Abstract
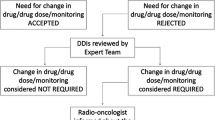
Objectives To evaluate the type, frequency, severity and predictors of potential Drug-Drug Interactions (DDIs) in a cohort of patients undergoing radiodiagnostic procedures. Setting Eight Radiology wards located in Tuscany (Italy). Methods All participants exposed to at least two medications were included in the analysis. DDIs were grouped according to their severity as ‘minor’, ‘moderate’ or ‘major’. A logistic model was used to estimate Odds Ratios and 95% Confidence Intervals for all predictors of potential DDI. Main outcome measures Type and predictors of potential DDI in a cohort of patients undergoing radiodiagnostic procedures. Results One-thousand-and-two subjects (57.6% females; mean age: 67.3 ± 12.2) entered the analysis, and 46.1% of them incurred in a potential DDI (78.9% ‘moderate’ in severity). The combination of allopurinol and ACE-inhibitors was the most frequent (21/153) among major potential DDIs, while steroids were involved in all cases of potential DDI due to premedication. Co-morbidity, number of co-medications, advanced age and premedication use increased the risk of potential DDI; a protective role was found for positive history of allergy. When the analysis was restricted to subjects with premedication (n = 93), only 12.9% of them reported a potential DDI directly attributable to premedication drugs. Conclusions Among patients undergoing radiological examination, types and predictors of potential DDIs appeared in agreement with other kind of in-hospital populations. Premedication revealed to be a proxy predictor for potential DDIs. Considering the poor capability of the prescriber in recognizing interactions, their systematic evaluation (using an informatics tool) in patients undergoing radiological examination might be helpful in preventing the occurrence of clinically relevant DDIs.




Similar content being viewed by others
References
McLean AJ, Le Couteur DG. Aging biology and geriatric clinical pharmacology. Pharmacol Rev. 2004;56:163–84.
Johnell K, Klarin I. The relationship between number of drugs and potential drug–drug interactions in the elderly: a study of over 600,000 elderly patients from the Swedish prescribed drug register. Drug Saf. 2007;30:911–8.
Juurlink DN, Mamdani M, Kopp A, Laupacis A, Redelmeier DA. Drug–drug interactions among elderly patients hospitalized for drug toxicity. JAMA. 2003;289:1652–8.
McDonnell PJ, Jacobs MR. Hospital admissions resulting from preventable adverse drug reactions. Ann Pharmacother. 2002;36:1331–6.
Peyriere H, Cassan S, Floutard E, Riviere S, Blayac JP, Hillaire-Buys D, et al. Adverse drug events associated with hospital admission. Ann Pharmacother. 2003;37:5–11.
Pirmohamed M, James S, Meakin S, Green C, Scott AK, Walley TJ, et al. Adverse drug reactions as cause of admission to hospital: prospective analysis of 18,820 patients. BMJ. 2004;329:15–9.
Gagne JJ, Maio V, Rabinowitz C. Prevalence and predictors of potential drug–drug interactions in Regione Emilia-Romagna, Italy. J Clin Pharm Ther. 2008;33:141–51.
Galatti L, Mazzaglia G, Greco A, Sessa E, Cricelli C, Schito GC, et al. Co-prescriptions with itraconazole and fluconazole as a signal for possible risk of drug-drug interactions: a four-year analysis from Italian general practice. Pharmacoepidemiol Drug Saf. 2007;16:422–8.
Magro L, Conforti A, Del Zotti F, Leone R, Iorio ML, Meneghelli I, et al. Identification of severe potential drug-drug interactions using an Italian general-practitioner database. Eur J Clin Pharmacol. 2008;64:303–9.
Thomsen HS. European Society of Urogenital Radiology (ESUR) guidelines on the safe use of iodinated contrast media. Eur J Radiol. 2006;60:307–13.
Lapi F, Cecchi E, Pedone C, Attanasio F, Banchelli G, Vannacci A, et al. Safety aspects of iodinated contrast media related to their physicochemical properties: a pharmacoepidemiology study in two Tuscany hospitals. Eur J Clin Pharmacol. 2008;64:723–37.
Micromedex(R). Micromedex-DRUGREAX. http://www.thomsonhc.com. Accessed February 2008.
Vonbach P, Dubied A, Beer JH, Krahenbuhl S. Recognition and management of potential drug-drug interactions in patients on internal medicine wards. Eur J Clin Pharmacol. 2007;63:1075–83.
Vonbach P, Dubied A, Krahenbuhl S, Beer JH. Evaluation of frequently used drug interaction screening programs. Pharm World Sci. 2008;30:367–74.
Langdorf MI, Fox JC, Marwah RS, Montague BJ, Hart MM. Physician versus computer knowledge of potential drug interactions in the emergency department. Acad Emerg Med. 2000;7:1321–9.
Rothman KJ, Greenland S. Types of epidemiology study. In: Rothman KJ, Greenland S, editors. Modern Epidemiology. Philadelphia: Lippincott Williams & Wilkins; 1998. p. 75–6.
Tulner LR, Frankfort SV, Gijsen GJ, van Campen JP, Koks CH, Beijnen JH. Drug–drug interactions in a geriatric outpatient cohort: prevalence and relevance. Drugs Aging. 2008;25:343–55.
Malone DC, Abarca J, Hansten PD, Grizzle AJ, Armstrong EP, Van Bergen RC et al. Identification of serious drug-drug interactions: results of the partnership to prevent drug-drug interactions. J Am Pharm Assoc (2003) 2004;44:142-51.
Cruciol-Souza JM, Thomson JC. Prevalence of potential drug-drug interactions and its associated factors in a Brazilian teaching hospital. J Pharm Pharm Sci. 2006;9:427–33.
Tramer MR, von Elm E, Loubeyre P, Hauser C. Pharmacological prevention of serious anaphylactic reactions due to iodinated contrast media: systematic review. BMJ. 2006;333:675.
Ko Y, Malone DC, Armstrong EP. Pharmacoeconomic evaluation of antimuscarinic agents for the treatment of overactive bladder. Pharmacotherapy. 2006;26:1694–702.
Paganini-Hill A, Ross RK. Reliability of recall of drug usage and other health-related information. Am J Epidemiol. 1982;116:114–22.
Glintborg B, Hillestrom PR, Olsen LH, Dalhoff KP, Poulsen HE. Are patients reliable when self-reporting medication use? Validation of structured drug interviews and home visits by drug analysis and prescription data in acutely hospitalized patients. J Clin Pharmacol. 2007;47:1440–9.
Solomon DH, Stedman M, Licari A, Weinblatt ME, Maher N, Shadick N. Agreement between patient report and medical record review for medications used for rheumatoid arthritis: the accuracy of self-reported medication information in patient registries. Arthritis Rheum. 2007;57:234–9.
Haukka J, Suvisaari J, Tuulio-Henriksson A, Lonnqvist J. High concordance between self-reported medication and official prescription database information. Eur J Clin Pharmacol. 2007;63:1069–74.
Skurtveit S, Selmer R, Tverdal A, Furu K. The validity of self-reported prescription medication use among adolescents varied by therapeutic class. J Clin Epidemiol. 2008;61:714–7.
Curtis JR, Westfall AO, Allison J, Freeman A, Kovac SH, Saag KG. Agreement and validity of pharmacy data versus self-report for use of osteoporosis medications among chronic glucocorticoid users. Pharmacoepidemiol Drug Saf. 2006;15:710–8.
Martin LM, Leff M, Calonge N, Garrett C, Nelson DE. Validation of self-reported chronic conditions and health services in a managed care population. Am J Prev Med. 2000;18:215–8.
Acknowledgements
We are very grateful to all pharmacists, radiologists and nurses who took part in the data collection.
Funding
This study was supported by a research grant from non-profit “Drug Education and Investigation (DEI) Foundation” (Italian Society of Pharmacology).
Conflicts of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lapi, F., Vietri, M., Moschini, M. et al. Potential drug–drug interactions and radiodiagnostic procedures: an in-hospital survey. Pharm World Sci 32, 200–205 (2010). https://doi.org/10.1007/s11096-010-9370-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-010-9370-4