Abstract
Background
Isocitrate dehydrogenase (IDH) mutated diffuse lower-grade gliomas (dLGG) are infiltrating brain tumors and increasing evidence is in favor of early multimodal treatment. In a Scandinavian population-based setting, we wanted to study treatment patterns over the last 15 years, focusing on the short-term postoperative course to better understand the potential negative consequences of treatment.
Methods
Patients ≥ 18 years with primary IDH-mutated dLGG grade 2 and 3, operated between January 2007–June 2021 were identified. Patients were divided into subgroups (2007–2011, 2012–2016, and 2017–2021) and comparisons regarding tumor- and disease characteristics, treatment, and postoperative outcome were performed.
Results
We identified 202 patients (n = 61, 2007–2011; n = 72, 2012–2016; n = 69, 2017–2021), where of 193 underwent resection without change in proportion of resections over time. More patients underwent complete resections in recent times (6.1%; 15.7%; 26.1%, respectively; p = 0.016). Forty-two patients had any neurological deficit postoperatively (14.8%; 23.6%; 23.2%; p = 0.379), mostly minor and transient. Differences in oncological therapy were seen between the investigated subgroups. Early radiotherapy alone (32.8%; 7%; 2.9%; p < 0.001), concomitant chemoradiotherapy (23%; 37.5%; 17.4%; p = 0.022), sequential chemoradiotherapy (0%; 18%; 49.3%; p < 0.001), and no adjuvant treatment (42.6%; 23.6%; 18.8%; p = 0.009) shifted during the studied period. Increasingly more patients received proton radiotherapy compared to photon radiotherapy during the later time periods (p < 0.001).
Conclusion
Complete resections were performed more often in later time periods without an apparent increase in surgical morbidity. Early adjuvant oncological treatment shifted towards providing chemotherapy and combined chemoradiotherapy more often in later time periods. Protons replaced photons as the radiation modality of choice.
Similar content being viewed by others
Introduction
Diffuse lower-grade gliomas (dLGGs) are slow-growing infiltrative tumors, typically affecting adults of younger age [1]. Over time, accumulating molecular aberrations tend to cause a more malignant tumor, leading to increased morbidity and premature death. The estimated overall survival (OS) is highly dependent on individual risk factors and the biological profile of the tumor. Recently, the 2021 version of the World Health Organization (WHO) Classification of tumors in the central nervous system further emphasized the molecular aspects of the classification, where adult-type dLGGs are characterized by the IDH-mutation [2] Moreover, due to the controversy of WHO-grading within the IDH-mutated tumors, it is now more common to report diffuse grade 2 and 3 astrocytomas (IDH-mutant without 1p19q codeletion) and oligodendrogliomas (IDH-mutant with 1p19q-codeletion) together under the term lower-grade gliomas [3,4].
There have been several important papers demonstrating that more active treatment of IDH-mutated tumors significantly prolongs survival [5,6,7]. Resection compared to biopsy is the preferred surgical strategy and a dose-response relationship is present, where a higher extent of resection (EoR) is favorable [7,8,9,10]. The adjuvant treatment strategy has changed in recent years following landmark papers demonstrating a clear survival benefit of the addition of upfront chemotherapy (procarbazine, lomustine, and vincristine, PCV) to radiotherapy [11,12,13,14] .
Transient neurologic deterioration following surgery is common [15,16,17,18]. A more active surgical strategy logically puts the patient at an increased neurological risk. For oncological therapy, perceived high-risk patients with IDH-mutated gliomas, according to the studies by Pignatti et al. [19] and Buckner et al. [12] from the pre-molecular era, are often given adjuvant treatment upfront following surgery to minimize the risk for rapid tumor progression and relapse. The perceived low-risk patients, on the other hand, are often managed with wait-and-scan to minimize the risk of long-term consequences of radiotherapy [20,21].
Altogether, it is likely that there has been a change during the past decade in the management of patients with IDH-mutated dLGG. We presumed a more active surgical approach and a higher proportion of patients receiving upfront oncological treatment to be found. Specifically, for the surgical treatment, we hypothesized that more patients in recent time periods underwent resection, and for those resected, a higher EoR was anticipated.
Materials and methods
Patient cohort
All patients in the western health care region of Sweden with newly diagnosed suspected primary intracranial intraaxial tumors, are managed by a multidisciplinary team (MDT) with weekly conferences at the Sahlgrenska University Hospital, Gothenburg, Sweden.
We aimed to include all patients fulfilling the study criteria in a database at Sahlgrenska University Hospital, during a time spanning from January 2007 to June 2021. Inclusion criteria were all patients ≥ 18 years and a primary histological diagnosis of IDH-mutated dLGG grade 2 and 3 during the study period. Patients with IDH mutated grade 4 astrocytomas were excluded. Patients were divided into three subgroups based on balanced time periods of histopathological diagnosis (2007–2011, 2012–2016, 2017–2021) before data analysis, taking into consideration those landmark papers by Jakola et al. [22] and Buckner et al. [12] could have affected the treatment strategy during this time in a surgical and oncological aspect, respectively [12,23]. These time periods were based mainly on these two papers due to their perceived clinical impact and publication year, 2012 respectively 2016, to evaluate the subsequent clinical effects. In total, 202 patients were identified. Data was collected in a retrospective fashion and all patients were followed at least six months after surgery.
Clinical and radiological characteristics
The demographic, surgical, and clinical data was retrospectively collected from electronic health records. Preoperative Karnofsky performance status (KPS) score was divided into three groups; 80–100 (normal activity), 50–70 (care for self with occasional assistance but unable to work or perform normal activities), 0–40 (patients with significant care needs, including hospitalization or institutionalization) [24]. Preoperative deficits were recorded from the patients logs. Cognitive deficit recorded was based on patient-reported symptoms and not necessarily cognitive assessment, and recorded from patient logs. Severe cognitive deficits affected the patient’s ability to work and daily life. The cognitive deficit was not based on the objective neurophysiologic assessment, as this was not routine during the first and second period. Post-operative neurological deficits were categorized as either any new or worsened deficit after surgery, with further classification into either minor or severe ones. Severe deficits were defined as aphasia or severe dysphasia with an impact on effective communication, hemianopia, motor function grade < 4 on the Medical Research Council (MRC) scale based on patient logs or cognitive deficit affecting daily life [18,25]. Deficits persisting more than 3 months were considered permanent [18]. Neurosurgical complications were evaluated using the Landriel-Ibanez classification within 30 days of surgery, [26] and neurological deficits were presented separately.
The surgical techniques were collected from the operation logs and included type of surgery (resection or biopsy), use of neuronavigation, ultrasound, motor mapping and monitoring under general anesthesia, awake mapping, ultrasonic aspirator and use of 5-ALA florescence. 5-ALA was used for hotspot detection and guided by regular microscope.
Type of radiation (photons or protons), and chemotherapy were registered. In this study, focusing on the initial management, adjuvant oncological treatment was defined as having chemotherapy and/or radiotherapy within six months after surgery. The patient was registered to have no oncological treatment if none was started within six months from surgery. In order not to miss planned sequential treatments started prior to six months, all patients who received oncological treatment were followed up to 12 months after surgery where both modalities were registered even if only one of them was initiated prior to six months. Chemoradiotherapy was defined as having either concomitant or sequential treatment.
Tumor volume was assessed by segmentation on magnetic resonance imaging (MRI) scans on the sequence where the glioma was best visualized (T2w or FLAIR sequences) with the software 3D slicer version 4.6.2 in accordance with previously published studies [27,28]. The tumor volume measurements were performed for general research purposes (not this specific project) and no specific measures were taken for blinding of clinical outcome and histomolecular data. The volumetric analysis was performed by several trained researchers and research assistants, and all were validated by an experienced neurosurgeon (A.S.J.) The postoperative volumes were calculated on MRI scans < 4 months of surgery. For some patients with postoperative scans performed > 4 months, it was possible to make a qualitative assessment regarding the variable complete versus partial resection, but cases with postoperative MRI performed later than 3 months after surgery were not included for volumetric assessment, but with the exemption being patients with radical resection where the volume was considered to be 0 cm [3].
Routine clinical analysis of IDH-status using a step-wise approach with initial IHC for R132H mutation followed by next-generation sequencing for IDH1 and IDH2 mutations if negative IHC was introduced in 2016. Patients diagnosed prior to 2016 have been reclassified as described in previous work [29].
Statistical analysis
IBM SPSS Statistics software program version 28.0 was used to perform statistical analyses. Data were presented as count values, proportions in percentage, means, and median, and the spread was presented with SD or quartiles one and three (Q1, Q3). The three subgroups were compared regarding categorical data using crosstabs and Pearson’s chi-square test or Fisher’s exact test (Fisher-Freeman-Halton), with a significance level set to 0.05. The distribution of continuous data were assessed by using Q-Q plots. Normally distributed data were analyzed with ANOVA, otherwise with Kruskal-Wallis.
Results
Baseline characteristics
A total of 202 patients were identified: 61 patients operated between 2007 and 2011 (Group 1), 72 patients between 2012 and 2016 (Group 2), and 69 patients between 2017 and 2021 (Group 3). The mean age at surgery was 41.7, 42.5, and 45.3 years in each group, respectively. Females were underrepresented in all three groups. Seizure was the most common presenting symptom. A detailed description of baseline characteristics is presented in Table 1. The preoperative and postoperative median tumor volumes were similar over time, and did not statistically differ between groups preoperatively (p = 0.329) and postoperatively (p = 0.401). However, complete resections increased over time from 3 patients (6.1%) in the earliest group to 18 patients (26.1%) in the latest period (p = 0.016).
Most patients had a KPS score between 80 and 100. Over time, a larger number of patients underwent neuropsychologic assessment both pre- and postoperatively. DTI/tractography, perfusion MRI, MR spectroscopy, and navigated TMS were performed to a greater extent in Groups 2 and 3. Most dLGGs were unifocal, unilateral, and located in the frontal or temporal lobe.
Treatment variables and techniques
As seen in Table 2, 193 patients in total were treated with resection, compared to nine patients that underwent biopsy only and there was no change in the ratio of resected versus biopsied patients over time (p = 0.977). The proportion of complete resections increased over time (2007–2011; 6.1%, 2012–2016; 15.7%, and 2017–2021; 26.1%; p = 0.016), see Table 1. Eight patients in total underwent resection supported by 5-ALA (0%, 8.7%, and 3%, p = 0.073) and nine patients, all of whom in group 3 had intraoperative MRI (13.6% of patients in Group 3).
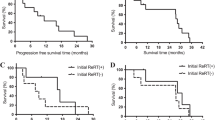
The proportion receiving concomitant (p = 0.012) as well as sequential (p < 0.001) chemoradiotherapy within 12 months postoperatively (see details under Methods) increased significantly in the later groups. Likewise, the proportion of patients treated with chemotherapy alone after surgery was greater in Groups 2 and 3 (p = 0.022) as seen in Table 3; Fig. 1. Among patients receiving chemotherapy (either chemotherapy alone or chemoradiotherapy), the use of PCV increased over time (8.2%; 19.4%; 39.3%, p = 0.01), and consequently the use of Temozolomide (TMZ) decreased (91.8%; 80.6%; 57.1% p = < 0.001). All patients who had chemotherapy concomitant with radiotherapy received TMZ.
Adjuvant treatment following surgery. The bars represent percentage (%) of the total number of patients in each group. Chemo; chemotherapy alone. Radio; radiotherapy alone. Chemoradio con; concomitant chemoradiotherapy (e.g., radiotherapy concomitant with temozolomide +/- adjuvant). Chemoradio seq; sequential chemoradiotherapy (i.e. combined treatment but without concomitant chemotherapy). None; no adjuvant treatment.
Administration of radiotherapy alone within six months postoperative was more common in the earliest group than in the later ones (p < 0.001), as shown in Fig. 1. Over time, the proportion of patients not receiving any adjuvant treatment within six months after surgery also decreased (p = 0.009). In irradiated patients, an increase in the proportion of patients receiving photon radiotherapy compared to proton radiotherapy was observed (p < 0.001) as seen in Fig. 2.
Only one patient received a hypofractionated course of radiotherapy. All other patients received radiotherapy at 1.8-2.0 Gy/fraction to a total dose of 50–54 Gy for grade 2 tumors or 59.4–60 Gy for grade 3 tumors, respectively.
Postoperative complications and neurologic deficits
No complication after surgery according to the Ibanez classification was the most frequent outcome in all groups, with similar frequency over time as seen in Table 4. New or worsened neurological deficit postoperatively was common during all periods, also without any significant difference in incidence over time. Most of these patients suffered from nonsevere deficits as seen in Table 4 and Supplementary Tables 1 and 2.
In total, 44 patients (14.8% in Group 1, 23.6% in Group 2, 26.1% in Group 3, p = 0.268) experienced any permanent deficit (i.e., any deficit, severe or nonsevere, persisting more than three months). Ten patients (5.0%) had a severe deficit persisting more than three months. For a detailed overview of permanent deficits, see Supplementary Tables 1 and 2. No patient died within 30 days. Table 4 presents additional details on complications and neurological deficits after surgery.
Discussion
We found a higher rate of complete radiological resection in the later time periods without a significant increase in neurological morbidity. Furthermore, early oncological therapy has become more common with time, and there has been a shift towards the use of PCV instead of TMZ and proton radiotherapy instead of photon radiotherapy.
The proportion of patients having biopsy were considerably smaller than those having a resection, and a change in treatment pattern could not be seen over time. However, the number of complete resections increased over time, suggesting a more active surgical approach. The reasoning behind the more extensive surgery, although not analyzed specifically in this study, is that increased EoR has been shown to be strongly associated with improved survival, especially in patients with IDH-mutated astrocytomas [30,31].
Increased use of intraoperative tools such as mapping, monitoring, neuronavigation, and intraoperative imaging may indicate an attempt to achieve more radical resections, also in eloquent regions, which can come with a risk of more neurological impairment postoperatively. The majority of patients experienced no surgical complications, and no difference was seen over time. Regarding neurologic deterioration, temporary loss of function is a known risk after surgery, for instance, transient supplementary motor area (SMA) syndrome, which usually resolves within three months due to brain plasticity [32, 33]. There was a nonsignificant trend towards more neurologic deficits postoperative in recent time periods, although most were nonsevere and transient. The number of patients that experienced severe permanent neurologic deficits was small and the observed increase in recent time periods was not significant. We report a higher number of deficits compared to many other studies, but the reported proportion of permanent severe deficits (5.0%) aligns well with the reported deficits in the literature [18,34]. However, if this is due to a difference in reporting remains speculative. Furthermore, our definition of a permanent deficit (i.e., persisting more than three months) does not mean that further improvements are not seen in a longer perspective [35].
Neuropsychological assessment was more frequent in the later time periods. Since 2017, all patients with a presumed lower-grade tumor are assessed both pre- and postoperatively. Compared to earlier subjective evaluations of cognitive functioning, these assessments are more thorough and capture various aspects of cognitive functioning; visual and verbal learning and memory, perception and visuo-spatial abilities, verbal functioning, psychomotor speed, motor speed, executive functioning including inhibition, mental flexibility and planning, different aspects of attention, and working memory. The assessments also include measures of mental fatigue, quality of life, depression, and anxiety. Although not intentional, this more detailed assessment and functional focus may have affected both pre- and postoperative registration of neurological deficits. This may contribute to the observed nonsignificant increase in deficits over time. This speculation that our data is influenced by the increased awareness and discovery of cognitive deficits following 2017 is possibly further strengthened by the fact that in the latest period there were trends of patients who have smaller and incidental tumors, but still report a higher percentage of preoperative deficits.
We found that patients in the later time periods more frequently were treated with chemoradiotherapy, as well as with chemotherapy alone. The decreased use of TMZ in the later time periods could partially be related to fewer tumors with IDH-mutation being classified as astrocytoma grade 3. Receiving radiotherapy alone after surgery has become rare, 32.8% in the earliest time period to 2.9% in the last (p < 0.001), perhaps a clinical effect of the Buckner trial [12]. Over time, it has also become more common to receive adjuvant treatment, with only around 20% of patients being selected for wait-and-scan in the later groups. The consequences of early radiotherapy may not be noticeable early on as side effects may present years after treatment [21,36]. However, in patients with negative prognostic factors, the survival benefits outweighs potential late side effects [12,37]. Still, which parameters to be used as prognostic factors are controversial as most of these parameters are from the pre-molecular era [38,39]. Therefore, the simple use of an age cut-off at 40 years, knowing the strong association between the status of IDH-mutation and age, is therefore outdated [19,40]. Furthermore, we observed that photon radiotherapy basically replaced by proton radiotherapy, which could be explained by an intention to avoid radiotherapy induced side effects [41].
Long-term follow-up is needed to look more closely at the tradeoff between survival benefit and functional consequences with more aggressive initial therapy. The ongoing PRO-GLIO study (NCT05190172), an RCT study on photon versus proton radiation in IDH-mutated LGG, is looking more closely at potential long-term adverse effects and survival benefits with different radiotherapy modalities. Further studies on the optimal timing of adjuvant oncological treatment, such as the IWOT study (NCT03763422) are important as patients with dLGG have a relatively long expected survival following diagnosis. Moreover, studies on prognostic factors stratified by the molecular subtype are needed to better define high-risk patients.
Limitations
Limitations include those associated with a retrospective study design and the lack of assessable imaging data for all cases in the earliest period where early postoperative MRI was not a part of the standard clinical routine. Neuropsychological assessment was not routinely done in the earlier time periods with possible detection bias for cognitive and more subtle neurological problems, as discussed in more detail above. The inherent small sample size limits the statistical power to detect smaller, but still meaningful differences over time.
Conclusion
In our center, the number of resections remains stable, but a more active surgical attitude resulted in more complete resections in recent years. No apparent increase in surgical morbidity was observed over time. Adjuvant chemotherapy has been implemented as part of standard-of-care for dLGG. In our center, radiotherapy has shifted from exclusively photons to a situation where a majority of patients now receive proton radiotherapy.
References
Ostrom QT, Gittleman H, Fulop J et al (2015) CBTRUS Statistical Report: Primary Brain and Central Nervous System Tumors Diagnosed in the United States in 2008–2012. Neuro-oncology 17(Suppl 4):iv1–iv62
Louis DN, Perry A, Wesseling P et al (2021) The 2021 WHO Classification of Tumors of the Central Nervous System: a summary. Neuro Oncol. 23:1231–1251
Eckel-Passow JE, Lachance DH, Molinaro AM et al (2015) Glioma Groups Based on 1p/19q, IDH, and TERT Promoter Mutations in Tumors. N Engl J Med 372(26):2499–2508
Cancer Genome Atlas Research N, Brat DJ, Verhaak RG et al (2015) Comprehensive, Integrative Genomic Analysis of Diffuse Lower-Grade Gliomas. N Engl J Med 372(26):2481–2498
Jakola AS, Skjulsvik AJ, Myrmel KS et al (2017) Surgical resection versus watchful waiting in low-grade gliomas. Ann Oncol 28(8):1942–1948
Patel SH, Bansal AG, Young EB et al (2019) Extent of Surgical Resection in Lower-Grade Gliomas: Differential Impact Based on Molecular Subtype. AJNR Am J Neuroradiol 40(7):1149–1155
Wijnenga MMJ, French PJ, Dubbink HJ et al (2018) The impact of surgery in molecularly defined low-grade glioma: an integrated clinical, radiological, and molecular analysis. Neuro-oncology 20(1):103–112
Still MEH, Roux A, Huberfeld G et al (2019) Extent of Resection and Residual Tumor Thresholds for Postoperative Total Seizure Freedom in Epileptic Adult Patients Harboring a Supratentorial Diffuse Low-Grade Glioma. Neurosurgery 85(2):E332–E340
Ius T, Pauletto G, Tomasino B et al (2020) Predictors of Postoperative Seizure Outcome in Low Grade Glioma: From Volumetric Analysis to Molecular Stratification. Cancers (Basel): 12(2):397
Weller M, van den Bent M, Preusser M et al (2021) EANO guidelines on the diagnosis and treatment of diffuse gliomas of adulthood. Nat Rev Clin Oncol 18(3):170–186
Buckner J, Giannini C, Eckel-Passow J et al (2017) Management of diffuse low-grade gliomas in adults - use of molecular diagnostics. Nat Rev Neurol 13(6):340–351
Buckner JC, Shaw EG, Pugh SL et al (2016) Radiation plus Procarbazine, CCNU, and Vincristine in Low-Grade Glioma. N Engl J Med 374(14):1344–1355
van den Bent MJ, Brandes AA, Taphoorn MJ et al (2013) Adjuvant procarbazine, lomustine, and vincristine chemotherapy in newly diagnosed anaplastic oligodendroglioma: long-term follow-up of EORTC brain tumor group study 26951. J Clin oncology: official J Am Soc Clin Oncol 31(3):344–350
Cairncross JG, Wang M, Jenkins RB et al (2014) Benefit from procarbazine, lomustine, and vincristine in oligodendroglial tumors is associated with mutation of IDH. J Clin oncology: official J Am Soc Clin Oncol 32(8):783–790
Carstam L, Smits A, Milos P et al (2019) Neurosurgical patterns of care for diffuse low-grade gliomas in Sweden between 2005 and 2015. Neurooncol Pract 6(2):124–133
Solheim O, Jakola AS, Gulati S, Johannesen TB (2012) Incidence and causes of perioperative mortality after primary surgery for intracranial tumors: a national, population-based study. J Neurosurg 116(4):825–834
De Witt Hamer PC, De Witt Hamer PC, Klein M, Hervey-Jumper SL, Wefel JS, Berger MS (2021) Functional Outcomes and Health-Related Quality of Life Following Glioma Surgery. Neurosurgery 88(4):720–732
De Witt Hamer PC, Robles SG, Zwinderman AH, Duffau H, Berger MS (2012) Impact of intraoperative stimulation brain mapping on glioma surgery outcome: a meta-analysis. J Clin oncology: official J Am Soc Clin Oncol 30(20):2559–2565
Pignatti F, van den Bent M, Curran D et al (2002) Prognostic factors for survival in adult patients with cerebral low-grade glioma. J Clin oncology: official J Am Soc Clin Oncol 20(8):2076–2084
Baumert BG, Hegi ME, van den Bent MJ et al (2016) Temozolomide chemotherapy versus radiotherapy in high-risk low-grade glioma (EORTC 22033–26033): a randomised, open-label, phase 3 intergroup study. Lancet Oncol 17(11):1521–1532
Douw L, Klein M, Fagel SS et al (2009) Cognitive and radiological effects of radiotherapy in patients with low-grade glioma: long-term follow-up. Lancet Neurol 8(9):810–818
Jakola AS, Skjulsvik AJ, Myrmel KS et al (2017) Surgical resection versus watchful waiting in low-grade gliomas. Ann Oncol. 28(8):1942-1948
Jakola AS, Myrmel KS, Kloster R et al (2012) Comparison of a strategy favoring early surgical resection vs a strategy favoring watchful waiting in low-grade gliomas. Jama 308(18):1881–1888
Martin RC, Gerstenecker A, Nabors LB, Marson DC, Triebel KL (2015) Impairment of medical decisional capacity in relation to Karnofsky Performance Status in adults with malignant brain tumor. Neurooncol Pract 2(1):13–19
Compston A (2010) Aids to the investigation of peripheral nerve injuries. Medical Research Council: Nerve Injuries Research Committee. His Majesty’s Stationery Office: ; 1942;pp. 48 (iii) and 74 figures and 7 diagrams; with aids to the examination of the peripheral nervous system. By Michael O’Brien for the Guarantors of Brain. Saunders Elsevier: 2010; pp. [8] 64 and 94 Figures. Brain;133(10):2838–2844
Landriel Ibanez FA, Hem S, Ajler P et al (2011) A new classification of complications in neurosurgery. World Neurosurg 75(5–6):709–715 discussion 604–711
Fedorov A, Beichel R, Kalpathy-Cramer J et al (2012) 3D Slicer as an image computing platform for the Quantitative Imaging Network. Magn Reson imaging 30(9):1323–1341
Corell A, Ferreyra Vega S, Hoefling N et al (2020) The clinical significance of the T2-FLAIR mismatch sign in grade II and III gliomas: a population-based study. BMC Cancer 20(1):450
Ferreyra Vega S, Olsson Bontell T, Corell A, Smits A, Jakola AS, Carén H (2021) DNA methylation profiling for molecular classification of adult diffuse lower-grade gliomas. Clin Epigenetics 13(1):102
Jakola AS, Pedersen LK, Skjulsvik AJ, Myrmel K, Sjavik K, Solheim O (2022) The impact of resection in IDH-mutant WHO grade 2 gliomas: a retrospective population-based parallel cohort study. J Neurosurg. 137(5):1321–1328
Delev D, Heiland DH, Franco P et al (2019) Surgical management of lower-grade glioma in the spotlight of the 2016 WHO classification system. J Neurooncol 141(1):223–233
Vassal M, Charroud C, Deverdun J et al (2017) Recovery of functional connectivity of the sensorimotor network after surgery for diffuse low-grade gliomas involving the supplementary motor area. J Neurosurg 126(4):1181–1190
Duffau H, Capelle L, Denvil D et al (2003) Functional recovery after surgical resection of low grade gliomas in eloquent brain: hypothesis of brain compensation. J Neurol Neurosurg Psychiatry 74(7):901–907
Bo HK, Solheim O, Kvistad KA et al (2019) Intraoperative 3D ultrasound-guided resection of diffuse low-grade gliomas: radiological and clinical results. J Neurosurg 132(2):518–529
Berger A, Tzarfati G, Costa M et al (2019) Incidence and impact of stroke following surgery for low-grade gliomas. J Neurosurg.:134(1):153–161
Dhermain F, Barani IJ (2016) Complications from radiotherapy. Handb Clin Neurol 134:219–234
Shaw EG, Wang M, Coons SW et al (2012) Randomized trial of radiation therapy plus procarbazine, lomustine, and vincristine chemotherapy for supratentorial adult low-grade glioma: initial results of RTOG 9802. J Clin oncology: official J Am Soc Clin Oncol 30(25):3065–3070
Pignatti F, van den Bent M, Curran D et al (2002) Prognostic factors for survival in adult patients with cerebral low-grade glioma. J Clin Oncol 20(8):2076–2084
Chang EF, Smith JS, Chang SM et al (2008) Preoperative prognostic classification system for hemispheric low-grade gliomas in adults. J Neurosurg 109(5):817–824
Etxaniz O, Carrato C, de Aguirre I et al (2017) IDH mutation status trumps the Pignatti risk score as a prognostic marker in low-grade gliomas. J Neurooncol 135(2):273–284
Tabrizi S, Yeap BY, Sherman JC et al (2019) Long-term outcomes and late adverse effects of a prospective study on proton radiotherapy for patients with low-grade glioma. Radiother Oncol 137:95–101
Funding
Open access funding provided by University of Gothenburg. The study was financed by grants from the Swedish state under the agreement between the Swedish government and the country councils, the ALF-agreement (ALFGBG-716,671), the Swedish Research Council (2017 − 00944) and the Gothenburg Society of Medicine.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This project was authorized by the regional ethical committee in Sweden, Västra Götaland (DNR 1067-16).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Svenjeby, C., Carstam, L., Werlenius, K. et al. Changes in clinical management of diffuse IDH-mutated lower-grade gliomas: patterns of care in a 15-year period. J Neurooncol 160, 535–543 (2022). https://doi.org/10.1007/s11060-022-04136-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-022-04136-y