Abstract
Purpose
The number of patients with depressive disordered globally increased and affects people of all ages and countries and has a significant and negative impact on the quality of life (QoL). Depression if left untreated may lead to severe consequences. However, there are several types of effective treatments, but often patients need support from health staff to find suitable treatments. This study aims to examine the global trend of the publications as well as the development of interventions for depressing treatment.
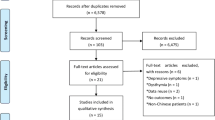
Methods
We download and analyzed 15,976 scientific research from the Web of Science from 1990 to 2018. A text mining based on Latent Dirichlet and terms’ co-occurrence in titles and abstracts to identify hidden research topics and research landscapes.
Results
We found that the number of papers related to non-pharmacological treatment (such as cognitive-behavioral, mindfulness, or family and social support) to improve the QoL of patients with depression has increased. The number of papers on this serious health issue in low–middle income countries (LMICs) was not as high as in high-income countries (HICs).
Conclusion
It is necessary to increase support of the treatment of depression in LMICs as well as applied non-pharmacological interventions to patients with depression.



Similar content being viewed by others
References
Paykel, E. S. (2008). Basic concepts of depression. Dialogues in Clinical Neuroscience, 10(3), 279–289.
Berrios, G. E. (1996). The history of mental symptoms: Descriptive psychopathology since the nineteenth century. Cambridge: Cambridge University Press.
World Health Organization. (1993). The ICD-10 classification of mental and behavioural disorders: Diagnostic criteria for research (Vol. 2). Geneva, Switzerland: World Health Organization.
Khoury, B., et al. (2013). Mindfulness-based therapy: A comprehensive meta-analysis. Clinical Psychology Review, 33(6), 763–771.
McCarter, T. (2008). Depression overview. American Health & Drug Benefits, 1(3), 44–51.
Marcus, M., et al. (2012). Depression: A global public health concern. World Health Organization Paper on Depression, 6–8.
Ho, R. C. M., et al. (2018). (2018) Factors associated with the risk of developing coronary artery disease in medicated patients with major depressive disorder. International Journal of Environmental Research and Public Health, 15(10), 2073.
Vigo, D., Thornicroft, G., & Atun, R. (2016). Estimating the true global burden of mental illness. The Lancet Psychiatry, 3(2), 171–178.
Bloom, D.E., et al. (2012). The global economic burden of noncommunicable diseases. Program on the Global Demography of Aging.
National Mental Health Commission Australian Government (2016). The economic cost of physical ill-health and serious mental illness. https://www.mentalhealthcommission.gov.au/news/2016/april/economic-cost-physical-health-and-mental-illness. Accessed 29 Oct 2019.
Ho, R. C., et al. (2013). The effect of severity of depressive disorder on economic burden in a university hospital in Singapore. Expert Review of Pharmacoeconomics & Outcomes Research, 13(4), 549–559.
Feng, L., Yap, K. B., & Ng, T. P. (2013). Depressive symptoms in older adults with chronic kidney disease: Mortality, quality of life outcomes, and correlates. The American Journal of Geriatric Psychiatry, 21(6), 570–579.
Ho, C. S., et al. (2014). Coexisting medical comorbidity and depression: Multiplicative effects on health outcomes in older adults. International Psychogeriatrics, 26(7), 1221–1229.
Group, W. (1995). The World Health Organization quality of life assessment (WHOQOL): Position paper from the World Health Organization. Social Science & Medicine, 41(10), 1403–1409.
Tan, S. H., et al. (2015). Determining the quality of life of depressed patients in Singapore through a multiple mediation framework. Asian Journal of Psychiatry, 18, 22–30.
Schuch, F. B., et al. (2016). Exercise improves physical and psychological quality of life in people with depression: A meta-analysis including the evaluation of control group response. Psychiatry Research, 241, 47–54.
Yang, W.-C., et al. (2017). Factors related to the improvement in quality of life for depressed inpatients treated with fluoxetine. BMC Psychiatry, 17(1), 309.
Dunner, D. L., et al. (2001). Improved health-related quality of life and reduced productivity loss after treatment with bupropion sustained release: A study in patients with major depression. Primary Care Companion to the Journal of Clinical Psychiatry, 3(1), 10.
Fu Keung Wong, D. (2008). Cognitive and health-related outcomes of group cognitive behavioural treatment for people with depressive symptoms in Hong Kong: Randomized wait-list control study. Australian & New Zealand Journal of Psychiatry, 42(8), 702–711.
Hofmann, S. G., et al. (2017). Effect of treatments for depression on quality of life: A meta-analysis. Cognitive Behaviour Therapy, 46(4), 265–286.
Anderson, N., & Ozakinci, G. (2018). Effectiveness of psychological interventions to improve quality of life in people with long-term conditions: Rapid systematic review of randomised controlled trials. BMC Psychology, 6(1), 11–11.
Tran, B. X., et al. (2019). Indices of change, expectations, and popularity of biological treatments for major depressive disorder between 1988 and 2017: A scientometric analysis. International Journal of Environmental Research and Public Health, 16(13), 2255.
Bornmann, L., & Leydesdorff, L. (2014). Scientometrics in a changing research landscape: Bibliometrics has become an integral part of research quality evaluation and has been changing the practice of research. EMBO Reports, 15(12), 1228–1232.
Martín-Martín, A., Orduna-Malea, E., & Delgado López-Cózar, E. (2018). Coverage of highly-cited documents in Google Scholar, Web of Science, and Scopus: A multidisciplinary comparison. Scientometrics, 116(3), 2175–2188.
Clarivate Analytics. Web of Science databases. Web of Science. https://clarivate.com/products/web-of-science/databases/. Accessed 26 June 2019.
Li, Y., et al. (2019). Leveraging latent Dirichlet allocation in processing free-text personal goals among patients undergoing bladder cancer surgery. Quality of Life Research, 28(6), 1441–1455.
Valle, D., et al. (2018). Extending the latent Dirichlet allocation model to presence/absence data: A case study on North American breeding birds and biogeographical shifts expected from climate change. Global Change Biology, 24(11), 5560–5572.
Chen, C., et al. (2017). Partial membership latent Dirichlet allocation for soft image segmentation. IEEE Transactions on Image Processing, 26(12), 5590–5602.
Lu, H. M., Wei, C. P., & Hsiao, F. Y. (2016). Modeling healthcare data using multiple-channel latent Dirichlet allocation. Journal of Biomedical Informatics, 60, 210–223.
Gross, A., & Murthy, D. (2014). Modeling virtual organizations with latent Dirichlet allocation: A case for natural language processing. Neural Networks, 58, 38–49.
Schwarz, C. (2018). ldagibbs: A command for topic modeling in Stata using latent Dirichlet allocation. The Stata Journal, 18(1), 101–117.
Blei, D. M., Ng, A. Y., & Jordan, M. I. (2002). Latent Dirichlet allocation. In Advances in neural information processing systems. Cambridge: MIT Press.
Brown, K. W., & Ryan, R. M. (2003). The benefits of being present: Mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology, 84(4), 822.
Asia, W. S.-E. (2017). Depression and suicide: Towards new paradigms in prevention and care. WHO South-East Asia Journal of Public Health, 6(1), 1–98.
Choo, C. C., et al. (2019). Health-related quality of life in pediatric patients with leukemia in Singapore: A Cross-Sectional Pilot Study. International Journal of Environmental Research and Public Health, 16(12), 2069.
Ho, R. C., et al. (2011). Clinical and psychosocial factors associated with depression and anxiety in Singaporean patients with rheumatoid arthritis. International Journal of Rheumatology, 14(1), 37–47.
Mak, A., et al. (2011). Damage accrual, cumulative glucocorticoid dose and depression predict anxiety in patients with systemic lupus erythematosus. Clinical Rheumatology, 30(6), 795–803.
Loh, A. Z., et al. (2017). The global prevalence of anxiety and depressive symptoms among caregivers of stroke survivors. Journal of the American Medical Directors Association, 18(2), 111–116.
Abraham, N., et al. (2019). A meta-analysis of the rates of suicide ideation, attempts and deaths in people with epilepsy. International Journal of Environmental Research and Public Health, 16(8), 1451.
Ho, R. C., & Mak, A. (2014). The interface between medicine and psychiatry: Neuropsychiatric aspects of systemic lupus erythematosus (SLE). Annals of the Academy of Medicine, Singapore, 43(8), 388–390.
Musiat, P., & Tarrier, N. (2014). Collateral outcomes in e-mental health: A systematic review of the evidence for added benefits of computerized cognitive behavior therapy interventions for mental health. Psychological Medicine, 44(15), 3137–3150.
Xiao, F., et al. (2017). Effectiveness of psychological interventions on depression in patients after breast cancer surgery: A meta-analysis of randomized controlled trials. Clinical Breast Cancer, 17(3), 171–179.
Huang, L., et al. (2018). Is cognitive behavioral therapy a better choice for women with postnatal depression? A systematic review and meta-analysis. PLoS ONE, 13(10), e0205243.
Zhang, M. W., & Ho, R. C. (2017). Moodle: The cost effective solution for internet cognitive behavioral therapy (I-CBT) interventions. Technology and Health Care, 25(1), 163–165.
Lu, Y., et al. (2017). Chronic administration of fluoxetine and pro-inflammatory cytokine change in a rat model of depression. PLoS ONE, 12(10), e0186700.
Bridges, L., & Sharma, M. (2017). The efficacy of yoga as a form of treatment for depression. Journal of Evidence-Based Complementary & Alternative Medicine, 22(4), 1017–1028.
Burnett-Zeigler, I., et al. (2016). Mind-body approaches to treating mental health symptoms among disadvantaged populations: A comprehensive review. Journal of Alternative and Complementary Medicine (New York, N.Y.), 22(2), 115–124.
Cramer, H., et al. (2013). Yoga for depression: A systematic review and meta-analysis. Depression and Anxiety, 30(11), 1068–1083.
Pascoe, M. C., & Bauer, I. E. (2015). A systematic review of randomised control trials on the effects of yoga on stress measures and mood. Journal of Psychiatric Research, 68, 270–282.
Ferguson, J. M. (2001). SSRI antidepressant medications: Adverse effects and tolerability. Primary Care Companion to the Journal of Clinical Psychiatry, 3(1), 22–27.
Zhang, M. W. B., & Ho, R. C. M. (2015). Ketamine’s potential as a rapid antidepressant was overplayed. BMJ: British Medical Journal, 351, 4467.
Zhang, M., et al. (2014). Application of low-cost methodologies for mobile phone app development. JMIR Mhealth Uhealth, 2(4), e55.
Fealy, S., et al. (2019). The Support for New Mums Project: A protocol for a pilot randomized controlled trial designed to test a postnatal psychoeducation smartphone application. Journal of Advanced Nursing, 75(6), 1347–1359.
Zhang, M. W., & Ho, R. C. (2017). Smartphone applications for immersive virtual reality therapy for internet addiction and internet gaming disorder. Technology and Health Care, 25(2), 367–372.
Zhang, M. W., et al. (2016). The alcohol tracker application: An initial evaluation of user preferences. BMJ Innovations, 2(1), 8–13.
Association, A. P. (2010). Treatment of patients with major depressive disorder. Practice guidelines. Washington, D.C.: AP Association.
Patel, V., et al. (2009). Packages of care for depression in low- and middle-income countries. PLoS Medicne, 6(10), e1000159.
Miller, G. (2006). Mental health in developing countries. The unseen: Mental illness's global toll. Science, 311(5760), 458–461.
Robertson, E., Celacun, N., & Stewart, D. (2003). Maternal mental health & child health and development. Geneva: WHO.
Pfeiffer, P. N., et al. (2011). Efficacy of peer support interventions for depression: A meta-analysis. General Hospital Psychiatry, 33(1), 29–36.
Latif, S., et al. (2017). Mobile health in the developing world: review of literature and lessons from a case study. IEEE Access, 5, 11540–11556.
Park, S. C., et al. (2014). Evidence-based, non-pharmacological treatment guideline for depression in Korea. Journal of Korean Medical Science, 29(1), 12–22.
Won, E., & Park, S. C. (2014). Evidence-based, pharmacological treatment guideline for depression in Korea. Journal of Korean Medical Science, 29(4), 468–484.
Lepine, B. A., et al. (2012). Treatment-resistant depression increases health costs and resource utilization. Brazilian Journal of Psychiatry, 34, 379–388.
Funding
No funding was received.
Author information
Authors and Affiliations
Contributions
BXT, GHH, CAL, CSHH, and RCMH developed the outline and contributed to analyses, interpreted results, and wrote the first and final drafts of the manuscript. BXT, GHH, DNN, TPN and HTD performed the literature search and data analysis, interpreted results, and wrote the manuscript. BXT, CAL, CSHH and RCMH critically revised the work. All author read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
This article does not contain any studies with human participants performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tran, B.X., Ha, G.H., Nguyen, D.N. et al. Global mapping of interventions to improve quality of life of patients with depression during 1990–2018. Qual Life Res 29, 2333–2343 (2020). https://doi.org/10.1007/s11136-020-02512-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-020-02512-7