Abstract
COVID-19 vaccine mandates are in place or being debated across the world. Standard neoclassical economics argues that the marginal social benefit from vaccination exceeds the marginal private benefit; everyone vaccinated against a given infectious disease protects others by not transmitting the disease. Consequently, private levels of vaccination will be lower than the socially optimal levels due to free-riding, which requires mandates to overcome the problem. We argue that universal mandates based on free-riding are less compelling for COVID-19. We argue that because the virus can be transmitted even after receiving the vaccine, most of the benefits of the COVID-19 vaccine are internalized: vaccinated individuals are protected from the worst effects of the disease. Therefore, any positive externality may be inframarginal or policy irrelevant. Even when all the benefits are not internalized by the individual, the externalities mainly are local, mostly affecting family and closely associated individuals, requiring local institutional (private and civil society) arrangements to boost vaccine rates, even in a global pandemic. Economists and politicians must justify such universal vaccine mandates on some basis other than free-riding.
Similar content being viewed by others
1 Introduction
This paper studies the economic rationale for universal vaccine mandates to battle the SARS-CoV-2 virus that led to the pandemic (commonly referred to as COVID-19) in the United States. We examine the nature of the consumption externality of the COVID-19 vaccine and ask if the externality is policy relevant. We find that the economic case for universal vaccine mandates, based on externality and free-riding, is weak for available COVID-19 vaccines, and that such vaccine mandates must be justified on some other basis.
Vaccine research and development often are recognized as global public goods when knowledge is shared across countries. Governments subsidize or support such R&D efforts through prizes, patent buyouts, or advance market commitments (Kremer et al., 2020; Tabarrok, 2020). In the United States, during the COVID-19 pandemic, the federal government procured vaccines and supplied them to the states, which then either followed or modified the guidelines of the Centers for Disease Control and Prevention (CDC) for prioritizing vaccine allocation (CDC 2022a). Similar efforts have been undertaken by the COVID-19 Vaccines Global Access (COVAX) alliance globally.
In addition to the supply side, sufficient demand is necessary to generate the benefits of the vaccine. To that end, strong calls for governmental mandates have been voiced. After an initial shortage and difficulties in scheduling vaccination appointments, by mid-April 2021, individuals residing in the United States who wanted to get vaccinated could do so without waiting (Howard, 2021). However, providing the vaccine at zero price with virtually no wait time has not led to near-universal adoption or, in some states, even majority adoption as of the end of 2021. For instance, in most states, a nontrivial proportion of healthcare workers, who were given top vaccination priority, have refused the vaccine (Shalby et al., 2020). Such evidence suggests that a price of zero was not sufficiently low to ensure universal vaccine consumption; to do so, the vaccines should have had a negative price. That is, the government should pay people to get vaccinated.
When a zero price does not generate sufficient demand for vaccines, the typical response is to call for various institutions, including different levels of government, to mandate vaccination, despite different levels of vaccine effectiveness. We see that policy response most recently against COVID-19 (Gostin et al., 2021; Stiglitz, 2021). Even prior to the COVID-19 pandemic, a large majority of economists argued that the benefits of mandated vaccines outweighed the costs, for example, in the case of measles (IGM Forum, 2015). Policymakers seem to agree. US federal, state, and city-wide mandates for COVID-19 vaccines are in force.Footnote 1 Of the six federal mandates, three remain in effect after being challenged in the US Supreme Court.Footnote 2 The vaccine mandates apply to healthcare workers,Footnote 3 military personnel,Footnote 4 and some categories of non-citizens traveling to the United States, subject to certain exceptions.Footnote 5 In addition to federal mandates, 20 statesFootnote 6 and 25 citiesFootnote 7 have mandated vaccination for different categories of workers with or without the alternative option of recurrent testing or recovery from previous infection.
In November 2021, the Biden Administration announced (White House, 2021b) that the Department of Labor’s Occupational Safety and Health Administration (OSHA) would require businesses with 100 or more employees—covering 84 million employees—to ensure that every worker is fully vaccinated or tests for COVID-19 infection on at least a weekly basis. Second, the Centers for Medicare & Medicaid Services (CMS) at the Department of Health and Human Services also required healthcare workers at facilities participating in the agency’s two entitlement programs to be fully vaccinated, a mandate that applied to more than 17 million workers. The goal of the mandates was to increase vaccination rates; both were challenged in the US Supreme Court. The US Supreme Court held the former mandate to be unconstitutional while allowing the mandate for healthcare centers. Forty-six other countries have issued vaccine mandates in various forms and scopes.Footnote 8 This paper explores the economic rationale for universal vaccine mandates, such as mandates at the federal or national level.
Economists recommending government interventions to increase vaccine uptake root their policy solutions in the free-rider problem associated with all viral diseases. Typically, everyone vaccinated against a given infectious disease protects themselves and protects others. If vaccines also protect others, the marginal social benefit from vaccination exceeds the marginal private benefit, creating the problem of free-riding and leading to underconsumption of the vaccine. For both efficiency reasons and distributive reasons, economists typically suggest a government intervention to correct the problem, usually in the form of a subsidy, and if that is insufficient, mandates. The standard economic argument in favor of vaccine mandates for various infectious diseases is that they help overcome the free-rider problem (Buttenheim & Asch, 2013; Gostin et al., 2021; Stiglitz, 2000).
As different kinds of government intervention to increase vaccination rates are debated, it is important to understand the nature of the externality posed by COVID-19 and the vaccines developed to protect against it. We put forward a simple argument in this paper: externalities and free-riding are not compelling in the case of the COVID-19 vaccine for which most of the benefits are internalized. Any call for mandates thus must be rooted in other justifications.
Our argument is as follows. An externality does not automatically imply free-riding. Most of the benefits from the vaccines developed to battle COVID-19 are internalized. That is because vaccinated individuals are protected from the most severe consequences of the infection, but they still can transmit the infection (albeit at lower rates than unvaccinated individuals). Any practical policy question cannot simply identify an externality and call for mandates but must examine the magnitudes of the policy’s private and social benefits. Furthermore, the externality is inframarginal, as defined by Buchanan and Stubblebine (1962). Externalities exist, but they are policy irrelevant. Whether an externality is inframarginal or not depends on the nature of the vaccine and many other factors, but most important, is institutionally contingent.
Second, even when the effects are not internalized fully, the external benefits of COVID vaccination are more local than global. Local public goods allow for more sorting and local “production”, which in this case means local incentives for vaccine uptake. Finally, if the non-universal adoption of a COVID-19 vaccine is related more to preferences and beliefs about the vaccine, the healthcare system, and government; then the argument is not about free-riding; the justification for mandates must come from elsewhere.
The case for universal vaccine mandates is not strongly grounded in explanations for underconsumption owing to a free-rider problem for the COVID-19 vaccine. Reasons unrelated to externalities and free-rider problems, but rooted in administrative convenience, politicization, misinformation, or paternalism, may justify vaccine mandates.
2 Externalities, public goods, and the free-rider problem with vaccination
Experts, economists, and policymakers have supported taxpayer funding or other support for vaccine development because vaccines serve as a global public good. In the absence of a pandemic, vaccine subsidies are ubiquitous because the development of pharmaceuticals and vaccines for infectious diseases can be very costly and subject to great uncertainty. During a pandemic, however, an early decision to subsidize the development, clinical trials, manufacturing, and delivery of a vaccine carry potentially large social benefits (Ahuja et al., 2021). Those benefits can be captured by subsidizing private research and development activities; negotiating contracts that guarantee a vaccine market, e.g., by committing to a minimum number of purchases (Kremer et al., 2020); or offering prizes and patent buyouts (Tabarrok, 2020). For instance, the US federal government’s Operation Warp Speed appropriated $10 billion to fund the development of COVID-19 vaccines and guaranteed that it would purchase a minimum number of doses to encourage production.
However, once a vaccine is developed and available widely, the consumption side becomes the relevant policy problem, raising the question of how to incentivize individuals to vaccinate. Some scholars refer to vaccines and the reduction of disease risk as pure public goods (Goodkin-Gold et al., 2020, p. 47). The public good argument is that vaccinations generate non-rival benefits (i.e., the benefit from a vaccinated individual does not decline as additional people encounter that individual), and non-exclusive benefits (i.e., once an individual has been vaccinated, she cannot easily exclude others from benefitting from her decision).
However, more than public goods, it is helpful to start with the more general language of externalities. Externalities can come in the form of net costs or benefits that an individual’s behavior imposes on others and that the individual does not consider. When any individual is vaccinated against an infectious disease, their chance of getting the disease is reduced. But vaccination also may reduce the chance of others getting the disease because the vaccine recipient is less likely to transmit it. If so, the social benefit from a dose of a vaccine exceeds the private benefit.
Although an individual benefits by being protected from infection, getting vaccinated is not costless. The costs usually are internalized, even if the vaccine is subsidized or made available at zero price. Logistical costs of getting vaccinated are borne by individuals as well as costs related to pain or adverse side effects (if any) from the vaccine. Such costs are nontrivial to the individual, as seen in higher rates of vaccine adoption when it is delivered orally (polio) versus injections (measles).
Incentives to free-ride by relying on others to vaccinate therefore may arise. We have so far not discussed magnitudes, just general directions. The exact magnitude of the free-riding will depend on the characteristics of the vaccine in question. For instance, in the case of the combined MMRV vaccine that protects against measles, mumps, rubella and varicella, 1-year antibody persistence rates for all four diseases exceed 95% (Lieberman et al., 2006). Many modern-day vaccines exhibit similarly high effectiveness against other diseases (Amanna & Slifka, 2020). The children vaccinated against MMRV protect themselves from the infectious diseases and protect others from infection by reducing transmission. The percentage of “breakthrough infections” is extremely low. Therefore, the marginal social benefit from vaccination is larger than the marginal private benefit and may create the dual problem of parents free-riding on community protection (“herd immunity”), thus leaving some children unvaccinated against MMRV. Kennedy and Gust (2008) documents that among church members reporting religious, safety, or philosophical objections to vaccination, vaccine hesitancy declined following a local measles outbreak, an action that is consistent with past free-riding.
In the face of vaccine free-riding, observers have called for mandates at different levels of government around the world. Browne (2016) analyzes California’s 2015 mandatory vaccine law for measles and concludes that it was justified in overcoming the free-rider problem and sharing the vaccination burden. Giubilini (2020) and Flanigan (2014) defend compulsory vaccination against pertussis, measles, and mumps, analogizing it to taxation and gun control. Van den Hoven (2012) and others contend that, owing to the unfairness of free-riding, parents have a moral duty to vaccinate their children.
While such framing of externalities has elicited criticism (Cowen, 1985, p. 58), it captures the collective-action problem that society faces in the case of vaccines. The Pigouvian solution, a subsidy, a mandate, or both for getting vaccinated, is considered to be the optimal policy response by many scholars (Francis, 2004; Goodkin-Gold et al., 2020). Stiglitz (2000) argues that vaccine mandates are a potential solution to the free-rider problem because they urge people to assume collective responsibility for preventing and eliminating infectious diseases.
We therefore can examine the problem through either lens because externalities and free-riding are considered to be “two sides of the same coin” (Cowen, 2002). The positive externality provided by vaccinated individuals, in sufficient numbers, can lead to free-riding by unvaccinated individuals. However, that rationale breaks down if the positive benefits of vaccination are excludable owing to technology or institutional arrangements. Even when the benefits of vaccination are not internalized fully and are excludable, free-riding may not arise. Not all vaccines are highly effective, at 95% rates, nor may they be durable so their effects wane over time. COVID-19 vaccines fall into that category.
Breakthrough infections, especially for newer variants, are frequent for COVID-19 vaccines, meaning that vaccinated individuals protect themselves against the most severe form of the disease. But they can still transmit the infection (albeit at lower rates) to others. Those characteristics make the externality arising from COVID-19 vaccines different from other vaccines that currently are mandated, at least for school-age children. The next section discusses the nature of the COVID-19 eternality in detail.
Although vaccine externalities are ubiquitous, the evidence for a free-rider problem is not always found. McKillop et al. (2019) do not uncover any evidence of free-riding in Human papillomavirus (HPV) vaccination drives in Dallas, Texas, but observe a positive and significant relationship between individual vaccine choices and average neighborhood vaccine rates. In other words, they observe clusters. Individuals were more likely to complete the HPV vaccination series when others in their neighborhood already had completed it. Holland and Zachary (2014) find that free-riding does not drive individual vaccine decisions and call the free-rider problem vis-à-vis mandatory vaccinations a “red herring”.
Even if no free-rider problem arises within a smaller group or neighborhood, vaccine mandates may be justified when and where vaccines have helped eliminate an infectious disease. In the case of smallpox, the vaccines that eradicated the virus successfully were a global public good. The benefits of vaccination were not just partially, but wholly non-excludable and non-rival, changing the nature of the free-rider problem. Even when a disease is eradicated locally, such as polio or measles in specific countries, the benefits are non-excludable and non-rival.
The discussion above brings us to the question of herd immunity. The herd immunity threshold is defined as “the proportion of a population immune to a communicable disease, either from innate immunity, natural infection, or vaccination, that prevents or significantly reduces serial transmission of its infectious agent.” The threshold differs across infectious diseases. The thresholds are predicted mathematically by relying on a transmissibility estimate called the reproductive number (or R0), but they likewise depend on the efficacy of vaccination, the prevalence of natural immunity, the durability of the protection, asymptomatic infections, population heterogeneity, and new mutations of the virus (epidemiologists call them “transitions”).
COVID-19 vaccines are less efficacious and durable than the MMRV vaccine, for which protection by vaccination or post-infection natural immunity tends to be lifelong. The argument, therefore, is that to reach the herd immunity threshold requires higher rates of COVID vaccination, justifying mandates with few exceptions.
Giurgea and Morens (2022) argue on the same grounds, however, that herd immunity for COVID-19 is neither easy to estimate nor attain through interventions because susceptibility to infection increases with the passage of time since vaccination. Herd immunity estimates for COVID-19 must account for lower vaccine efficacy, waning immunity, a dynamic mutating virus, and so on. Giurgea and Morens conclude that “current vaccine strategies may be able to slow down COVID-19 spread and are likely to alleviate the burden that waves of severe cases can inflict on limited health care resources, but they are unlikely to lead to COVID-19 eradication.” Therefore, economic arguments based on the non-excludable and non-rival public good characteristics of herd immunity, and the vaccine mandates aiming to achieve it, do not apply to COVID-19.
3 Is the positive externality from COVID-19 vaccines inframarginal?
Not every externality generates a free-rider problem. More generally, if most of the benefits and costs of an activity are internalized, free-riding is a smaller problem than commonly acknowledged. We argue that the current vaccines for COVID-19 do not pose a free-rider problem, especially against some variants. While unvaccinated people are by far at the highest risk for catching and spreading COVID-19, fully vaccinated persons can develop symptomatic or asymptomatic COVID-19 infections. And though the risk of transmission is much lower (half by some estimates; see Eyre et al., 2022), fully vaccinated individuals can transmit the infection to both vaccinated and unvaccinated people.
Scobie et al. (2021) studied 13 US jurisdictions from April 4 to July 17, 2021, when the Delta variant COVID-19 infection was predominant and found that age-standardized rates of reported cases were much higher among persons not fully vaccinated (112.3 per 100,000) than those fully vaccinated (10.1 per 100,000). Similarly, hospitalizations (9.1 versus 0.7 per 100,000), and deaths (1.6 versus 0.1 per 100,000) were much higher among persons not fully vaccinated than their fully vaccinated counterparts. Cross-country data on death rates by vaccination status across different variants of the infection also show that unvaccinated persons are far more likely to die (Mathieu & Roser, 2021).
Relying on CDC data from 26 states and two cities, the New York Times compared age-adjusted average daily case and death rates for vaccinated and unvaccinated people (New York Times, 2022). For example, during the Omicron wave (observations collected December 19–25, 2021), unvaccinated persons were twice as likely to contract COVID-19 and 20 times as likely to have a fatal infection, compared to fully vaccinated individuals.
It is now well established that even fully vaccinated individuals can get infected, even before the Omicron wave (Moghadas et al., 2021). Breakthrough infections across different variants and different parts of the world have been recorded (Araf et al., 2022). Based on the antibodies produced after vaccination, researchers have found that the Omicron variant is more skilled at evading immune responses (Lu et al., 2022). The Omicron wave saw record numbers of breakthrough infections, although fully vaccinated individuals are still protected from the most severe consequences.
Therefore, the benefits from the COVID-19 vaccines, mainly lowering the risk of hospitalization and much lower risk of death, are excludable, although not perfectly so. And while the social benefit from each vaccine dose exceeds its private benefits, a free-rider problem does not necessarily arise. The unvaccinated cannot derive much protection from the vaccinated during the COVID-19 pandemic, especially for newer variants. In fact, the opposite might be true. If vaccinated individuals are asymptomatic and out and about, they may place unvaccinated individuals at greater risk since it is harder to detect symptomless spreaders of the infection.
Externalities are ubiquitous, but not all of them require policy intervention. For instance, a well-kept front yard produces benefits in the form of aesthetic pleasure. And while various institutional mechanisms are available to internalize the spillover benefits to, say, neighbors, it is difficult to exclude an occasional passerby from enjoying the benefits of a beautiful yard. However, the decision of the homeowner to have a beautiful front yard may not be affected by the inability to exclude or charge the occasional bystander for “enjoying the view.” The spillover benefit here is one of an inframarginal externality, for which interventions will not increase supply on the margin. Private incentives to maintain a beautiful front yard (e.g., personal enjoyment, property value increases, viewers’ approbation) are sufficiently high for most homeowners to take appropriate action. The optimal amount of the good (“curb appeal”) gets produced and consumed; an externality exists, but it is inframarginal and not Pareto relevant (Buchanan & Stubblebine, 1962).Footnote 9
Whether an externality is inframarginal or not depends on various factors like technology, local context, and institutional arrangements that may preclude free-riding. Inframarginal externalities are of course subjective since some individuals may derive very high marginal private benefits from an activity like working on their gardens.
Individuals in the general population have strong private incentives to vaccinate themselves against COVID-19. First, vaccination will protect them from the worst effects of the disease. Vaccinated individuals are likely to have mild infections or remain asymptomatic. Second, vaccination will allow them to engage in social activities that were either not possible or too costly because of disease transmission risk. Third, it will facilitate entry to social groups and clubs that require participants to be vaccinated. For example, they can work at a grocery store, fly on an international air carrier, or attend a sporting event.
The impact of COVID-19 infection is not uniform across all individuals and groups. The elderly and people with comorbidities, especially heart disease, hypertension, or diabetes, are affected more severely than others (CDC, 2022b). For the Alpha and Delta variants, hospitalizations and fatalities are higher among individuals over 65 years of age (CDC, 2022c). For individuals in that age group or persons with comorbidities or other health conditions, getting vaccinated likely is privately and socially optimal (since self-isolation to avoid exposure as the other method of avoiding infection). The same incentives operate for individuals in occupations that face higher risks of contracting the virus, such as Uber drivers or checkout clerks. Some individuals also encounter more people, thereby passing on the benefits of their vaccination to others. But the private incentives to get vaccinated may be sufficiently strong that the benefit conferred on others is not relevant at the margin. If that is the case, the economic justification for universal vaccine mandates is weaker than commonly acknowledged because the externality may be inframarginal, which undermines free-rider problems.
4 Internalizing local externalities and institutional responses
If the benefits of a vaccine are not readily internalized, and various coordination and information problems prevent full Coasean bargaining (Coase, 1960), corrective intervention is not necessarily required because solutions can be found in a variety of institutional arrangements. Once again, consider a well-maintained front yard. A beautiful yard generates a positive externality for neighbors, not just because it is an attractive sight but also because it increases real estate values by increasing a home’s curb appeal (Johnson et al., 2020). Because not all of the aesthetic benefits of a garden are internalized and because yard maintenance carries a cost, standard theory predicts under-maintenance or underinvestment in front yards and curb appeal. But private solutions to the problem are available. One is for a single private entity (a monopolist) to internalize the externality (Demsetz, 1967, p. 348). The relevant actor typically is a private developer or a closed group such as a homeowners’ association that adopts rules about how yards are to be maintained and collects fees to ensure their maintenance. Such entities are clubs in the sense of Buchanan (1965). Another solution is Coasean bargaining between neighbors offering to help with yard work.
In the case of COVID-19, the negative externality of the disease and the positive externality from the vaccine depend on individuals’ interactions in close proximity to one another. Some of our daily interactions take place in public spaces, wherein interactions with strangers are not chosen explicitly. One cannot select the passengers with whom to travel on the subway and such interactions “may create cross-site externalities by increasing the infection risk of uninfected non-subway riders who later interact with subway riders at another site” (Leeson & Rouanet, 2021, p. 1109). Nor can one exclude others from riding on the subway. But many interactions occur at sites that are privately owned and that individuals visit voluntarily. In the absence of a vaccine, one can choose to patronize a grocery store rather than another that may be too crowded or shop at a less busy time of day. Therefore, people at risk of exposure to disease rationally can adapt their behavior, since externalities are bilateral in the Coasean sense.
Unlike interactions on public transportation or at the grocery store, many voluntary private interactions are at small-scale and repeated. We focus mainly on three types: private firms, private clubs, and civic associations. All of them can incentivize vaccination to internalize externalities among their members.
First, consider a firm that requires employees to work in close proximity. Evidence from pre-COVID-vaccine periods suggests that firms took steps to slow the spread of the virus (Mulligan, 2021). It may make sense for a business owner to mandate vaccination for the entire staff to internalize all of the benefits of vaccination and ensure no free-riding. Such a policy may sound extreme, but many real-world examples can be found in which vaccines are required as part of the job. For instance, seasonal flu shots are mandatory in some hospital wards and nursing homes; sex workers in the adult-entertainment industry must be vaccinated against hepatitis. Employer-mandated vaccinations are somewhat voluntary—an individual can always look for another job—but they are mandatory conditional on employment at a particular firm. One way of thinking about such mandates is that they are binding in the short run, when it may be difficult to find alternative employment, but voluntary in the medium to long run, when exit is possible. Second, such mandates are not universal. Third, controlling free-riding may not explain employers’ vaccination mandates; avoiding liability in the event of a workplace outbreak supplies a powerful incentive for requiring vaccinations.
For privately provisioned goods that are consumed collectively—such as airline travel—the mandates may extend beyond employees. Before the existence of a COVID-19 vaccine, some airlines mandated mask-wearing and proof of a negative test result for air travel. For international flights, some of the requirements were based on other countries’ immigration rules. But airlines also formulated their own rules for protecting passengers.
A private firm can incentivize vaccination, especially for employees, policy that typically is implemented by giving employees time off or having vaccine drives at the workplace, with monetary incentives or bonuses for getting vaccinated. The issue of transaction costs nevertheless arises. Consider a grocery store, such as Trader Joe’s. If the owners wish to internalize the externality, they must deal with two groups interacting in close physical proximity: employees and customers. They could mandate that everyone working in or patronizing all Trader Joe’s stores be vaccinated. That mandate would be a blunt policy that might not even be optimal for the purpose of internalizing externalities. The grocery chain’s store owners could provide free or subsidized vaccines or mandate the vaccine for employees, but for the hundreds of patrons visiting daily, the same policy would be prohibitively costly either because it would exclude many patrons or because checking customers’ vaccine certificates is too time consuming and troublesome.
Because the grocery store business is vigorously competitive, Trader Joe’s is not likely to be willing to check customers’ vaccine statuses for fear that some of them will shop elsewhere. Nor will Trader Joe’s subsidize its patrons’ vaccinations. Even if it did, the size of the subsidy offered (say, in the form of a discount) is unlikely to be large enough to narrow the gap much between the private and social marginal benefits of vaccination. Trader Joe’s employees are a different story. Unvaccinated workers potentially impose a negative externality on the chain’s store every working day. Employees also spend more time in the store than customers do, a relevant consideration for infectious diseases. Moreover, the mutual gains in the relationships between owners and employees are larger than between owners and customers. All else equal, we would expect Trader Joe’s to incentivize vaccinations of employees to a greater extent than they would incentivize vaccinations of customers. In fact, in January 2021, several retail stores, such as Trader Joe’s and Dollar General, announced that employees would be paid to get vaccinated (Miller, 2021). In February, Kroger (2021) announced that it would pay employees $100 to get the COVID-19 vaccine. Other private firms are considering similar incentives. In a recent poll conducted by the Yale Chief Executive Leadership Institute, 72% of current and former CEOs signaled an openness to vaccine mandates (Egan, 2020). One of the reasons private firms might not mandate COVID vaccines is legal uncertainty regarding vaccines approved for emergency use.
The second avenue of private solutions to inframarginal externalities is the institution of clubs. Buchanan’s (1965) theory of clubs explains how individuals and firms can supply public goods privately. Club goods typically are excludable (by charging membership fees) but non-rivalrous (or becoming rivalrous only beyond some congestion threshold, which is predetermined by the club facility’s capacity). It is profitable for firms or individuals to supply collectively consumed goods privately if they can persuade individuals to join the club to share the cost of providing the club good. The example Buchanan offers is a swimming pool. But the same underlying logic applies to the kind of positive externality created by excluding those who are unvaccinated from a club whose members are vaccinated. One of the goods or services provided is protection from getting infected by other club members owing to the club’s insistence on vaccination.
Typically, like privately owned firms, clubs adopt effective incentive-alignment mechanisms. The owners of clubs, which may be their members, are residual claimants over the revenues they generate from membership and user fees net of the costs of supplying the goods and services for which a club is established. During the pandemic, assuming a general preference for remaining COVID-19-free, more individuals are likely to get vaccinated if joining provides access to the club’s benefits, such as protection from disease transmission. Club owners capture profits only if its patrons are willing to pay; given a preference for protection from infectious diseases, the incentives of club owners and patrons are well aligned. Clubs also are exposed to market discipline—the freedom of their patrons to enter or exit—and such discipline applies competitive pressure on club management to cater to the preferences of their members. As a result, club managers must consider the costs of their mandates to ensure that they do not over-exclude. Finally, compared to other providers of collective goods such as the state, private clubs can adapt quickly since they can design and amend membership contracts for very specific situations.
Take swimming pools, gyms, and exercise facilities, which place people in close proximity while exercising and in common areas and changing rooms. Let us stipulate that conditional on believing that COVID-19 is an infectious disease with serious health consequences, patrons are likely to join only if all members take certain precautions. In the absence of a vaccine, clubs may enforce mask mandates and social-distancing rules. Once a vaccine becomes available, if members have a strong preference for having everyone in the group be vaccinated, then the club can mandate vaccines as a condition for inclusion. The transaction costs grocery stores face in checking vaccine records for all customers may be prohibitive. But clubs have solved that problem already (by their capacity choices and membership fee schedules) and need to add only one more membership requirement (vaccination).
Clubs also face incentives not to over-exclude and to cater to the preferences of their members. If the patrons are young and healthy and willing to risk some exposure to infection, the clubs may adopt mechanisms to accommodate them. For instance, the clubs may offer certain hours of operation for members who are vaccinated and other hours for anyone else, allowing patrons to choose the appropriate level of exposure to infection risk. In fact, before the availability of a vaccine, many gyms and exercise studios mandated masks during certain hours of operation; no masks were required at other times. Wearing a mask while working out intensely may impose high costs on some patrons, especially those who are young and likely to be asymptomatic or mildly symptomatic. Clubs therefore face strong incentives to impose mandates that align well with the preferences of their patrons.
While we have laid out a few specific incentive mechanisms that we expect (in the positive public choice sense of Leeson and Thompson (2021)), to observe in response to a pandemic, we have seen an even wider variety of attempts to encourage vaccination. The differences emerge from recognizing that vaccines generate both benefits and costs; incentives for behavioral changes thus must be tailored to the special circumstances of time and place.
For example, Kroger offered a lottery of $1 million and free groceries for a year to the winners (only the vaccinated were eligible); The Greenhouse offered pre-rolled marijuana joints under its “Pot for shots” campaign (Elassar, 2021); Krispy Kreme (Dickler, 2021), Chagrin Cinemas, and Samuel Adams (Tyko, 2021) gave out free donuts, popcorn, and beer, respectively, to those who showed their vaccine certificate. The National Football League announced that it would not extend the regular season to accommodate a COVID-19 outbreak among unvaccinated players, which lead to the forfeiting of games (Patra, 2021).
None of the examples just mentioned imply that decentralized social or nongovernmental mechanisms will reach an optimal allocation of resources. Instead, our argument simply is that social mechanisms can transform social benefits into private benefits, allowing people to internalize externalities in creative ways. If a free marijuana joint pushes a young person to get vaccinated, no other governmental subsidy or mandate is required. In fact, such intervention would be wasteful to the extent that it is financed or enforced by distortionary taxes somewhere else.
5 What type of policy response?
We do not mean to imply that no economic argument supports vaccine policy mandates. We mentioned the supply side previously. On the demand side, policy should, first, not get in the way. Certain state and private actions can block private incentives from arising to make the externality inframarginal. At the time of writing, vaccines developed by Moderna, Pfizer, and Johnson & Johnson have been approved by the US Food and Drug Administration for emergency use. Other vaccines, most notably AstraZeneca’s, the one adopted most widely by other countries, are still pending approval in the United States. Opacity concerning the FDA’s approval process may create uncertainty and foster mistrust. Furthermore, approval for emergency use may create legal problems for private firms and clubs seeking to enforce vaccine mandates for their employees.
The constructive role for public policy is twofold. First, policy can be justified if it reduces transaction costs sufficiently. While we have focused on the private mechanisms adopted by firms, clubs, and civil associations, governmental policies and private technologies may bolster the effectiveness of (or complement) private mechanisms by reducing the transaction costs faced by private actors and civil associations that check vaccines or mandate vaccines. This can be done through mechanisms such as a health pass. This is essentially a barcode that is given to every vaccinated individual and allows them access to providers of several collective goods and services, such as grocery stores, airlines, concert halls, sports centers, bars, and restaurants. The principle of exclusion at work in club goods is at work here. But monitoring and excluding can now be accomplished at lower transaction costs, without which private firms and individuals would not attempt these mechanisms. For example, in December 2020, Singapore Airlines introduced “health passports” (Thomas, 2020). That technology allows the airline to lower the cost of monitoring its own passengers, it could be used more broadly to verify vaccine status at a low cost to other organizations. Both private firms and local governments have introduced such passes in New York City, to provide ease of entry to restaurants, shops, and other local establishments.
When private arrangements or transaction cost-reducing policies above may not be sufficient, a question remains about the level of government at which a mandate should be adopted. It is not enough to point to the fact that one person’s vaccination decision has a tiny impact on other people all over the world. In practice, we need to look at both the relative and absolute magnitudes of the externalities.
For an analogy, consider the problem of littering. Littering is an externality. If your neighbor throws a plastic cup out his window on the way home, that cup has a chance (however small) of ending up in the farthest reaches of the ocean and thus being an externality on every other person on the earth. Given it has a positive chance of occurring, it is a global negative externality, strictly speaking. What should be the appropriate policy response to littering? There can be social pressures against littering. There are private solutions by providing trash cans. While there may be a role for some international agreements, it seems implausible that the bulk of the effort should be at the national or international scale.
Public goods and externalities are “two sides of the same coin.” We know from Tiebout (1956) sorting those local public goods can sometimes be dealt with through local policy. The sorting allows the local community to internalize the externality, not at the individual level, but at the appropriately defined local level. More than a theoretical possibility, there is evidence that cities internalize local externalities (Shoag & Veuger, 2018). The general principle is that the policy response may be dealt with at the level which experiences the bulk of the externality. Garbage thrown within someone’s house can be dealt with at the household level. Garbage thrown on the street can be dealt with at the neighborhood/city level.
We can apply this logic to vaccine mandates. If most of the benefits are local in nature, the appropriate policy response would be at the local level. Again, if this is the case, the economic case for universal vaccine mandates, at the federal level, is weaker than commonly acknowledged.
There is another kind of collective problem that we have not considered so far. Every society has limited hospital capacity, and no society develops infrastructure to treat most of the population at the same time, as it would be prohibitively costly. However, during a pandemic, a lot of people get sick at the same time, adding stress to the limited hospital infrastructure. Some aspects of the healthcare infrastructure are not elastic in the short run, and this kind of stress on the health infrastructure may result in poor quality care or, worse, a collapse of the system. This is the reason, in the absence of a vaccine, many countries mandated shutdowns and lockdowns so that the healthcare infrastructure does not collapse.
Some believe that stress on the (often state-provisioned or subsidized) healthcare system is a negative externality on the entire society, and therefore, vaccines should be mandated. Once again, given the presence of a vaccine, the private benefits from vaccination are very high. Therefore, in places where the vaccine supply and availability are not the problems, the proportion of unvaccinated, however large, is the relevant group that can overwhelm the healthcare infrastructure. In societies with high state capacity, this is not a problem, as the healthcare infrastructure is relatively robust. This can become a problem in areas with low state capacity and merit a vaccine mandate. However, we should caution that a society with low state capacity will also find it very difficult to enforce a universal vaccine mandate, and the intended result may not be achieved. Furthermore, if recovering from COVID-19 provides similar protection as the vaccine (which depends on the variant, see Shane, 2021) then, once again, reaching a level where the hospital infrastructure is not overwhelmed may be achieved without universal mandates, since the unvaccinated are at higher risk of contracting COVID-19 and developing natural immunity. And the COVID-19 vaccine immunity wanes over time, so reaching herd immunity is not the relevant policy goal for hospital capacity.
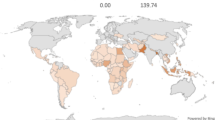
One last argument in favor of a universal mandate is that new mutations are mostly developed in unvaccinated populations or populations without high natural immunity (Niesen et al., 2021). While this may be true, we have argued that locating an externality is insufficient to justify countrywide vaccine mandates. To solve the problem of new mutations, a global vaccine mandate is required, which would be virtually impossible to enforce. Without the global mandate, the countrywide mandate is insufficient to prevent new mutations. Furthermore, in many countries across the world, especially low-income countries, the constraint is not the lack of a mandate but the lack of availability of the vaccine (Sheikh et al., 2021).
6 Divergent preferences versus free-riding
Our analysis so far has focused on situations in which people recognize an externality and then, depending on the nature of their collective interactions and the transaction costs involved, decide whether to take actions to internalize the externalities. Papers on optimal Pigouvian subsidies implicitly do the same thing.
We imagine these collective-action solutions as creating an incentive for people on the margin to take vaccines. For example, because each of the vaccines is relatively new, people are uncertain about the costs and benefits of getting them. For some, given the existing information on the vaccine, the expected private benefits outweigh the expected private costs. For others, the expected costs are greater, so they will not get the vaccine. As people learn more about the vaccines, if the experimental trials capture the costs and benefits, we expect more people to get the vaccine. The sort of institutional mechanisms that we discuss above can speed up this process.
In the case of the COVID-19 vaccines, there are distinct subsets of people who are unlikely to be persuaded by the mechanisms that we have highlighted so far. One group believes there is no infectious disease, and that COVID-19 is a conspiracy (see Ullah et al., 2021). Therefore, they do not consider the vaccine a desirable good because there is no negative externality from the infectious disease that needs to be overcome. Some believe that the vaccines contain mechanisms that allow government surveillance through microchips (see Berry et al., 2021). For these individuals, the vaccine is not a good but a private and social bad. More than just not getting vaccinated, these people will actively inhibit other people from getting vaccinated. For these groups, the question of underconsumption and optimal consumption is moot. For example, in January 2021, protesters forced a temporary shutdown of a vaccination site at Dodger Stadium (Gerber & Khan, 2021).
These are not people who would receive a vaccination if it was provided at zero or negative cost. They are not free-riding on other vaccinated individuals in the absence of a mandate. Unlike the examples in previous sections, transaction costs are not the reason that these people are not convinced to take the vaccine. If the optimal policy response required 100% vaccination, then to persuade COVID-19 deniers would require a very large Pigouvian subsidy to incentivize them to take the vaccine, and even that may not get society to 100% vaccination. In fact, for COVID-19 deniers and those who believe that the vaccine is a surveillance instrument, a mandate may be counterproductive, further strengthening the belief that the pandemic, or its cure, is a government conspiracy.
If people refuse to take the vaccine because of their unique beliefs and preferences, that is an entirely different problem than not taking the vaccine because they want to free-ride on others. Bridging divergent preferences is not an economic problem solved only using economic analysis. One must appeal to something else. Philosophers may be able to help.
There are also some who argue that misinformation is the chief cause of low rates of vaccination (Loomba et al., 2021; Pierri et al., 2021). This requires intervention in the form of an information campaign, quite different than a vaccine mandate. Communication experts and influencers may be more helpful than economists.
Bradley and Navin (2021), when talking about COVID-19, claim that it is incorrect to label vaccine refusers as free-riders because their beliefs and motivations may be different from free-riding. In practice, it may be impossible to disentangle non-vaccination because of free-riding from non-vaccination because of divergent preferences/beliefs. Either way, our main argument still holds. Since the reason for non-vaccination is unlikely to be free-riding, the economic case for universal vaccine mandates is weaker than commonly acknowledged.
Even in the case of COVID-19 deniers, most of the population will have immunity (for the short-term in the case of COVID-19) due to the vaccine or natural immunity protection before there is 100% vaccination in the community. Here, again, Buchanan and Stubblebine’s (1962) concept of inframarginal externalities matters. At a high-enough level of vaccination, the marginal externality disappears, and we only have an inframarginal externality. If the deniers and conspiracy theorists are not too numerous, their lack of vaccination does not generate a negative externality on the rest of the population. And this group will likely develop natural immunity after 2 years of the pandemic. Becchetti and Salustri (2021) find from survey data from Italy that around 21% of the population will not take the vaccine, regardless of new information arriving about its costs and benefits. The collective-action problem is about incentivizing those on the margin that are most open to the vaccine.
7 Conclusion
This paper started from the widely accepted premise by economists writing on vaccines, that vaccines generate a positive externality. The private and social marginal benefits of vaccines do not perfectly align creating room for policy interventions to improve outcomes for everyone involved. However, we argue that vaccine mandates, which are a common policy approach to the externality are weaker than commonly acknowledged in the case of COVID-19 vaccine.
We find that the presence of a positive externality does not automatically imply free-riding. In fact, most of the benefits for the vaccines developed to battle COVID-19 are internalized. This is because vaccinated individuals are protected from the most severe consequences of the infection, but they can transmit the infection, especially in the case of newer variants of the novel corona virus. In this sense, the externality is also partially excludable since asymptomatic vaccinated individuals may transmit to the unvaccinated. Given the strong private incentives to vaccinate, the externality may be inframarginal, as defined by Buchanan and Stubblebine (1962); that is, the externalities exist, but they are irrelevant to the policy.
Second, even when the effects are not completely internalized, the external benefits are more local than global. Family members infect each other. Coworkers infect each other. The policy response should reflect the level of the externality. Therefore, the case for universal vaccine mandates is weaker than often acknowledged within the economics literature. Local public goods allow for more sorting and local “production,” which, in this case, means local incentives to take the vaccine.
Finally, if the non-universal adoption of a COVID-19 vaccine is due to preferences and beliefs about the nature/existence of the virus, vaccine, the healthcare system, and government, then the argument is not based on free-riding. Policymakers must their argument in favor of mandates rooted in explanations other than free-riding.
The case for universal COVID-19 vaccine mandates is not strongly situated in explanations for underconsumption due to a free-rider problem. Nothing in our argument implies there is no role for governmental policy in vaccination. Instead, we maintain that the policy response should not singularly focus on universal vaccine mandates to solve a free-rider problem if none exists. There may be other reasons, not related to externalities and free-rider problems, but instead in politicization, misinformation, or paternalism, to justify vaccine mandates.
Notes
Data on counties and private players mandating vaccines have not been included in this compilation.
Of the remaining three, two have been stayed by court orders and one has been withdrawn after the US Supreme Court ruled that Congress had not granted such authority in National Federation of Independent Business v. Occupational Safety and Health Administration, 595 U.S. (2022) (per curiam).
See the Omnibus COVID-19 Health Care Staff Vaccination Rule (2021).
See the Department of Defense (2021).
See Presidential Proclamation 10,294 (White House, 2021a)
California, Colorado, Connecticut, Delaware, Guam, Hawaii, Illinois, Maine, Maryland, Massachusetts, Minnesota, New Jersey, New Mexico, New York, Oregon, Pennsylvania, Puerto Rico, Rhode Island, Vermont and Washington.
Aquinnah, Boston, Chicago, Denver, District of Columbia, Hoboken, Jackson, King County, Los Angeles, New Bedford, New Orleans, New York City, Newark, Pasadena, Philadelphia, Portland (Oregon), Providence, Richmond (Virginia), Sacramento, San Diego, San Francisco, San Jose, Seattle, St. Louis and Tucson.
Australia, Austria, Bulgaria, Canada, China, Costa Rica, Croatia, Czech Republic, Denmark, Ecuador, Egypt, Fiji, Finland, France, Germany, Ghana, Greece, Hungary, Indonesia, Italy, Kenya, Kuwait, Latvia, Lebanon, Malaysia, Micronesia, Morocco, Netherlands, New Zealand, Oman, Philippines, Poland, Romania, Russia, Saudi Arabia, Serbia, Singapore, South Korea, Sweden, Switzerland, Tajikistan, Tunisia, Turkey, Turkmenistan, Ukraine, and United Kingdom. Ours is not an exhaustive list but based on information available on the vaccine plans of different countries. (Reuters, 2021).
Buchanan and Stubblebine (1962) distinguish between inframarginal and Pareto-irrelevant externalities, a distinction that turns on whether one considers only marginal changes or allows for discrete changes in people’s actions. That is an important theoretical distinction, but not important for the applications in this paper.
References
Ahuja, A., Athey S., Baker, A., Budish, E., Castillo, J. C., Glennerster, R., Kominers, S. C., Kremer, M., Lee, J., Prendergast, C., Snyder, C. M., Tabarrok, A., Tan, B. J., & Wiccek, W. (2021). Preparing for a pandemic: Accelerating vaccine availability. AEA Papers and Proceedings, 111, 331–335. https://doi.org/10.1257/pandp.20211103
Amanna, I., & Slifka, M. (2020). Successful vaccines. In L. Hangartner & D. Burton (Eds.), Vaccination strategies against highly variable pathogens (pp. 1–30). Springer.
Araf, Y., Akter, F., Tang, Y., Fatemi, R., Parvez, Md. S. A., Zheng, C., & Hossain, Md. G. (2022). Omicron variant of SARS-CoV-2: Genomics, transmissibility, and responses to current COVID-19 vaccines. Journal of Medical Virology, 94(5), 1825–1832.
Becchetti, L., & Salustri, F. (2021). Optimal policies for vaccine campaign: The case of COVID-19. Working Paper. https://doi.org/10.2139/ssrn.3760388
Berry, S. D., et al. (2021). Lessons learned from frontline skilled nursing facility staff regarding COVID-19 vaccine hesitancy. Journal of the American Geriatrics Society, 69(5), 1140–1146.
Bradley, E., & Navin, M. (2021). Vaccine refusal is not free-riding. Erasmus Journal for Philosophy and Economics, 14(1), 167–181.
Browne, K. (2016). The measles and free-riders: California’s mandatory vaccination law. Cambridge Quarterly of Healthcare Ethics, 25(3), 472–478.
Buchanan, J. M. (1965). An economic theory of clubs. Economica, 32(125), 1. https://doi.org/10.2307/2552442
Buchanan, J. M., & Stubblebine, W. C. (1962). Externality in classic papers in natural resource economics (pp. 138–154). Palgrave Macmillan.
Buttenheim, A. M., & Asch, D. A. (2013). Making vaccine refusal less of a free-ride. Human Vaccines & Immunotherapeutics, 9(12), 2674–2675.
Center for Disease Control and Prevention [CDC]. (2022c). Risk for COVID-19 infection, hospitalization, and death by age group. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-age.html. Retrieved from March 25, 2022c.
Center for Disease Control and Prevention [CDC]. (2022b). People with certain medical conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Retrieved from March 25, 2022b.
Center for Disease Control and Prevention [CDC]. (2022a). How CDC is making COVID-19 vaccine recommendations. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations-process.html. Retrieved from March 25, 2022a.
Coase, R. H. (1960). The problem of social cost, The. Journal of Law & Economics, 3, 1–44.
Cowen, T. (1985). Public goods definitions and their institutional context: A critique of public goods theory. Review of Social Economy, 43(1), 53–63. https://doi.org/10.1080/00346768500000020
Cowen, T. (2002). Public goods and externalities. In D. Hendersion (Ed.), The concise encyclopedia of economics. Liberty Fund.
Demsetz, H. (1967). Toward a theory of property rights. American Economic Review, 57(2), 347–359.
Department of Defense. (2021, August 24). Mandatory Coronavirus Disease 2019 Vaccination of Department of Defense Service Members. Retrieved from, https://media.defense.gov/2021/Aug/25/2002838826/-1/-1/0/MEMORANDUM-FOR-MANDATORY-CORONAVIRUS-DISEASE-2019-VACCINATION-OF-DEPARTMENT-OF-DEFENSE-SERVICE-MEMBERS.PDF
Dickler, J. (2021). Free with Covid vaccine: Krispy Kreme, marijuana, beer and more. CNBC, 31 March. https://www.cnbc.com/2021/03/31/free-with-covid-vaccine-krispy-kreme-marijuana-beer-and-more.html. Retrieved from March 25, 2022.
Egan, M. (2020). Major CEOs signal Covid vaccine mandates could be on the way. CNN Business, 16 December. https://www.cnn.com/2020/12/16/business/ceos-covid-vaccine-mandate/index.html. Retrieved from March 25, 2022.
Elassar, A. (2021). A Michigan marijuana dispensary is offering a free joint to anyone who gets a Covid-19 vaccine. CNN, 23 January. https://edition.cnn.com/2021/01/23/us/michigan-marijuana-free-weed-vaccine-trnd/index.html. Retrieved from March 25, 2022.
Eyre, D. W., et al. (2022). Effect of Covid-19 vaccination on transmission of alpha and delta variants. The New England Journal of Medicine, 386(8), 744–756.
Flanigan, J. (2014). A defense of compulsory vaccination. HEC Forum, 26(1), 5–25.
Francis, P. J. (2004). Optimal tax/subsidy combinations for the flu season. Journal of Economic Dynamics & Control, 28(10), 2037–2054.
Gerber, M., & Khan, I. (2021). Dodger Stadium vaccination site shut down amid protest—Los Angeles Times. The Los Angeles times, 30 January. https://www.latimes.com/california/story/2021-01-30/dodger-stadiums-covid-19-vaccination-site-shutdown-after-dozens-of-protesters-gather-at-entrance. Retrieved from March 25, 2022.
Giubilini, A. (2020). An argument for compulsory vaccination: The taxation analogy. Journal of Applied Philosophy, 37(3), 446–466.
Giurgea, L. T., Morens, D. M., & Yount, J. (2022). Great expectations of COVID-19 herd immunity. mBio 13(1), e03495–21. https://doi.org/10.1128/mbio.03495-21
Goodkin-Gold, M., et al. (2020). Optimal vaccine subsidies for endemic and epidemic diseases. National Bureau of Economic Research Working Paper 28085.
Gostin, L. O., Salmon, D. A., & Larson, H. J. (2021). Mandating COVID-19 vaccines. The Journal of the American Medical Association, 325(6), 532–533.
Holland, M. S., & Zachary, C. E. (2014). Herd immunity and compulsory childhood vaccination: Does the theory justify the law? Oregon Law Review, 93(1), 1–48.
Howard, J. (2021). All 50 states now have expanded or will expand Covid vaccine eligibility to everyone 16 and up. CNN. https://edition.cnn.com/2021/03/30/health/states-covid-19-vaccine-eligibility-bn/index.html. Retrieved from March 25, 2022.
IGM Forum. (2015). Vaccines: A survey, March 10. https://www.igmchicago.org/surveys/vaccines/. Retrieved from March 25, 2022.
Johnson, E. B., Tidwell, A., & Villupuram, S. V. (2020). Valuing curb appeal. Journal of Real Estate Finance and Economics, 60(1–2), 111–133. https://doi.org/10.1007/s11146-019-09713-z
Kennedy, A. M., & Gust, D. A. (2008). Measles outbreak associated with a church congregation: A study of immunization attitudes of congregation members. Public Health Reports, 123(2), 126–134. https://doi.org/10.2139/ssrn.3571437
Kremer, M., Levin, J., & Snyder, C. M. (2020). Advance market commitments: Insights from theory and experience. AEA Papers and Proceedings, 110, 269–273.
Kroger. (2021). Kroger announces new vaccine payment for all associates. 5 February. http://ir.kroger.com/CorporateProfile/press-releases/press-release/2021/Kroger-Announces-New-Vaccine-Payment-for-All-Associates/default.aspx. Retrieved from March 25, 2022.
Leeson, P. T., & Rouanet, L. (2021). Externality and COVID-19. Southern Economic Journal, 87(4), 1107–1118.
Leeson, P. T., & Thompson, H. A. (2021). Public choice and public health. Public Choice. https://doi.org/10.1007/s11127-021-00900-2
Lieberman, J. M., et al. (2006). The safety and immunogenicity of a quadrivalent measles, mumps, Rubella and varicella vaccine in healthy children: A study of manufacturing consistency and persistence of antibody. The Pediatric Infectious Disease Journal, 25(7), 615–622.
Loomba, S., et al. (2021). Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nature Human Behaviour, 5(3), 337–348.
Lu, L., et al. (2022). Neutralization of severe acute respiratory syndrome coronavirus 2 omicron variant by sera from BNT162b2 or CoronaVac vaccine recipients. Clinical Infectious Diseases, 75(1), e822–e826.
Mathieu, E., & Roser, M. (2021). How do death rates from COVID-19 differ between people who are vaccinated and those who are not? Our World in Data, November 23. https://ourworldindata.org/covid-deaths-by-vaccination. Retrieved from March 25, 2022.
McKillop, C. N., et al. (2019). Do traditional economic theories of free-riding behavior explain spatial clustering of HPV vaccine uptake? SSM - Population Health, 8, 100421.
Miller, C. (2021). Trader Joe’s, Dollar General and others are paying workers to get vaccines. NPR, January 21. https://www.npr.org/2021/01/21/958849642/grocers-have-a-strategy-to-get-their-workers-vaccinated-against-covid-19-pay-the. Retrieved from March 25, 2022.
Moghadas, S. M., Vilches, T. N., Zhang, K., Wells, C. R., Shoukat, A., Singer, B. H., Meyers, L. A., Neuzil, K. M., Langley, J. M., Fitzpatrick, M. C., & Galvani, A. P. (2021). The impact of vaccination on coronavirus disease 2019 (COVID-19) outbreaks in the United States. Clinical Infectious Diseases, 73(12), 2257–2264.
Mulligan, C. (2021). The backward art of slowing the spread? Congregation efficiencies during COVID-19. National Bureau of Economic Research Working Paper 28737.
National Federation of Independent Business v. Occupational Safety and Health Administration, 595 U.S. (2022). (per curiam).
New York Times. (2022). Coronavirus in the U.S.: Latest map and case counts. https://www.nytimes.com/interactive/2021/us/covid-cases.html. Retrieved from March 25, 2022.
Niesen, M. J. M., Anand, P., Silvert, E., Suratekar, R., Pawlowski, C., Ghosh, P., Lenehan, P., Hughes, T., Zemmour, D., O’Horo, J. C., Yao, J. D., Pritt, B. S., Norgan, A., Hurt, R. T., Badley, A. D., Venkatakrishnan, A. J., & Soundararajan, V. (2021). COVID-19 vaccines dampen genomic diversity of SARS-CoV-2: Unvaccinated patients exhibit more antigenic mutational variance. MedRxiv. https://doi.org/10.1101/2021.07.01.21259833
Omnibus COVID-19 Health Care Staff Vaccination Rule; Centers for Medicare & Medicaid Services (CMS), HHS. (2021). 86 Fed. Reg. 61555. https://www.federalregister.gov/documents/2021/11/05/2021-23831/medicare-and-medicaid-programs-omnibus-covid-19-health-care-staff-vaccination. Retrieved from September 7, 2022.
Patra, K. (2021). NFL informs clubs that COVID-19 outbreaks among unvaccinated players could lead to forfeited games. NFL, 22 July. https://www.nfl.com/news/nfl-covid-19-outbreaks-unvaccinated-players-forfeit-cancelled-game. Retrieved from March 25, 2022.
Pierri, F., et al. (2021). The impact of online misinformation on U.S. COVID-19 vaccinations. arXiv preprint, https://doi.org/10.48550/ARXIV.2104.10635.
Reuters. (2021). Factbox: Countries making COVID-19 vaccines mandatory, 31 December. https://www.reuters.com/business/healthcare-pharmaceuticals/countries-making-covid-19-vaccines-mandatory-2021-08-16/. Retrieved from March 25, 2022).
Scobie, H. M., Johnson, A. G., Suthar, A. B., et al. (2021). Monitoring incidence of COVID-19 cases, hospitalizations, and deaths, by vaccination status—13 U.S. jurisdictions, April 4–July 17, 2021. Morbidity and Mortality Weekly Report, 70, 1284–1290. https://doi.org/10.15585/mmwr.mm7037e1
Shalby, C. et al. (2020). Some healthcare workers refuse to take COVID-19 vaccine, even with priority access. The Los Angeles Times, 31 December. https://www.latimes.com/california/story/2020-12-31/healthcare-workers-refuse-covid-19-vaccine-access. Retrieved from March 25, 2022.
Shane, C. (2021). Hybrid immunity. Science, 372(6549), 1392–1393.
Sheikh, A. B., Pal, S., Javed, N., & Shekhar, R. (2021). COVID-19 vaccination in developing nations: Challenges and opportunities for innovation. Infectious Disease Reports, 13(2), 429–436. MDPI AG.
Shoag, D., & Veuger, S. (2018). Shops and the city: Evidence on local externalities and local government policy from big-box bankruptcies. The Review of Economics and Statistics, 100(3), 440–453. https://doi.org/10.1162/rest_a_00703
Stiglitz, J. E. (2000). Economics of the public sector (3rd ed.). WW Norton.
Stiglitz, J. E. (2021). COVID-19 and human freedom. Project Syndicate, 7 September. https://www.project-syndicate.org/commentary/covid19-spike-in-us-reflects-misunderstanding-of-liberty-by-joseph-e-stiglitz-2021-09. Retrieved from March 25, 2022.
Tabarrok, A. T. (2020). Grand innovation prizes to address pandemics: A primer. Working paper. https://doi.org/10.2139/ssrn.3571437
Thomas, G. (2020). Singapore Airlines trials new digital health passport. Airline Ratings, 27 December. https://www.airlineratings.com/news/singapore-airlines-trials-new-digital-health-passport/. Retrieved from March 25, 2022.
Tiebout, C. M. (1956). A pure theory of local expenditures. Journal of Political Economy, 64(5), 416–424.
Tyko, K. (2021). Free beer for COVID vaccine: Samuel Adams announces incentive on National Beer Day and how to get free Coors Pure. USA Today, 7 April. https://www.usatoday.com/story/money/food/2021/04/07/national-beer-day-sam-adams-covid-vaccine-incentive-free-beer/7108414002/. Retrieved from March 25, 2022.
Ullah, I., et al. (2021). Myths and conspiracy theories on vaccines and COVID-19: Potential effect on global vaccine refusals. Vacunas, 22(2), 93–97.
van den Hoven, M. (2012). Why one should do one’s bit: Thinking about free-riding in the context of public health ethics. Public Health Ethics, 5(2), 154–160.
White House. (2021b). Fact sheet: Biden administration announces details of two major vaccination policies, 4 November. https://www.whitehouse.gov/briefing-room/statements-releases/2021b/11/04/fact-sheet-biden-administration-announces-details-of-two-major-vaccination-policies/. Retrieved from March 25, 2022.
White House. (2021a). A proclamation on advancing the safe resumption of global travel during the COVID-19 pandemic. 31 October. https://www.whitehouse.gov/briefing-room/presidential-actions/2021a/10/25/a-proclamation-on-advancing-the-safe-resumption-of-global-travel-during-the-covid-19-pandemic/. Retrieved from September 7, 2022.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Albrecht, B.C., Rajagopalan, S. Inframarginal externalities: COVID-19, vaccines, and universal mandates. Public Choice 195, 55–72 (2023). https://doi.org/10.1007/s11127-022-01006-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11127-022-01006-z
Keywords
- Externality
- Inframarginal externality
- Underconsumption
- Free-rider problem
- Vaccines
- Universal vaccine mandates
- COVID-19