Abstract
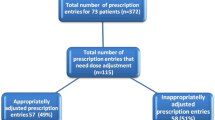
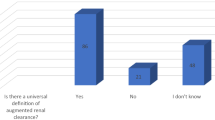
Background Renal dosage adjustment for patients with reduced kidney function is a common function of clinical pharmacy service. Assessment of pharmacist’s intervention in the aspect of quality and economic impact should be conducted to evaluate the benefit of this service. Objective This study aimed to assess the quality and cost saving of clinical pharmacists’ recommendation on renal dosage adjustment among patients with reduced kidney function. Setting Eight medical wards of the Siriraj Hospital, a tertiary-care hospital in Bangkok, Thailand. Method A retrospective study was conducted using medical records and clinical pharmacist’s intervention database. All patients admitted to the study wards whose estimated creatinine clearance were less than 60 mL/min or presented with acute kidney injury on admission during October 2016–December 2017 were included. The targeted medications were antimicrobial agents. Main outcome measure Percentage of the concordance between pharmacists’ recommendation compared to standard dosing references and related cost saving. Results Among 158 patients, pharmacists provided 190 recommendations, including 151 (79.1%) dose reduction, 17 (8.9%) dose increase and 22 (11.5%) recommendations to provide supplemental dose after dialysis. These recommendations were 90.5% consistent with standard references. Physician accepted and complied with 89.5% of pharmacists’ recommendations. Average direct cost saving was €5,114.11 while cost avoidance was €863.47. Conclusion Trained clinical pharmacists were able to provide high-quality recommendation on dosage adjustment in these patients in accordance to standard dosing guidelines. In addition, dosage adjustment also led to a significant direct cost saving and cost avoidance from prevention of adverse drug reactions.


Similar content being viewed by others
References
Hill NR, Fatoba ST, Oke JL, Hirst JA, O'Callaghan CA, Lasserson DS, et al. Global prevalence of chronic kidney disease—a systematic review and meta-analysis. PLoS ONE. 2016;11:e0158765.
Stanifer JW, Muiru A, Jafar TH, Patel UD. Chronic kidney disease in low- and middle-income countries. Nephrol Dial Transpl. 2016;31:868–74.
Mills KT, Xu Y, Zhang W, Bundy JD, Chen CS, Kelly TN, et al. A systematic analysis of worldwide population-based data on the global burden of chronic kidney disease in 2010. Kidney Int. 2015;88:950–7.
Ingsathit A, Thakkinstian A, Chaiprasert A, Sangthawan P, Gojaseni P, Kiattisunthorn K, et al. Prevalence and risk factors of chronic kidney disease in the Thai adult population: Thai SEEK study. Nephrol Dial Transpl. 2010;25:1567–75.
Susantitaphong P, Cruz DN, Cerda J, Abulfaraj M, Alqahtani F, Koulouridis I, et al. World incidence of AKI: a meta-analysis. Clin J Am Soc Nephrol. 2013;8:1482–93.
Srisawat N, Kulvichit W, Mahamitra N, Hurst C, Praditpornsilpa K, Lumlertgul N, et al. The epidemiology and characteristics of acute kidney injury in the Southeast Asia intensive care unit: a prospective multicentre study. Nephrol Dial Transpl. 2019. https://doi.org/10.1093/ndt/gfz087.
Matzke GR, Dowling TC, Marks SA, Murphy JE. Influence of kidney disease on drug disposition: an assessment of industry studies submitted to the FDA for new chemical entities 1999–2010. J Clin Pharmacol. 2016;56:390–8.
Dowling TC, Matzke GR, Murphy JE, Burckart GJ. Evaluation of renal drug dosing: prescribing information and clinical pharmacist approaches. Pharmacotherapy. 2010;30:776–86.
Tully MP, Buchan IE. Prescribing errors during hospital inpatient care: factors influencing identification by pharmacists. Pharm World Sci. 2009;31:682–8.
Manley HJ, McClaran ML, Overbay DK, Wright MA, Reid GM, Bender WL, et al. Factors associated with medication-related problems in ambulatory hemodialysis patients. Am J Kidney Dis. 2003;41:386–93.
Grabe DW, Low CL, Bailie GR, Eisele G. Evaluation of drug-related problems in an outpatient hemodialysis unit and the impact of a clinical pharmacist. Clin Nephrol. 1997;47:117–21.
Saad R, Hallit S, Chahine B. Evaluation of renal drug dosing adjustment in chronic kidney disease patients at two university hospitals in Lebanon. Pharm Pract (Granada). 2019;17:1304.
Fink JC, Chertow GM. Medication errors in chronic kidney disease: one piece in the patient safety puzzle. Kidney Int. 2009;76:1123–5.
Drenth-van Maanen AC, van Marum RJ, Jansen PA, Zwart JE, van Solinge WW, Egberts TC. Adherence with dosing guideline in patients with impaired renal function at hospital discharge. PLoS ONE. 2015;10:e0128237.
Falconnier AD, Haefeli WE, Schoenenberger RA, Surber C, Martin-Facklam M. Drug dosage in patients with renal failure optimized by immediate concurrent feedback. J Gen Intern Med. 2001;16:369–75.
Hassan Y, Al-Ramahi RJ, Aziz NA, Ghazali R. Impact of a renal drug dosing service on dose adjustment in hospitalized patients with chronic kidney disease. Ann Pharmacother. 2009;43:1598–605.
MICROMEDEX [Internet]. Truven health analytics. https://www.micromedexsolutions.com. Accessed 12 Aug 2018.
Aronoff GR, Berns JS, Brier ME, Kasbekar N, Mueller BA, et al. Drug prescribing in renal failure. 5th ed. Philadelphia: American College of Physicians; 2007. p. 272.
Gilbert DNCH, Eliopoulos GM, Saag MS, Pavia AT, Black D, et al. The Sanford guide to antimicrobial therapy 2016. 46th ed. Sperryville, VA: Antimicrobial Therapy, Inc.; 2016. p. 254.
Thai Association for the Study of the Liver. Thailand practice guideline for management of chronic hepatitis B and C. 1st ed. Bangkok: Parbpim Ltd.; 2015. p. 74.
Chuang LC, Sutton JD, Henderson GT. Impact of a clinical pharmacist on cost saving and cost avoidance in drug therapy in an intensive care unit. Hosp Pharm. 1994;29(215–8):21.
Riewpaiboon A. Standard cost lists for health economic evaluation in Thailand. J Med Assoc Thai. 2014;97(Suppl 5):S127–S134134.
Shields RK, Anand R, Clarke LG, Paronish JA, Weirich M, Perone H, et al. Defining the incidence and risk factors of colistin-induced acute kidney injury by KDIGO criteria. PLoS ONE. 2017;12:e0173286.
Oliveira JF, Silva CA, Barbieri CD, Oliveira GM, Zanetta DM, Burdmann EA. Prevalence and risk factors for aminoglycoside nephrotoxicity in intensive care units. Antimicrob Agents Chemother. 2009;53:2887–911.
Norrby SR. Side effects of cephalosporins. Drugs. 1987;34(Suppl 2):105–20.
Kohno S, Yamaguchi K, Aikawa N, Sumiyama Y, Odagiri S, Aoki N, et al. Linezolid versus vancomycin for the treatment of infections caused by methicillin-resistant Staphylococcus aureus in Japan. J Antimicrob Chemother. 2007;60:1361–9.
Hassan Y, Al-Ramahi RJ, Aziz NA, Ghazali R. Adverse drug events in hospitalized patients with chronic kidney disease. Int J Clin Pharmacol Ther. 2010;48:571–6.
Hassan Y, Al-Ramahi R, Abd Aziz N, Ghazali R. Drug use and dosing in chronic kidney disease. Ann Acad Med Singap. 2009;38:1095–103.
AbuRuz SM, Alrashdan Y, Jarab A, Jaber D, Alawwa IA. Evaluation of the impact of pharmaceutical care service on hospitalized patients with chronic kidney disease in Jordan. Int J Clin Pharm. 2013;35:780–9.
Arrabal-Duran P, Duran-Garcia ME, Ribed-Sanchez A, Hidalgo-Collazos P, Sanjurjo-Saez M. Pharmaceutical interventions in prescriptions for patients admitted with chronic renal failure. Nefrologia. 2014;34:710–5.
Saengpeng A, Saramunee K, Anusornsangiam W. Development of dosage adjustment system for in-patients with renal impairment at Prasat Hospital, Surin Province. Thai J Pharm Pract. 2017;9:281–91.
Thanasermsuay W. The effects of pharmacist's intervention on dosage adjustment for patients with renal insufficiency at the medical wards of Ramathibodi Hospital [master thesis]. Bangkok: Mahidol University; 2549.
Cabello-Muriel A, Gascon-Canovas JJ, Urbieta-Sanz E, Iniesta-Navalon C. Effectiveness of pharmacist intervention in patients with chronic kidney disease. Int J Clin Pharm. 2014;36:896–903.
Barnes KD, Tayal NH, Lehman AM, Beatty SJ. Pharmacist-driven renal medication dosing intervention in a primary care patient-centered medical home. Pharmacotherapy. 2014;34:1330–5.
Thai Food and Drug Administration. Drug situation, medication and health care cost. https://ndi.fda.moph.go.th/uploads/policy_file/20170801151423.pdf.
Acknowledgements
All authors would like to thank the medical ward pharmacist team, physicians, residents, fellows, nurses, administrators and other supporting personnel of the medical wards at Siriraj Hospital for their contribution to this project.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
All authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sukkha, S., Rattanavipanon, W., Chamroenwit, B. et al. Quality assessment and cost saving of renal dosing recommendation by clinical pharmacists at medical wards in Thailand. Int J Clin Pharm 42, 610–616 (2020). https://doi.org/10.1007/s11096-020-01016-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-020-01016-1