R., & Taylor, R. S. (2011). Psychological interventions for coronary heart disease. Cochrane Database Syst. Rev., 8, CD002902. https://doi.org/10.1002/14651858.CD002902.pub3
Ruano-Ravina, A., Pena-Gil, C., Abu-Assi, E., Raposeiras, S., V’ant Hof, A., Meindersma, E., & Prescott, E. I. B. (2016). Participation and adherence to cardiac rehabilitation programs. A systematic review. Int. J. Cardiol., 223, 436–443. https://doi.org/10.1016/j.ijcard.2016.08.120
Ozemek, C., & Squires, R. W. (2021). Enrollment and adherence to early outpatient and maintenance cardiac rehabilitation programs. J. Cardiopulm. Rehabilit. Prev., 41(6), 367–374. https://doi.org/10.1097/HCR.0000000000000645
Richards, S. H., Anderson, L., Jenkinson, C. E., Whalley, B., Rees, K., Davies, P., Bennett, P., Liu, Z., West, R., Thompson, D. R., & Taylor, R. S. (2017). Psychological interventions for coronary heart disease. Cochrane Database of Syst. Rev., 4(4), CD102902. https://doi.org/10.1002/14651858.CD002902.pub4
Yafi, F. A., Jenkins, L., Albersen, M., Corona, G., Isidori, A. M., Goldfarb, S., Maggi, M., Nelson, C. J., Parish, S., Salonia, A., Tan, R., Mulhall, J. P., & Hellstrom, W. J. (2016). Erectile dysfunction. Nat. Rev. Dis. Primers, 2, 16003. https://doi.org/10.1038/nrdp.2016.3
Milani, R. V., & Lavie, C. J. (2007). Impact of cardiac rehabilitation on depression and its associated mortality. Am. J. Med., 120(9), 799–806. https://doi.org/10.1016/j.amjmed.2007.03.026
Khan, Z., Musa, K., Abumedian, M., & Ibekwe, M. (2021). Prevalence of depression in patients with post-acute coronary syndrome and the role of cardiac rehabilitation in reducing the risk of depression: a systematic review. Cureus, 13(12), e20851. https://doi.org/10.7759/cureus.20851
Silva, A. B., Sousa, N., Azevedo, L. F., & Martins, C. (2017). Physical activity and exercise for erectile dysfunction: systematic review and meta-analysis. Br. J. Sports Med., 51(19), 1419–1424. https://doi.org/10.1136/bjsports-2016-096418
Lange, R. A., & Levine, G. N. (2014). Sexual activity and ischemic heart disease. Curr. Cardiol. Reprts, 16(2), 445. https://doi.org/10.1007/s11886-013-0445-4
Duca, Y., Calogero, A. E., Cannarella, R., Giacone, F., Mongioi, L. M., Condorelli, R. A., & La Vignera, S. (2019). Erectile dysfunction, physical activity and physical exercise: recommendations for clinical practice. Andrologia, 51(5), e13264. https://doi.org/10.1111/and.13264
Kałka, D., Domagała, Z., Dworak, J., Womperski, K., Rusiecki, L., Marciniak, W., Adamus, J., & Pilecki, W. (2013). Association between physical exercise and quality of erection in men with ischaemic heart disease and erectile dysfunction subjected to physical training. Kardiol. Polska, 71(6), 573–580. https://doi.org/10.5603/KP.2013.0120
Weibel, L., Massarotto, P., Hediger, H., & Mahrer-Imhof, R. (2016). Early education and counselling of patients with acute coronary syndrome. A pilot study for a randomized controlled trial. Euro. J. Cardiovasc. Nurs., 15(4), 213–222. https://doi.org/10.1177/1474515114556713
Cojocariu, S. A., Maștaleru, A., Sascău, R. A., Stătescu, C., Mitu, F., Cojocaru, E., Trandafir, L. M., & Leon-Constantin, M. M. (2021). Relationships between psychoeducational rehabilitation and health outcomes-a systematic review focused on acute coronary syndrome. J. Personal. Med., 11(6), 440. https://doi.org/10.3390/jpm11060440
Ponholzer, A., Gutjahr, G., Temml, C., & Madersbacher, S. (2010). Is erectile dysfunction a predictor of cardiovascular events or stroke? A prospective study using a validated questionnaire. Int. J. Impot. Res., 22(1), 25–29. https://doi.org/10.1038/ijir.2009.40
Nascimento, E. R., Maia, A. C., Pereira, V., Soares-Filho, G., Nardi, A. E., & Silva, A. C. (2013). Sexual dysfunction and cardiovascular diseases: a systematic review of prevalence. Clinics, 68(11), 1462–1468. https://doi.org/10.6061/clinics/2013(11)13
Author information
Authors and Affiliations
Contributions
Conceptualisation: VGN, F-SFJ, and L-VM; methodology: VGN, F-SFJ, and F-AÓ; patient selection and recruitment: F-SFJ and F-AÓ; rehabilitation training and outcomes: VGN, F-SFJ, L-VM, M-HI, and Martinez-Olmos, Francisco José; measures and data acquisition: VGN, L-VM, and AMD; software, validation, data curation and formal analysis: F-AÓ and AMD; writing (original draft preparation): F-SFJ and L-VM; writing (review and editing): F-AÓ, VGN, AMD, M-HI, and M-OFJ; visualisation, supervision, investigation, and resources: VGN, AMD, M-HI, and M-OFJ.
All the authors read and approved the final version of this manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have not disclosed any competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Valtueña-Gimeno, N., Ferrer-Sargues, F.J., Fabregat-Andrés, O. et al. The impact of a neuromuscular rehabilitation programme on the quality of life of patients with acute coronary syndrome and its relationship with sexual dysfunction: a randomised controlled trial. Qual Life Res 33, 433–442 (2024). https://doi.org/10.1007/s11136-023-03534-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-023-03534-7