Abstract
Purpose
Given the availability of TKIs with high central nervous system efficacy, the question arises as to whether upfront SRS provides additional clinical benefits. The goal of this study was to characterize the clinical outcomes of SRS as salvage therapy for TKI-uncontrolled BMs.
Methods
This retrospective study included EGFR-mutant NSCLC patients presenting BMs at the time of primary tumor diagnosis. BMs were categorized into three subgroups, referred to as “Nature of TKI-treated BMs”, “TKI-controlled brain metastases ± SRS”, and “SRS salvage therapy”. The first subgroup analysis characterized the effects of TKIs on tumor behavior. In the second subgroup, we compared outcomes of TKI-controlled BMs treated with TKI alone versus those treated with combined TKI-SRS therapy. The third subgroup characterized the outcomes of TKI-uncontrolled BMs treated with SRS as salvage therapy Clinical outcomes include local and distant tumor control.
Results
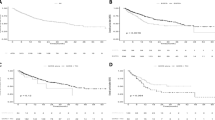
This study included 106 patients with a total of 683 BMs. TKI treatment achieved control in 63% of local tumors at 24 months. Among the TKI-controlled BMs, local tumor control was significantly higher in the combined TKI-SRS group (93%) than in the TKI-alone group (65%) at 24 months (p < 0.001). No differences were observed between the two groups in terms of distant tumor control (p = 0.832). In dealing with TKI-uncontrolled BMs, salvage SRS achieved local tumor control in 58% of BMs at 24 months.
Conclusions
While upfront TKI alone proved highly effective in BM control, this study also demonstrated the outcomes of SRS when implemented concurrently with TKI or as salvage therapy for TKI-uncontrolled BMs. This study also presents a strategy of the precise timing and targeting of SRS to lesions in progression.



Similar content being viewed by others
Abbreviations
- BM:
-
Brain metastasis
- EGFR:
-
Epidermal growth factor receptor
- GKRS:
-
Gamma-knife radiosurgery
- KPS:
-
Karnofsky Performance Scale
- MRI:
-
Magnetic resonance imaging
- NSCLC:
-
Non-small cell lung cancer
- SRS:
-
Stereotactic radiosurgery
- TKI:
-
Tyrosine kinase inhibitor
References
Aoyama H, Shirato H, Tago M, Nakagawa K, Toyoda T, Hatano K, Kenjyo M, Oya N, Hirota S, Shioura H, Kunieda E, Inomata T, Hayakawa K, Katoh N, Kobashi G (2006) Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial. JAMA 295:2483–2491. https://doi.org/10.1001/jama.295.21.2483
Chang EL, Wefel JS, Hess KR, Allen PK, Lang FF, Kornguth DG, Arbuckle RB, Swint JM, Shiu AS, Maor MH, Meyers CA (2009) Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol 10:1037–1044. https://doi.org/10.1016/S1470-2045(09)70263-3
Brown PD, Jaeckle K, Ballman KV, Farace E, Cerhan JH, Anderson SK, Carrero XW, Barker FG 2nd, Deming R, Burri SH, Menard C, Chung C, Stieber VW, Pollock BE, Galanis E, Buckner JC, Asher AL (2016) Effect of Radiosurgery alone vs Radiosurgery with Whole Brain Radiation Therapy on cognitive function in patients with 1 to 3 brain metastases: a Randomized Clinical Trial. JAMA 316:401–409. https://doi.org/10.1001/jama.2016.9839
Yamamoto M, Serizawa T, Shuto T, Akabane A, Higuchi Y, Kawagishi J, Yamanaka K, Sato Y, Jokura H, Yomo S, Nagano O, Kenai H, Moriki A, Suzuki S, Kida Y, Iwai Y, Hayashi M, Onishi H, Gondo M, Sato M, Akimitsu T, Kubo K, Kikuchi Y, Shibasaki T, Goto T, Takanashi M, Mori Y, Takakura K, Saeki N, Kunieda E, Aoyama H, Momoshima S, Tsuchiya K (2014) Stereotactic radiosurgery for patients with multiple brain metastases (JLGK0901): a multi-institutional prospective observational study. Lancet Oncol 15:387–395. https://doi.org/10.1016/S1470-2045(14)70061-0
Chiou GY, Chiang CL, Yang HC, Shen CI, Wu HM, Chen YW, Chen CJ, Luo YH, Hu YS, Lin CJ, Chung WY, Shiau CY, Guo WY, Pan DH, Lee CC (2021) Combined stereotactic radiosurgery and tyrosine kinase inhibitor therapy versus tyrosine kinase inhibitor therapy alone for the treatment of non-small cell lung cancer patients with brain metastases. J Neurosurg 1–8. https://doi.org/10.3171/2021.9.JNS211373
Unger KR, Lominska CE, Chanyasulkit J, Randolph-Jackson P, White RL, Aulisi E, Jacobson J, Jean W, Gagnon GJ (2012) Risk factors for posttreatment edema in patients treated with stereotactic radiosurgery for meningiomas. Neurosurgery 70:639–645. https://doi.org/10.1227/NEU.0b013e3182351ae7
Loganadane G, Dhermain F, Louvel G, Kauv P, Deutsch E, Le Pechoux C, Levy A (2018) Brain Radiation Necrosis: current management with a focus on non-small cell Lung Cancer Patients. Front Oncol 8:336. https://doi.org/10.3389/fonc.2018.00336
Miller JA, Bennett EE, Xiao R, Kotecha R, Chao ST, Vogelbaum MA, Barnett GH, Angelov L, Murphy ES, Yu JS, Ahluwalia MS, Suh JH, Mohammadi AM (2016) Association between Radiation Necrosis and Tumor Biology after Stereotactic Radiosurgery for Brain Metastasis. Int J Radiat Oncol Biol Phys 96:1060–1069. https://doi.org/10.1016/j.ijrobp.2016.08.039
Kang L, Mai J, Liang W, Zou Q, Huang C, Lin Y, Liang Y (2023) CNS efficacy of afatinib as first-line treatment in advanced non-small cell lung cancer patients with EGFR mutations. Front Oncol 13:1094195. https://doi.org/10.3389/fonc.2023.1094195
Zhao Y, Li S, Yang X, Chu L, Wang S, Tong T, Chu X, Yu F, Zeng Y, Guo T, Zhou Y, Zou L, Li Y, Ni J, Zhu Z (2022) Overall survival benefit of osimertinib and clinical value of upfront cranial local therapy in untreated EGFR-mutant nonsmall cell lung cancer with brain metastasis. Int J Cancer 150:1318–1328. https://doi.org/10.1002/ijc.33904
Yang JCH, Kim SW, Kim DW, Lee JS, Cho BC, Ahn JS, Lee DH, Kim TM, Goldman JW, Natale RB, Brown AP, Collins B, Chmielecki J, Vishwanathan K, Mendoza-Naranjo A, Ahn MJ (2020) Osimertinib in patients with epidermal growth factor receptor mutation-positive non-small-cell Lung Cancer and Leptomeningeal Metastases: the BLOOM Study. J Clin Oncol 38:538–547. https://doi.org/10.1200/JCO.19.00457
Park S, Lee MH, Seong M, Kim ST, Kang JH, Cho BC, Lee KH, Cho EK, Sun JM, Lee SH, Ahn JS, Park K, Ahn MJ (2020) A phase II, multicenter, two cohort study of 160 mg osimertinib in EGFR T790M-positive non-small-cell lung cancer patients with brain metastases or leptomeningeal disease who progressed on prior EGFR TKI therapy. Ann Oncol 31:1397–1404. https://doi.org/10.1016/j.annonc.2020.06.017
Reungwetwattana T, Nakagawa K, Cho BC, Cobo M, Cho EK, Bertolini A, Bohnet S, Zhou C, Lee KH, Nogami N, Okamoto I, Leighl N, Hodge R, McKeown A, Brown AP, Rukazenkov Y, Ramalingam SS, Vansteenkiste J (2018) CNS response to Osimertinib Versus standard epidermal growth factor receptor tyrosine kinase inhibitors in patients with untreated EGFR-Mutated Advanced Non-Small-Cell Lung Cancer. J Clin Oncol: JCO2018783118. https://doi.org/10.1200/JCO.2018.78.3118
Patel PH, Palma D, McDonald F, Tree AC (2019) The Dandelion Dilemma Revisited for Oligoprogression: treat the whole lawn or weed selectively? Clin Oncol (R Coll Radiol) 31:824–833. https://doi.org/10.1016/j.clon.2019.05.015
Langston J, Patil T, Ross Camidge D, Bunn PA, Schenk EL, Pacheco JM, Jurica J, Waxweiler TV, Kavanagh BD, Rusthoven CG (2023) CNS downstaging: an emerging treatment paradigm for extensive brain metastases in Oncogene-Addicted Lung Cancer. Lung Cancer 178:103–107. https://doi.org/10.1016/j.lungcan.2023.02.006
Magnuson WJ, Lester-Coll NH, Wu AJ, Yang TJ, Lockney NA, Gerber NK, Beal K, Amini A, Patil T, Kavanagh BD, Camidge DR, Braunstein SE, Boreta LC, Balasubramanian SK, Ahluwalia MS, Rana NG, Attia A, Gettinger SN, Contessa JN, Yu JB, Chiang VL (2017) Management of brain metastases in tyrosine kinase inhibitor-naive epidermal growth factor receptor-mutant non-small-cell Lung Cancer: a retrospective multi-institutional analysis. J Clin Oncol 35:1070–1077. https://doi.org/10.1200/JCO.2016.69.7144
Lee CC, Chou CL, Chen CJ, Yang HC, Wu HM, Shiau CY, Pan DH, Chung WY (2018) Stereotactic radiosurgery for hypervascular intracranial tumors. J Neurooncol 140:547–558. https://doi.org/10.1007/s11060-018-2980-8
Pai FY, Chen CJ, Wang WH, Yang HC, Lin CJ, Wu HM, Lin YC, Chen HS, Yen YS, Chung WY, Guo WY, Pan DH, Shiau CY, Lee CC (2019) Low-dose Gamma Knife Radiosurgery for Acromegaly. Neurosurgery 85:E20–E30. https://doi.org/10.1093/neuros/nyy410
Lee CC, Pan DH, Chung WY, Liu KD, Yang HC, Wu HM, Guo WY, Shih YH (2012) Brainstem cavernous malformations: the role of Gamma Knife surgery. J Neurosurg 117 Suppl:164–169. https://doi.org/10.3171/2012.8.GKS121066
Lee CC, Wintermark M, Xu Z, Yen CP, Schlesinger D, Sheehan JP (2014) Application of diffusion-weighted magnetic resonance imaging to predict the intracranial metastatic tumor response to gamma knife radiosurgery. J Neurooncol 118:351–361. https://doi.org/10.1007/s11060-014-1439-9
Lee CC, Yen CP, Xu Z, Schlesinger D, Sheehan J (2014) Large intracranial metastatic tumors treated by Gamma Knife surgery: outcomes and prognostic factors. J Neurosurg 120:52–59. https://doi.org/10.3171/2013.9.JNS131163
Shaw E, Scott C, Souhami L, Dinapoli R, Kline R, Loeffler J, Farnan N (2000) Single dose radiosurgical treatment of recurrent previously irradiated primary brain tumors and brain metastases: final report of RTOG protocol 90 – 05. Int J Radiat Oncol Biol Phys 47:291–298. https://doi.org/10.1016/s0360-3016(99)00507-6
Lin YY, Guo WY, Lu CF, Peng SJ, Wu YT, Lee CC (2023) Application of artificial intelligence to stereotactic radiosurgery for intracranial lesions: detection, segmentation, and outcome prediction. J Neurooncol 161:441–450. https://doi.org/10.1007/s11060-022-04234-x
Snell JW, Sheehan J, Stroila M, Steiner L (2006) Assessment of imaging studies used with radiosurgery: a volumetric algorithm and an estimation of its error. Technical note. J Neurosurg 104:157–162. https://doi.org/10.3171/jns.2006.104.1.157
Peled N, Kian W, Inbar E, Goldstein IM, Zemel M, Rotem O, Rozenblum AB, Nechushtan H, Dudnik E, Levin D, Zer A, Keren-Rosenberg S, Yust-Katz S, Fuchs V, Remilah AA, Shelef I, Roisman LC (2022) Osimertinib in advanced EGFR-mutant lung adenocarcinoma with asymptomatic brain metastases: an open-label, 3-arm, phase II pilot study. Neurooncol Adv 4:vdab188. https://doi.org/10.1093/noajnl/vdab188
Vogelbaum MA, Brown PD, Messersmith H, Brastianos PK, Burri S, Cahill D, Dunn IF, Gaspar LE, Gatson NTN, Gondi V, Jordan JT, Lassman AB, Maues J, Mohile N, Redjal N, Stevens G, Sulman E, van den Bent M, Wallace HJ, Weinberg JS, Zadeh G, Schiff D (2022) Treatment for Brain Metastases: ASCO-SNO-ASTRO Guideline. J Clin Oncol 40:492–516. https://doi.org/10.1200/JCO.21.02314
Yomo S, Oda K (2018) Impacts of EGFR-mutation status and EGFR-TKI on the efficacy of stereotactic radiosurgery for brain metastases from non-small cell lung adenocarcinoma: a retrospective analysis of 133 consecutive patients. Lung Cancer 119:120–126. https://doi.org/10.1016/j.lungcan.2018.03.013
Dohm AE, Tang JD, Mills MN, Liveringhouse CL, Sandoval ML, Perez BA, Robinson TJ, Creelan BC, Gray JE, Etame AB, Vogelbaum MA, Forsyth P, Yu HM, Oliver DE, Ahmed KA (2022) Clinical outcomes of non-small cell lung cancer brain metastases treated with stereotactic radiosurgery and immune checkpoint inhibitors, EGFR tyrosine kinase inhibitors, chemotherapy and immune checkpoint inhibitors, or chemotherapy alone. J Neurosurg 1–8. https://doi.org/10.3171/2022.9.JNS221896
Shao J, Li J, Song L, He Q, Wu Y, Li L, Liu D, Wang C, Li W (2022) The number of brain metastases predicts the survival of non-small cell lung cancer patients with EGFR mutation status. Cancer Rep (Hoboken) 5:e1550. https://doi.org/10.1002/cnr2.1550
Lin NU, Lee EQ, Aoyama H, Barani IJ, Barboriak DP, Baumert BG, Bendszus M, Brown PD, Camidge DR, Chang SM, Dancey J, de Vries EG, Gaspar LE, Harris GJ, Hodi FS, Kalkanis SN, Linskey ME, Macdonald DR, Margolin K, Mehta MP, Schiff D, Soffietti R, Suh JH, van den Bent MJ, Vogelbaum MA, Wen PY Response Assessment in Neuro-Oncology g (2015) response assessment criteria for brain metastases: proposal from the RANO group. Lancet Oncol 16: e270–278 https://doi.org/10.1016/S1470-2045(15)70057-4
Author information
Authors and Affiliations
Contributions
The first draft of the manuscript was written by Joseph Shang-En Hung and all authors commented on previous versions of the manuscript. All authors reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Disclosure
The authors have no relevant disclosures to make.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hung, J.SE., Su, YH., Chen, CJ. et al. Is it advisable to perform radiosurgery for EGFR-TKI-controlled brain metastases? A retrospective study of the role of radiosurgery in lung cancer treatment. J Neurooncol 164, 413–422 (2023). https://doi.org/10.1007/s11060-023-04425-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-023-04425-0