Abstract
Purpose
We examined if child maltreatment (CM) is associated with worse health-related quality of life (HRQoL) in midlife women and if the association is mediated by psychosocial factors.
Methods
A total of 443 women were enrolled in the Pittsburgh site of the longitudinal Study of Women’s Health Across the Nation-Mental Health Study. The analytic sample included 338 women who completed the SF-36 and the Childhood Trauma Questionnaire. Generalized linear regression was used to assess the association between CM and two HRQoL component scores. Structural nested mean models were used to evaluate the contribution of each psychosocial mediator (lifetime psychiatric history, depressive symptoms, sleep problems, very upsetting life events, low social support) to the association.
Results
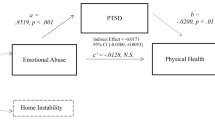
Thirty-eight percent of women reported CM. The mean mental (MCS) and physical (PCS) SF-36 component scores were 2.3 points (95% CI − 4.3, − 0.3) and 2.5 points (95% CI − 4.5, − 0.6) lower, respectively, in women with any CM than in those without. When number of CM types increased (0, 1, 2, 3+ types), group mean scores decreased in MCS (52, 51, 48, 47, respectively; p < .01) and PCS (52, 52, 49, 49, respectively; p = .03). In separate mediation analyses, depressive symptoms, very upsetting life events, or low social support, reduced these differences in MCS, but not PCS.
Conclusions
CM is a social determinant of midlife HRQoL in women. The relationship between CM and MCS was partially explained by psychosocial mediators. It is important to increase awareness among health professionals that a woman’s midlife well-being may be influenced by early-life adversity.

Similar content being viewed by others
Abbreviations
- BMI:
-
Body mass index
- CES-D:
-
Center for Epidemiologic Studies Depression scale
- CTQ:
-
Childhood Trauma Questionnaire
- CM:
-
Child maltreatment
- HRQoL:
-
Health-related quality of life
- MCS:
-
Mental component score
- PCS:
-
Physical component score
- SCID:
-
Structured clinical interview for the diagnosis of DSM-IV axis 1 disorders
- SES:
-
Socioeconomic status
- SF-36:
-
Medical outcomes survey short form 36
- SNMM:
-
Structural nested mean model
- SWAN-MHS:
-
Study of Women’s Health Across the Nation-Mental Health Study
References
Fayers, P. M., & Machin, D. (2016). Quality of life: The assessment, analysis and interpretation of patient-reported outcomes (3rd ed.). Chichester: Wiley.
Greenfield, E. A. (2010). Child abuse as a life-course social determinant of adult health. Maturitas, 66(1), 51–55.
Cutler, S. E., & Nolen-Hoeksema, S. (1991). Accounting for sex differences in depression through female victimization: Childhood sexual abuse. Sex Roles, 24(7), 425–438.
Weiss, E. L., Longhurst, J. G., & Mazure, C. M. (1999). Childhood sexual abuse as a risk factor for depression in women: Psychosocial and neurobiological correlates. American Journal of Psychiatry, 156(6), 816–828.
Afifi, T. O., Enns, M. W., Cox, B. J., de Graaf, R., ten Have, M., & Sareen, J. (2007). Child abuse and health-related quality of life in adulthood. Journal of Nervous and Mental Disease, 195(10), 797–804.
Cuijpers, P., Smit, F., Unger, F., Stikkelbroek, Y., ten Have, M., & de Graaf, R. (2011). The disease burden of childhood adversities in adults: A population-based study. Child Abuse Neglect, 35(11), 937–945.
Rikhye, K., Tyrka, A. R., Kelly, M. M., Gagne, G. G. Jr., Mello, A. F., Mello, M. F., et al. (2008). Interplay between childhood maltreatment, parental bonding, and gender effects: Impact on quality of life. Child Abuse Neglect, 32(1), 19–34.
Weber, S., Jud, A., & Landolt, M. A. (2016). Quality of life in maltreated children and adult survivors of child maltreatment: A systematic review. Quality of Life Research, 25(2), 237–255.
Bonomi, A. E., Cannon, E. A., Anderson, M. L., Rivara, F. P., & Thompson, R. S. (2008). Association between self-reported health and physical and/or sexual abuse experienced before age 18. Child Abuse Neglect, 32(7), 693–701.
Corso, P. S., Edwards, V. J., Fang, X., & Mercy, J. A. (2008). Health-related quality of life among adults who experienced maltreatment during childhood. American Journal of Public Health, 98(6), 1094–1100.
Dickinson, L. M., deGruy, F. V., Dickinson, W. P., & Candib, L. M. (1999). Health-related quality of life and symptom profiles of female survivors of sexual abuse. Archives of Family Medicine, 8(1), 35–43.
Draper, B., Pfaff, J. J., Pirkis, J., Snowdon, J., Lautenschlager, N. T., Wilson, I., et al. (2008). Long-term effects of childhood abuse on the quality of life and health of older people: Results from the Depression and Early Prevention of Suicide in General Practice Project. Journal of American Geriatrics Society, 56(2), 262–271.
Evren, C., Sar, V., Dalbudak, E., Cetin, R., Durkaya, M., Evren, B., et al. (2011). Lifetime PTSD and quality of life among alcohol-dependent men: Impact of childhood emotional abuse and dissociation. Psychiatry Research, 186(1), 85–90.
Walker, E. A., Gelfand, A., Katon, W. J., Koss, M. P., Von Korff, M., Bernstein, D., et al. (1999). Adult health status of women with histories of childhood abuse and neglect. American Journal of Medicine, 107(4), 332–339.
Agorastos, A., Pittman, J. O., Angkaw, A. C., Nievergelt, C. M., Hansen, C. J., Aversa, L. H., et al. (2014). The cumulative effect of different childhood trauma types on self-reported symptoms of adult male depression and PTSD, substance abuse and health-related quality of life in a large active-duty military cohort. Journal of Psychiatric Research, 58, 46–54.
Aversa, L. H., Lemmer, J., Nunnink, S., McLay, R. N., & Baker, D. G. (2014). Impact of childhood maltreatment on physical health-related quality of life in U.S. active duty military personnel and combat veterans. Child Abuse Neglect, 38(8), 1382–1388.
Vanderweele, T. J., Vansteelandt, S., & Robins, J. M. (2014). Effect decomposition in the presence of an exposure-induced mediator-outcome confounder. Epidemiology, 25(2), 300–306.
Sowers, M., Crawford, S., Sternfeld, B., Morganstein, D., Gold, E., Greendale, G., et al. (2000) SWAN: A multicenter, multiethnic, community-based cohort study of women and the menopausal transition. In: R. A. Lobo, J. Kelsey, & R. Marcus, Menopause: Biology and pathobiology (pp. 175–188). New York: Academic Press.
Spitzer, R. L., Williams, J. B., Gibbon, M., & First, M. B. (1992). The structured clinical interview for DSM-III-R (SCID). I: History, rationale, and description. Archives of General Psychiatry, 49(8), 624–629.
Ware, J. E., Snow, K. K., Kosinski, M. A., & Gandek, B. G. (1993). SF-36 health survey manual and interpretation guide. Boston: Health Institute, Boston New England Medical Centre.
Bernstein, D. P., Stein, J. A., Newcomb, M. D., Walker, E., Pogge, D., Ahluvalia, T., et al. (2003). Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Neglect, 27(2), 169–190.
Bernstein, D. P., Fink, L., Handelsman, L., Foote, J., Lovejoy, M., Wenzel, K., et al. (1994). Initial reliability and validity of a new retrospective measure of child abuse and neglect. American Journal of Psychiatry, 151(8), 1132–1136.
Ware, J. E. (1994). SF-36 physical and mental health summary scales: A user’s manual. Boston: Health Institute, New England Medical Center.
Bromberger, J. T., Kravitz, H. M., Chang, Y. F., Cyranowski, J. M., Brown, C., & Matthews, K. A. (2011). Major depression during and after the menopausal transition: Study of Women’s Health Across the Nation (SWAN). Psychological Medicine, 41(9), 1879–1888.
Radloff, L. S. (1977). The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401.
Dohrenwend, B. S., Askenasy, A. R., Krasnoff, L., & Bruce, P. (1978). Exemplification of a method for scaling life events: The PERI Life Events Scale. Journal of Health Social Behaviour, 19(2), 205–229.
Sherbourne, C. D., & Stewart, A. L. (1991). The MOS social support survey. Social Science Medicine, 32(6), 705–714.
Montez, J. K., Bromberger, J. T., Harlow, S. D., Kravitz, H. M., & Matthews, K. A. (2016). Life-course Socioeconomic Status and Metabolic Syndrome Among Midlife Women. Journal of Gerontology B Psychological Science Social Science, 71(6), 1097–1107.
World Health Organization. (1996). Research on the menopause in the 1990s: Report of a WHO scientific group. Geneva: World Health Organization (WHO).
Spielberger, C. D., & Reheiser, E. C. (2009). Assessment of emotions: Anxiety, anger, depression, and curiosity. Applied Psychology Health Well Being, 1(3), 271–302.
Yost, K. J., Haan, M. N., Levine, R. A., & Gold, E. B. (2005). Comparing SF-36 scores across three groups of women with different health profiles. Quality Life Research, 14(5), 1251–1261.
Norman, G. R., Sloan, J. A., & Wyrwich, K. W. (2003). Interpretation of changes in health-related quality of life: The remarkable universality of half a standard deviation. Medical Care, 41(5), 582–592.
Naimi, A. I., Schnitzer, M. E., Moodie, E. E., & Bodnar, L. M. (2016). Mediation analysis for health disparities research. American Journal of Epidemiology, 184(4), 315–324.
Fagundes, C. P., Lindgren, M. E., Shapiro, C. L., & Kiecolt-Glaser, J. K. (2012). Child maltreatment and breast cancer survivors: Social support makes a difference for quality of life, fatigue, and cancer stress. European Journal of Cancer, 48(5), 728–736.
Witt, A., Brown, R. C., Plener, P. L., Brähler, E., & Fegert, J. M. (2017). Child maltreatment in Germany: Prevalence rates in the general population. Child Adolescent Psychiatry Mental Health, 11, 47.
Stoltenborgh, M., Bakermans-Kranenburg, M. J., & van Ijzendoorn, M. H. (2013). The neglect of child neglect: A meta-analytic review of the prevalence of neglect. Social Psychiatry Psychiatric Epidemiology, 48, 345–355.
Kessler, R. C., Chiu, W. T., Demler, O., Merikangas, K. R., & Walters, E. E. (2005). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 617–627.
Center on the Developing Child at Harvard University. Building the Brain’s “Air Traffic Control” System: How early experiences shape the development of executive function: Working paper no. 11. National Scientific Council on the Developing Child. Published February 2011. Retrieved April 15, 2016, from https://developingchild.harvard.edu/wp-content/uploads/2011/05/How-Early-Experiences-Shape-the-Development-of-Executive-Function.pdf
Child Welfare Information Gateway. (2015). Understanding the effects of maltreatment on brain development. Washington, DC: U.S. Department of Health and Human Services, Children’s Bureau. Published April 2015. Retrieved April 14, 2016. https://www.childwelfare.gov/pubPDFs/brain_development.pdf.
Glaser, D. (2000). Child abuse and neglect and the brain-a review. Journal of Child Psychology Psychiatry, 41(1), 97–116.
Acknowledgments
In addition to the authors, the SWAN would like to acknowledge the contributions of the following: Clinical Centers: University of Michigan, Ann Arbor—Siobán Harlow, PI 2011–present, MaryFran Sowers, PI 1994–2011; Massachusetts General Hospital, Boston, MA—Joel Finkelstein, PI 1999–present; Robert Neer, PI 1994–1999; Rush University, Rush University Medical Center, Chicago, IL—Howard Kravitz, PI 2009–present; Lynda Powell, PI 1994–2009; University of California, Davis/Kaiser—Ellen Gold, PI; University of California, Los Angeles—Gail Greendale, PI; Albert Einstein College of Medicine, Bronx, NY—Carol Derby, PI 2011–present, Rachel Wildman, PI 2010–2011; Nanette Santoro, PI 2004–2010; University of Medicine and Dentistry—New Jersey Medical School, Newark—Gerson Weiss, PI 1994–2004; and the University of Pittsburgh, Pittsburgh, PA—Karen Matthews, PI. NIH Program Office: National Institute on Aging, Bethesda, MD—Chhanda Dutta 2016–present; Winifred Rossi 2012–2016; Sherry Sherman 1994–2012; Marcia Ory 1994–2001; National Institute of Nursing Research, Bethesda, MD—Program Officers. Central Laboratory: University of Michigan, Ann Arbor—Daniel McConnell (Central Ligand Assay Satellite Services). Coordinating Center: University of Pittsburgh, Pittsburgh, PA—Maria Mori Brooks, PI 2012–present; Kim Sutton-Tyrrell, PI 2001–2012; New England Research Institutes, Watertown, MA—Sonja McKinlay, PI 1995–2001. Steering Committee: Susan Johnson, Current Chair and Chris Gallagher, Former Chair. We also thank the study staff and all the women who participated in SWAN.
Funding
This research was part of the Study of Women’s Health Across the Nation (SWAN), which has grant support from the National Institutes of Health, Department of Health and Human Services, through the National Institute on Aging, the National Institute of Nursing Research, and the NIH Office of Research on Women’s Health (Grants Nos: U01NR004061, U01AG012505, U01AG012535, U01AG012531, U01AG012539, U01AG012546, U01AG012553, U01AG012554, U01AG012495). Supplemental funding from the National Institute of Mental Health (MH59689) is also gratefully acknowledged.
Author information
Authors and Affiliations
Contributions
All the authors participated in the design, execution, and analysis of the paper, and they have approved the final version. HHSL developed research hypotheses, performed statistical analyses, and wrote the entire manuscript. JTB reviewed and edited the entire manuscript to improve the focus and clarity. AIN provided knowledge and guidance for statistical analyses, particularly mediation analyses, and programming support. MMB provided input on statistical analyses and interpretation of findings. GAR reviewed and made suggestions for the entire manuscript and provided psychiatric expertise. JGB reviewed and helped in addressing the implications of study findings in community settings.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
The study was approved by the University of Pittsburgh Institutional Review Board. Informed consent was obtained from all individual participants included in the study.
Disclaimer
The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Aging, National Institute of Nursing Research, Office of Research on Women’s Health, or National Institutes of Health.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lin, HH.S., Naimi, A.I., Brooks, M.M. et al. Child maltreatment as a social determinant of midlife health-related quality of life in women: do psychosocial factors explain this association?. Qual Life Res 27, 3243–3254 (2018). https://doi.org/10.1007/s11136-018-1937-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-018-1937-x