Abstract
Purpose
Pulmonary antibiotic delivery is recommended as maintenance therapy for cystic fibrosis (CF) patients who experience chronic infections. However, abnormally thick and sticky mucus present in the respiratory tract of CF patients impairs mucus penetration and limits the efficacy of inhaled antibiotics. To overcome the obstacles of pulmonary antibiotic delivery, we have developed nanocomposite microparticles (nCmP) for the inhalation application of antibiotics in the form of dry powder aerosols.
Methods
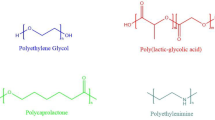
Azithromycin-loaded and rapamycin-loaded polymeric nanoparticles (NP) were prepared via nanoprecipitation and nCmP were prepared by spray drying and the physicochemical characteristics were evaluated.
Results
The nanoparticles were 200 nm in diameter both before loading into and after redispersion from nCmP. The NP exhibited smooth, spherical morphology and the nCmP were corrugated spheres about 1 μm in diameter. Both drugs were successfully encapsulated into the NP and were released in a sustained manner. The NP were successfully loaded into nCmP with favorable encapsulation efficacy. All materials were stable at manufacturing and storage conditions and nCmP were in an amorphous state after spray drying. nCmP demonstrated desirable aerosol dispersion characteristics, allowing them to deposit into the deep lung regions for effective drug delivery.
Conclusions
The described nCmP have the potential to overcome mucus-limited pulmonary delivery of antibiotics.






Similar content being viewed by others
Abbreviations
- Ac-Dex:
-
Acetalated dextran
- AZI:
-
Azithromycin
- CAC:
-
Cyclic-to-acyclic
- CDCl3 :
-
Deuterated chloroform
- CF:
-
Cystic fibrosis
- CFTR:
-
Cystic fibrosis transmembrane conductance regulator
- D2O:
-
Deuterium oxide
- DCC:
-
N,N′-dicyclohexyl- carbodiimde
- DCl:
-
Deuterium chloride
- DMAP:
-
4-(dimethylamino) pyridine
- ED:
-
Emitted dose
- EE:
-
Encapsulation efficiency
- FPD:
-
Fine particle dose
- FPF:
-
Fine particles fraction
- HPMC:
-
Hydroxypropyl methylcellulose
- KF:
-
Karl Fischer
- mPEG:
-
Poly(ethylene glycol) methyl ether
- nCmP:
-
Nanocomposite microparticles
- NGI:
-
Next Generation Impactor
- NP:
-
Nanoparticles
- PPTS:
-
P-toluenesulfonate
- PXRD:
-
Powder X-ray diffraction
- RAP:
-
Rapamycin
- RF:
-
Respirable fraction
- TEA:
-
2-methoxypropene (2-MOP), triethylamine
- VP5k:
-
poly(ethylene glycol) vitamin E
References
Bowenand S-J, Hull J. The basic science of cystic fibrosis. Paediatr Child Health. 2015;25:159–64.
Bradbury NA. Cystic Fibrosis. In: Bradshaw RA, Stahl PD, Gilbert A, editors. Encyclopedia of Cell Biology, 1st ed. Waltham; 2015. p 283–293.
Thursfieldand RM, Davies JC. Cystic Fibrosis: therapies targeting specific gene defects. Paediatr Respir Rev. 2012;13:215–9.
Chuchalin A, Amelina E, Bianco F. Tobramycin for inhalation in cystic fibrosis: beyond respiratory improvements. Pulm Pharmacol Ther. 2009;22:526–32.
Milla CE. Nutrition and lung disease in cystic fibrosis. Clin Chest Med. 2007;28:319–30.
FibrosisFoundation C. Patient registry 2005 annual report. Maryland: Bethesda; 2005.
Heijerman H, Westerman E, Conway S, Touw D. Inhaled medication and inhalation devices for lung disease in patients with cystic fibrosis: a European consensus. J Cyst Fibros. 2009;8:295–315.
Rajan S, Saiman L. Pulmonary infections in patients with cystic fibrosis. Semin Respir Infect. 2002;17:47–56.
Regelmann WE, Elliott GR, Warwick WJ, Clawson CC. Reduction of sputum pseudomonas aeruginosa density by antibiotics improves lung function in cystic fibrosis more than Do bronchodilators and chest physiotherapy alone. Am Rev Respir Dis. 1990;141:914–21.
Wagner T, Soong G, Sokol S, Saiman L, Prince A. EFfects of azithromycin on clinical isolates of pseudomonas aeruginosa from cystic fibrosis patients. Chest. 2005;128:912–9.
Southernand KW, Barker PM. Azithromycin for cystic fibrosis. Eur Respir J. 2004;24:834–8.
Saiman L, Marshall BC, Mayer-Hamblett N, et al. Azithromycin in patients with cystic fibrosis chronically infected with pseudomonas aeruginosa: A randomized controlled trial. JAMA. 2003;290:1749–56.
Wilms EB, Touw DJ, Heijerman HGM, van der Ent CK. Azithromycin maintenance therapy in patients with cystic fibrosis: A dose advice based on a review of pharmacokinetics, efficacy, and side effects. Pediatr Pulmonol. 2012;47:658–65.
Piscitalle SC, Danziger LH, Rodvold KA. Clarithromycin and azithromycin: new macrolide antibiotics. Clin Pharmacol. 1992;11:137–52.
Zhao M, You Y, Ren Y, Zhang Y, Tang X. Formulation, characteristics and aerosolization performance of azithromycin DPI prepared by spray-drying. Powder Technol. 2008;187:214–21.
Abdulrahman BA, Khweek AA, Akhter A, Caution K, Kotrange S, Abdelaziz DHA, et al. Autophagy stimulation by rapamycin suppresses lung inflammation and infection by Burkholderia cenocepacia in a model of cystic fibrosis. Autophagy. 2011;7:1359–70.
Chen Y-C, Lo C-L, Lin Y-F, Hsiue G-H. Rapamycin encapsulated in dual-responsive micelles for cancer therapy. Biomaterials. 2013;34:1115–27.
Broaders KE, Cohen JA, Beaudette TT, Bachelder EM, Frechet JMJ. Acetalated dextran is a chemically and biologically tunable material for particulate immunotherapy. Proc Natl Acad Sci U S A. 2009;106:5497–502.
Cook RO, Pannu RK, Kellaway IW. Novel sustained release microspheres for pulmonary drug delivery. J Control Release. 2005;104:79–90.
Kauffman KJ, Kanthamneni N, Meenach SA, Pierson BC, Bachelder EM, Ainslie KM. Optimization of rapamycin-loaded acetalated dextran microparticles for immunosuppression. Int J Pharm. 2012;422:356–63.
Broaders KE, Cohen JA, Beaudette TT, Bachelder EM, Fréchet JMJ. Acetalated dextran is a chemically and biologically tunable material for particulate immunotherapy. Proc Natl Acad Sci. 2009;106:5497–502.
Bachelder EM, Beaudette TT, Broaders KE, Dashe J, Fréchet JMJ. Acetal-derivatized dextran: an acid-responsive biodegradable material for therapeutic applications. J Am Chem Soc. 2008;130:10494–5.
Sham JOH, Zhang Y, Finlay WH, Roa WH, Löbenberg R. Formulation and characterization of spray-dried powders containing nanoparticles for aerosol delivery to the lung. Int J Pharm. 2004;269:457–67.
Ong HX, Traini D, Ballerin G, Morgan L, Buddle L, Scalia S, et al. Combined inhaled salbutamol and mannitol therapy for mucus hyper-secretion in pulmonary diseases. AAPS J. 2014;16:269–80.
Jensen DMK, Cun D, Maltesen MJ, Frokjaer S, Nielsen HM, Foged C. Spray drying of siRNA-containing PLGA nanoparticles intended for inhalation. J Control Release. 2010;142:138–45.
Littringer EM, Mescher A, Schroettner H, Achelis L, Walzel P, Urbanetz NA. Spray dried mannitol carrier particles with tailored surface properties – The influence of carrier surface roughness and shape. Eur J Pharm Biopharm. 2012;82:194–204.
Cooney GF, Lum BL, Tomaselli M, Fiel SB. Absolute bioavailability and absorption characteristics of aerosolized tobramycin in adults with cystic fibrosis. J Clin Pharmacol. 1994;34:255–9.
Hoppentocht M, Hagedoorn P, Frijlink HW, de Boer AH. Developments and strategies for inhaled antibiotic drugs in tuberculosis therapy: A critical evaluation. Eur J Pharm Biopharm. 2014;86:23–30.
Stanojevic S, Waters V, Mathew JL, Taylor L, Ratjen F. Effectiveness of inhaled tobramycin in eradicating Pseudomonas aeruginosa in children with cystic fibrosis. J Cyst Fibros. 2014;13:172–8.
Geller DE, Pitlick WH, Nardella PA, Tracewell WG, Ramsey BW. PHarmacokinetics and bioavailability of aerosolized tobramycin in cystic fibrosis. Chest. 2002;122:219–26.
Dolovichand MB, Dhand R. Aerosol drug delivery: developments in device design and clinical use. Lancet. 2011;377:1032–45.
Ibrahim BM, Tsifansky MD, Yang Y, Yeo Y. Challenges and advances in the development of inhalable drug formulations for cystic fibrosis lung disease. Expert Opin Drug Deliv. 2011;8:451–66.
Kuzmovand A, Minko T. Nanotechnology approaches for inhalation treatment of lung diseases. J Control Release. 2015;219:500–18.
Daniels T, Mills N, Whitaker P. Nebuliser systems for drug delivery in cystic fibrosis. Cochrane Database Syst Rev. 2013. doi:10.1002/14651858.CD007639.pub2.
Tang BC, Dawson M, Lai SK, Wang Y-Y, Suk JS, Yang M, et al. Biodegradable polymer nanoparticles that rapidly penetrate the human mucus barrier. Proc Natl Acad Sci. 2009;106(46):19268–73. doi:10.1073/pnas.0905998106.
Stegemann S, Kopp S, Borchard G, Shah VP, Senel S, Dubey R, et al. Developing and advancing dry powder inhalation towards enhanced therapeutics. Eur J Pharm Sci. 2013;48:181–94.
Wattsand AB, Williams RO. Nanoparticles for pulmonary delivery. In: Smythand DCH, Hickey JA, editors. Controlled pulmonary drug delivery. New York: Springer; 2011. p. 335–66.
Collnot E-M, Baldes C, Wempe MF, Hyatt J, Navarro L, Edgar KJ, et al. Influence of vitamin E TPGS poly(ethylene glycol) chain length on apical efflux transporters in Caco-2 cell monolayers. J Control Release. 2006;111:35–40.
Meenach SA, Anderson KW, Zach Hilt J, McGarry RC, Mansour HM. Characterization and aerosol dispersion performance of advanced spray-dried chemotherapeutic PEGylated phospholipid particles for dry powder inhalation delivery in lung cancer. Eur J Pharm Sci. 2013;49:699–711.
F. W. The ARLA Respiratory deposition calculator 2008.
Mert O, Lai SK, Ensign L, Yang M, Wang Y-Y, Wood J, et al. A poly(ethylene glycol)-based surfactant for formulation of drug-loaded mucus penetrating particles. J Control Release. 2012;157:455–60.
Bootz A, Vogel V, Schubert D, Kreuter J. Comparison of scanning electron microscopy, dynamic light scattering and analytical ultracentrifugation for the sizing of poly(butyl cyanoacrylate) nanoparticles. Eur J Pharm Biopharm. 2004;57:369–75.
Meenach SA, Kim YJ, Kauffman KJ, Kanthamneni N, Bachelder EM, Ainslie KM. Synthesis, optimization, and characterization of camptothecin-loaded acetalated dextran porous microparticles for pulmonary delivery. Mol Pharm. 2012;9:290–8.
Wu X, Hayes D, Zwischenberger JB, Kuhn RJ, Mansour HM. Design and physicochemical characterization of advanced spray-dried tacrolimus multifunctional particles for inhalation. Drug Des Devel Ther. 2013;7:59–72.
Meenach SA, Vogt FG, Anderson KW, Hilt JZ, McGarry RC, Mansour HM. Design, physicochemical characterization, and optimization of organic solution advanced spray-dried inhalable dipalmitoylphosphatidylcholine (DPPC) and dipalmitoylphosphatidylethanolamine poly(ethylene glycol) (DPPE-PEG) microparticles and nanoparticles for targeted respiratory nanomedicine delivery as dry powder inhalation aerosols. Int J Nanomedicine. 2013;8:275–93.
Wu X, Zhang W, Hayes D, Mansour HM. Physicochemical characterization and aerosol dispersion performance of organic solution advanced spray-dried cyclosporine A multifunctional particles for dry powder inhalation aerosol delivery. Int J Nanomedicine. 2013;8:1269–83.
Liand X, Mansour HM. Physicochemical characterization and water vapor sorption of organic solution advanced spray-dried inhalable trehalose microparticles and nanoparticles for targeted Dry powder pulmonary inhalation delivery. AAPS PharmSciTech. 2011;12:1420–30.
Hickey AJ, Mansour HM, Telko MJ, Xu Z, Smyth HDC, Mulder T, et al. Physical characterization of component particles included in dry powder inhalers. I. Strategy review and static characteristics. J Pharm Sci. 2007;96:1282–301.
Chew NYK, Chan H-K. The Role of particle properties in pharmaceutical powder inhalation formulations. J Aerosol Med. 2002;15:325–30.
Mohammadi G, Valizadeh H, Barzegar-Jalali M, Lotfipour F, Adibkia K, Milani M, et al. Development of azithromycin–PLGA nanoparticles: physicochemical characterization and antibacterial effect against salmonella typhi. Colloids Surf B: Biointerfaces. 2010;80:34–9.
Kaialyand W, Nokhodchi A. Dry powder inhalers: physicochemical and aerosolization properties of several size-fractions of a promising alterative carrier, freeze-dried mannitol. Eur J Pharm Sci. 2015;68:56–67.
Zhang Z, Xu L, Chen H, Li X. Rapamycin-loaded poly(ε-caprolactone)-poly(ethylene glycol)-poly(ε-caprolactone) nanoparticles: preparation, characterization and potential application in corneal transplantation. J Pharm Pharmacol. 2014;66:557–63.
Li X, Chang S, Du G, Li Y, Gong J, Yang M, et al. Encapsulation of azithromycin into polymeric microspheres by reduced pressure-solvent evaporation method. Int J Pharm. 2012;433:79–88.
Ungaro F, De Rosa G, Miro A, Quaglia F, La Rotonda MI. Cyclodextrins in the production of large porous particles: development of dry powders for the sustained release of insulin to the lungs. Eur J Pharm Sci. 2006;28:423–32.
Suarez S, Hickey AJ. Drug properties affecting aerosol behavior. Respir Care. 2000;45:652–66.
Hickey AJ, Heidi M. Delivery of Drugs by the Pulmonary Route. In: Florence AT, Siepmann J. editors. Modern Pharmaceutics: Applications and Advances, 5th ed. New York: Informa Healthcare; 2009. p 191–219.
Hickey AJ, Mansour HM. Formulation challenges of powders for the delivery of small molecular weight molecules as aerosols. In: Rathbone MJ, Hadgraft J, Roberts MS, Lane ME, editors. Modified-release drug delivery technology, 2nd ed. New York: Informa Healthcare; 2008. p. 573–602.
Edwards DA. The macrotransport of aerosol particles in the lung: aerosol deposition phenomena. J Aerosol Sci. 1995;26:293–317.
Acknowledgments And Disclosures
The authors gratefully acknowledge financial support from an Institutional Development Award (IDeA) from the National Institute of General Medical Sciences of the National Institutes of Health under grant number P20GM103430. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors thank RI-INBRE for HPLC access and RIN2 for SEM, DLS, PXRD, and DSC access.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, Z., Meenach, S.A. Synthesis and Characterization of Nanocomposite Microparticles (nCmP) for the Treatment of Cystic Fibrosis-Related Infections. Pharm Res 33, 1862–1872 (2016). https://doi.org/10.1007/s11095-016-1921-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-016-1921-5