Abstract
Background
Salvage of recurrent previously irradiated brain metastases (rBrM) is a significant challenge. Resection without adjuvant re-irradiation is associated with a high local failure rate, while reirradiation only partially reduces failure but is associated with greater radiation necrosis risk. Salvage resection plus Cs131 brachytherapy may offer dosimetric and biologic advantages including improved local control versus observation, with reduced normal brain dose versus re-irradiation, however data are limited.
Methods
A prospective registry of consecutive patients with post-stereotactic radiosurgery (SRS) rBrM undergoing resection plus implantation of collagen-matrix embedded Cs131 seeds (GammaTile, GT Medical Technologies) prescribed to 60 Gy at 5 mm from the cavity was analyzed.
Results
Twenty patients underwent 24 operations with Cs131 implantation in 25 tumor cavities. Median maximum preoperative diameter was 3.0 cm (range 1.1–6.3). Gross- or near-total resection was achieved in 80% of lesions. A median of 16 Cs131 seeds (range 6–30), with a median air-kerma strength of 3.5 U/seed were implanted. There was one postoperative wound dehiscence. With median follow-up of 1.6 years for survivors, two tumors recurred (one in-field, one marginal) resulting in 8.4% 1-year progression incidence (95%CI = 0.0–19.9). Radiographic seed settling was identified in 7/25 cavities (28%) 1.9–11.7 months post-implantation, with 1 case of distant migration (4%), without clinical sequelae. There were 8 cases of radiation necrosis, of which 4 were symptomatic.
Conclusions
With > 1.5 years of follow-up, intraoperative brachytherapy with commercially available Cs131 implants was associated with favorable local control and toxicity profiles. Weak correlation between preoperative tumor geometry and implanted tiles highlights a need to optimize planning criteria.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The treatment of recurrent, previously-irradiated brain metastases (rBrM) is a growing clinical challenge given the increasing survival of many cancer patients with BrM, and the increasing use of stereotactic radiosurgery for this indication [1, 2]. Indeed a growing patient population suffers from disabling or life-limiting CNS-only or CNS-predominant metastases [3, 4].
Salvage treatment paradigms for rBrM are heterogenous, institution-dependent and without an established standard of care. The benefits of adjuvant stereotactic radiosurgery (SRS) after initial surgical metastatectomy is well-established [5, 6]. However, for patients requiring salvage resection for post-SRS recurrence, where the risk of recurrence with surgery alone approximates 40%, adjuvant reirradiation (reRT) carries a greater risk of radiation necrosis (RN) [7]. Thus, adjuvant reRT is commonly withheld or underdosed in this population, likely contributing to suboptimal local control [8].
Brachytherapy, which delivers radiation to surgical cavities’ most superficial margin and thus spares the deeper surrounding, previously-irradiated brain parenchyma, offers an opportunity for adjuvant RT with theoretically better RN risk profile than less-conformal external-beam irradiation if appropriately dosed. Best studied among permanent intracavitary brachytherapy isotopes in the CNS are iodine-125 (I125) and cesium-131 (Cs131). I125 is characterized by higher total deposited dose, more unpredictable dosimetry and a 60-day half-life, which can result in prolonged patient radiation exposure and has been found to carry radiation necrosis rates of around 25% after prior SRS [9, 10]. Cs131 has radiobiological advantages including continuous deposition with a substantially lower half-life of 9.7 days, resulting in reduced deposited dose than I125, and has been described for a variety of primary and metastatic brain tumor applications since FDA approval in 2003. This advantage translates to reductions in theoretical and observed CNS RN rates, versus both I125 and external-beam irradiation in early reports [11, 12].
An initial report using a manually-spaced “seeds on a strand” formulation of Cs131 for rBrM described 83% local control with limited accrual and follow-up [13]. More recently, an FDA-approved, commercially available Cs131 formulation with the radioactive seeds embedded in a conformable collagen carrier has been introduced, with the logistical advantages of more even seed spacing, and thus no need for additional surgical glues or scaffolds to affix the initial construct in place as with the unembedded preparation reported previously.
Initial clinical data using collagen-embedded Cs131 brachytherapy suggest safety and early efficacy for recurrent meningiomas, glioblastomas and a mixed cohort of tumors, but rBrM outcomes have not been detailed [14,15,16]. We describe the first experience using this Cs131 formulation for rBrM and report selection criteria, planning considerations and outcomes, with long-term follow-up.
Methods
Patient inclusion and selection criteria
Following IRB approval, consecutive patients with rBrM who underwent resection plus permanent intracavitary collagen-embedded Cs131 brachytherapy (GammaTile, GT Medical Technologies) were evaluated. At our institution, all patients with suspected rBrM undergo multidisciplinary tumor board review with neurosurgery, radiation oncology, neuro-radiology, neuro-oncology and medical oncology participation, and are evaluated with gadolinium-enhanced MRI and perfusion imaging [17]. In general, recurrent disease is suspected with nodular enhancement, intercurrent growth on two consecutive MRIs, and ≥ 1 advanced imaging modality suggestive of viable tumor over treatment effect (i.e., elevated DCE perfusion or FDG positron emission tomography [PET] if suitable). Systemic cancer-directed treatment is generally suspended perioperatively, particularly with anticipated myelosuppression. In general, myelosuppressive systemic therapy is resumed 2–4 weeks postoperatively, depending on magnitude/rapidity of toxicity.
Cs131 tile implantation
After tumor resection, brachytherapy implantation proceeded after intraoperative frozen section confirmation of viable recurrent disease by a neuropathologist (≥ 5% viable disease in cases with admixed treatment effect/RN). Cs131plaques were rehydrated using sterile saline. Entire resection cavities were covered without gaps, not including overlying dura which is resected with suspected involvement. Per vendor specifications, this orientation is designed to deliver a prescribed dose of 60 Gy at a depth of 5 mm from the cavity assuming the cavity is fully covered with tiles. The delivered dose is not modifiable given the supplied seed strength is determined by the vendor; a higher dose could be delivered if the tiles are surgically oriented in the opposite direction, which brings the embedded Cs131 seeds closer to the exposed cavity wall. Each tile was used whole (4 seeds) or halved (2 seeds) to accommodate smaller or irregularly shaped cavities. Seed strength was confirmed by medical physicists; vendor specifications were used when in-house measurements were within 3% variance, which was the case with all lots to date.
Following tile placement, dura was closed, and skin closed with staples (or absorbable sutures in 3 cases during an acute phase of the COVID-19 pandemic to reduce subsequent patient-caregiver exposure). All patients were treated with routine antibiotic prophylaxis and 2 weeks of levetiracetam prophylaxis for supratentorial resections per standard procedure.
Postimplant dosimetry was performed using a registration of the postoperative-day 1 axial T1 post-contrast MRI and 1 mm-slice thickness CT. A CNS radiation oncologist contoured the surgical cavity and a high risk CTV (HR-CTV) was created as a 5 mm expansion of the surgical bed excluding uninvolved anatomic structures like adjacent cranium [16].
Imaging analysis
Clinical evaluations were performed 2 weeks postoperatively; and at least every 3 months thereafter with concurrent surveillance contrasted MRI. Complications were assessed using CTCAE version 5.0.
MRIs were acquired on 1.5 T or 3 T scanners using consensus brain tumor protocol specifications [18]. Preoperative and all subsequent scans were reviewed for all patients (n = 184 total scans) by a blinded neuroradiologist. The preoperative scan (within 30 days before surgery), postoperative day 1 scan, scan closest to 3 months post procedure, and subsequent scan with the maximal enhancing and non-enhancing lesions after surgery or the last available follow up scan were selected for quantification. The enhancing lesion on contrast T1-weighted images and perilesional T2 hyperintense non-enhancing lesion on fluid-attenuated inversion recovery (FLAIR) images were manually segmented using commercial FDA-approved software (iNtuition ver.4.4.13.P6, TeraRecon, Durham, NC) by a neuroradiologist. Extent of resection was categorized as gross- or near-total resection (GTR/NTR) if > 85% reduction in enhancing volume and otherwise as subtotal (STR) based on prior literature in gliomas and metastases [19,20,21]. Radiation necrosis was defined as postoperative enhancement enlargement > 1 cm3 without suspicion for viable recurrence by blinded neuroradiologist review, and was considered symptomatic with new or worsened referable symptoms.
Statistics
Associations between the number of embedded seeds with the pre- and postoperative tumor diameters, volume, and surface area were calculated using Pearson correlation coefficients. Local failure was determined at the lesion level and defined as evidence of progressive disease (defined per above) within the HR-CTV. Seed settling was determined at the lesion level. Both local failure and seed settling rates were estimated using a cumulative incidence function from the date of Cs131 implant assuming a competing risk of death. Overall survival (OS) was calculated using Kaplan Meier methodology from the date of first resection until death for those with an event or last follow-up for those who were censored. Level of statistical significance was set < 0.05. All tests were two-sided and statistical analyses were performed using SAS v9.4 (SAS Institute, Cary, NC) and R v4.1.3 (The R Foundation for Statistical Computing).
Results
Twenty patients underwent 24 operations with Cs131 implantation in 25 cavities between September 2019 and October 2021 (Table 1). An additional 10 cases with planned Cs131 implantations for suspected rBrM were aborted intraoperatively given < 5% viable disease (n = 5) or cancelled for unrelated reasons (n = 5; 15% each).
Median maximum preoperative diameter was 3.0 cm (range 1.1–6.3), median preoperative enhancing volume was 9.5 cm3 (range 0.6–69.7) and median preoperative surface area was 21.7 cm2 (range 3.4–81.9). All treated lesions had received ≥ 1 prior course of SRS (range 20–30 Gy between 1 and 5 fractions) a median of 358 days preoperatively (range 56–1334) earlier. Eight lesions (32%) had prior single-fraction SRS with doses ranging from 18 to 21 Gy and the remainder hypofractionated SRS of either 8-9 Gy × 3 fractions (n = 9) or 6 Gy × 5 (n = 8). Four had also undergone prior resection or laser ablation. Twenty-three of 25 implanted lesions had elevated DCE perfusion characteristics on preoperative MRI. Six lesions also were evaluated with FDG PET prior to resection, of these, 4 (66%) were FDG avid.
Seed requirement
For the 25 cavities successfully implanted, 156 tiles were pre-ordered and 114 were ultimately implanted, reflecting a wastage rate of 26.9%. A median of 16 Cs131 seeds (range 6–30) per lesion, with a median air-kerma strength of 3.5 U/seed (and variance of 0.09 U) were implanted. In one case, seeds were implanted one day earlier with a corresponding strength of 3.81 U/seed and dose of 65.3 Gy at 5 mm from the cavity surface (this case was not subsequently necrotic or recurrent). Preoperative surface area, maximal diameter and enhancing volume were weakly associated with the number of ultimately implanted seeds (correlation coefficients = 0.49, 0.50, and 0.41, respectively).
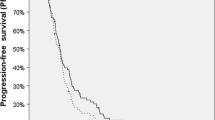
Clinical outcomes
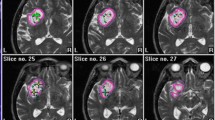
With median follow-up for survivors of 1.6 years (range 0.6–2.1), 2 local recurrences were identified resulting in a 1-year local progression incidence of 8.4% (95%CI 0.0–19.9, Fig. 1). This included patients with large recurrences with radioresistant histology and multiple prior local treatments, including 1 patient with renal cell carcinoma who progressed through laser interstitial thermal therapy (LITT) and SRS as previously reported (Fig. 2A) [22]. The local recurrence was in a gross-totally removed 3.0 × 2.8 cm ALK-rearranged solitary lung cancer brain metastasis that recurred 7.5 months following SRS (21 Gy). Eleven months later, nodular enhancement with elevated perfusion was identified along the anterioinferior edge of the resection cavity, partially within and marginal to the HD-CTV which did not receive the full 60 Gy prescription dose and fell within the 50% isodose line of 30 Gy. The patient was neurologically stable with well-controlled extracranial disease. This marginal relapse was recently treated with salvage hypofractionated SRS (27 Gy in 3 fractions).
Three representative rBrM case examples with columns from left to right delineating pre-operative T1 post contrast MRI (T1 + G), immediate post-operative MRI, dosimetry, post-implant T1 post contrast MRI showing either local control or suspected relapse and DCE (dynamic contrast-enhanced) perfusion imaging corresponding to that same post-implant MRI scan. A Recurrent parietal rectal cancer metastasis after prior hypofractionated SRS (8 Gy × 3) showing durable control with no evidence of tumor recurrence 17 months post implantation. Of note, the dosimetry is set to show 95% of the prescription dose or higher. B Recurrent temporal non small cell lung cancer brain metastasis after prior 21 Gy × 1 showing hyperperfusing recurrence within and marginal to the HR-CTV 11 months post-operatively (blue dotted box). Of note, for the Cs131 dosimetry, the thin yellow line delineates the HR-CTV. For the upper panel, the dosimetry shows 95% of the prescription dose or higher. In the enlarged lower panel, the 30 Gy (i.e., 50% isodose line) and 60 Gy (i.e., 100% isodose line) are shown in blue and red, respectively. C Recurrent parietal renal cell carcinoma metastasis after previous hypofractionated SRS (6 Gy × 5) showing enhancement in the surgical cavity with subtle hyperperfusion at 10 months post implant suspicious for viable tumor mixed with necrosis (blue dotted box)
The second relapse was a 3.4 × 1.5 cm left frontoparietal tumor renal cell carcinoma metastasis that recurred 44.5 months after hypofractionated SRS (30 Gy in 5 fractions) (Fig. 2C). Pathology showed admixed viable tumor and necrosis. Mildly hyperperfusing nodular enhancement was identified 10 months post-implantation along the surgical cavity suggestive of viable recurrence (likely with mixed RN). He was managed with dexamethasone for symptomatic RN and subsequently observed over the ensuing 5 months with mild change. More recently, he received addition SRS for distant brain progression.
One-year cumulative incidence of overall intracranial progression was 41.1% (95%CI 20.9–61.3); corresponding to the 2 above local/regional index-site progression plus 13 cases with new or progressing pre-existing distant sites of disease within the brain. One year OS was 64.0% (95%CI 45.8–89.4); median OS was not reached.
Detailed analysis of post-implant imaging
T1 post-contrast enhancement
Following implantation, increased enhancement versus the immediate postoperative scan was seen in 19/23 evaluable lesions at 3 months postoperatively (83%; 95%CI 61.2–95.0). However, morphologic features and perfusion characteristics were not suggestive of viable disease in any case at this time point, and the patients were managed with the assumption this was treatment effect with dexamethasone used as needed for symptoms. Two such lesions were eventually deemed radiographically concerning for recurrent disease by multidisciplinary consensus and reflect the two aforementioned local progression events.
T2 FLAIR
Median baseline preoperative FLAIR volume was 48.1 cm3 (range 7.0–231.6). At 3 months 23/24 evaluable lesions had a reduction in the quantitative volumetric edema with an average reduction of 56.0% (Supplemental Fig. 1).
Post-implant radiation necrosis and wound toxicity
There were 8 cases (32%) of radiographic radiation necrosis of which 4 (50%) were assessed to be symptomatic after retrospective multidisciplinary review. One of these lesions had previously received single-fraction SRS to a total dose of 21 Gy and the remaining 7 lesions received hypofractionated SRS.
There was 1 case of wound dehiscence in a high-risk patient with multiple prior RT courses, and prior resection complicated by pseudomeningocele. The patient required CSF shunting and wound revision for CSF leak and intracranial hypertension. There was 1 postoperative seizure in a patient with prior seizures, that was controlled with anti-epileptic medications.
Stability of tile/seed positioning post-implantation
Seven treated cavities (28%) were found to have asymptomatic change in seed position at a median 6.3 months postoperatively (range 1.9–11.7), most often into a dependent position (n = 6) with half into a discrete cluster, and less commonly, a fall from a single cavity wall (n = 1), for a 1-year cumulative incidence of 28.8% (95% CI 10–2-47.3).
One patient with ventricular communication with the resection cavity was found to have a single seed migrate into the adjacent occipital horn of the lateral ventricle at 3.6 months, and further migration of that single seed into the infundibular recess of the third ventricle at 5.9 months postoperatively, at which point no meaningful radioactivity remained due to the isotope’s relatively short half-life [Fig. 3].
Illustrative case example of seed position change after implantation. A T2 MRI and B Thin slice CT showing original position of the Cs131 brachytherapy seeds on postoperative day 1 apposed to the anterior, posterior and medial resection cavity walls. C T2 MRI from 3.7 months post-implant which reveals clumping of the tiles/seeds along the inferior cavity wall (and no longer apposing the medial edge). D T2 MRI from 5 months post-implant which shows migration of these seeds with clustering in the inferior medial margin of the surgical cavity. E Sagittal contrast-enhanced T1 MRI shows a single hypointense seed in the infundibular recess of the 3rd ventricle, which is confirmed on F axial non-contrast CT as metallic density. Yellow arrows point to Cs131 seeds
Discussion
We describe the application of commercially available collagen-embedded Cs131 for previously-irradiated rBrM. This is an area of significant unmet need given historically poor control with surgery alone and the potential toxicity of repeat SRS. In one of the largest reported series of rBrM treated with repeat SRS, 30 patients with a median brain tumor volume of 4.8 cc experienced a suboptimal 1-year local control rate of 68%, with associated toxicities including edema (13%), RN (10%) and hemorrhage (13%), all in tumors of > 7 cc volume [23]. Others report similarly low 1-year local control rates of approximately 61–68% at even smaller tumor volumes [24, 25]. Recurrent tumors requiring surgical resection are an even bigger challenge to salvage: these are often significantly larger (typically ≥ 2.5 cm in diameter or > 8 cm3 in volume, and in our current series approximately 9.5 cm3), and local failure is size-dependent with larger tumor volumes associated with higher recurrence rates [26]. Indeed, the largest salvage surgical experience identified a 40% 1-year local recurrence rate in 155 rBrM, with a trend towards improved but still suboptimal, local control with adjuvant reirradiation versus observation (29% vs. 44%, p = 0.07 by multivariate analysis)[7].
While these data support using adjuvant reirradiation for local control, the tradeoff lies in balancing radiotoxicity. Some series suggest high 1 year symptomatic RN rates with reRT in almost 30% of patients [27]. In one surgical series describing resection and reRT of rBrM, 13% developed symptomatic RN (grade 2 RN with grade 3 seizures or grade 3 RN) at a median follow-up of only 9 months at which time 2/3 of patients were deceased [8]. In Wilcox et al., the radiographic RN rate at 1 year was 13.4% with a symptomatic RN rate of 5.1% [7]. Thus, in our practice, gross-totally removed post-irradiation rBrM typically do not receive reRT until additional local failure due to this perceived significant rate of external-beam radiotoxicity. We thus sought to define the role for Cs131 brachytherapy as part of a programmatic salvage strategy for rBrM incorporating LITT for deep/unresectable tumors below 2.5 cm in diameter or for poor open-surgical candidates, and salvage resection for larger, superficial, and tumors near/involving high-eloquence circuitry.
We selected Cs131 for this population given early reported Cs131 efficacy for rBrM both in the upfront and salvage (previously-irradiated) settings [14, 28]. Prior studies have yielded early enthusiasm for Cs131 in a “seeds-on-a-strand” formulation with different seed strengths, following salvage rBrM resection. Wernicke et al. demonstrated 83% 1-year actuarial freedom from local progression in 13 patients with 15 previously-irradiated rBrM (previously treated with SRS or whole-brain radiotherapy) treated with Cs131 prescribed to 80 Gy to 5 mm depth, with limited follow-up of 5 months [13]. Toxicity at this higher prescription dose included 4 postoperative infections/pseudomeningoceles, 2 new-onset seizures, 1 case of asymptomatic RN, 1 infection 7 months postoperatively, and seed migration in 1 case (in which fibrin glue was used). Chen et al. also reported on “strands on a seed” Cs131, at the higher prescription dose of 80 Gy to 5 mm, for a spectrum of histologies including 22 recurrent metastases of which not all were previously irradiated, and without uniform reporting on prior local treatment histories; this treatment was associated with an 11.2% 1-year local failure rate [29].
The collagen matrix-embedded formulation described in this study allows for rapid, evenly spaced placement of brachytherapy apposed to resection cavity walls. This tile-embedded form factor, similar to historical gelfoam-embedded I125 formulations, may also theoretically help maintain the overall shape of the implant and cavity during the dose-deposition period [30, 31]. This formulation has been described to be associated with a 10% surgical complication rate and 10% rate of RN, in recurrent meningiomas with limited follow-up [14].
Our finding of durable local control with approximately 10% failure cumulative incidence (of which 1 of 2 cases was asymptomatic and has not yet required retreatment with 5 months of follow up) for this difficult-to-treat salvage population with large tumors compares favorably to the aforementioned historical cohorts with both observation and reRT, which carry failure rates of up to 40% [7]. This larger study corroborates control outcomes from the prior non-embedded reports, despite three-times longer follow-up for the earlier report; this follow-up duration is more representative of the modern 18-month median survival of brain metastasectomy patients (Table 2) [32]. Reflective of the high-risk population, iPFS was more modest, underscoring that such salvage approaches are most successful in well-selected patients and as part of a broader multi-modality strategy for example with CNS-penetrant cancer-directed therapies able to prevent further brain progression. Wound outcomes were generally good, and implants were previously shown to not be associated with concerning radiation exposure to patients, caregivers or providers [33]. Further, we identified decreased tumor-associated edema at 3 months post-operatively in line with the known benefits of palliative resection of brain metastases in other contexts [34]. Our symptomatic radiation necrosis rate of 15–20% is on par with other accepted approaches for retreatment of rBrM, though still suboptimal [7]. We have limited power to assess for associations between prior SRS doses or prior resection/LITT and post-brachytherapy radiation necrosis. Most of the lesions which developed radiation necrosis in our series had prior hypofractionated SRS which we suspect is a surrogate for larger lesional size, and which is a known predictor of radiation necrosis risk.
We identify several key areas for future research. Increased enhancement was seen in most patients post-implantation, representing treatment effect in a majority of cases, as corroborated by DCE perfusion/FDG PET or subsequent resolution [35]. Better correlates of subsequent recurrence or symptomatic RN are needed for this population, but also for all post-radiation brain metastases. Despite multidisciplinary expert review and advanced imaging suggestive of recurrent disease for all cases, patient selection remained challenging, with over one-quarter of patients ultimately found to not harbor viable tumor, despite a relatively liberal (though evidence-based) 5% viability threshold for implantation[7, 36]. The specific benefit of Cs131 brachytherapy for patients with purely recurrent tumor vs. < 100% viable disease remains unclear, though we did not identify an increased rate of changes in post-operative enhancement by viability-necrosis proportions, within the limited powering of this experience.
Seed ordering estimates require better prognostic models. The relatively high implant-wastage rate has implications for the healthcare system given the high incremental cost of this technology. Better predictive models potentially incorporating radiomics may assist in this work. In addition, as there may be a learning curve with this as with any procedural adjunct, future study should evaluate the role of user experience on outcomes.
Finally, we identify a high rate of Cs131 seed settling 1.9–11.7 months postoperatively, corresponding to the known disintegration timeframe of collagen at 3–6 months, and a case of distant migration. While we did not identify any patient harm, and do not foresee off-site radioactivity danger given the majority of biologically relevant dose is deposited by 40 days (approximately 4 half-lives), this phenomenon requires attention in all implanted cases and particularly intra- and para-ventricular cavities, given the potential risk of aqueductal obstruction.
Randomized prospective study is necessary to eliminate potential selection bias and provide additional powering to establish more definitive safety and efficacy data for this indication. The accruing phase II study randomizing salvage resection of rBrM with or without Cs131 brachytherapy (NCT04690348) will help fill this gap.
Conclusions
Salvage intracavitary Cs131 implantation was associated with a favorable control rate and toxicity profile in large recurrent rBrM. This paradigm is also associated with significantly improved tumor-associated edema, though delayed seed settling and rare migration requires clinician awareness.
Change history
23 August 2022
A Correction to this paper has been published: https://doi.org/10.1007/s11060-022-04121-5
References
Löscher W, Potschka H (2005) Blood-brain barrier active efflux transporters: ATP-binding cassette gene family. NeuroRx 2:86–98. https://doi.org/10.1602/neurorx.2.1.86
Barbour AB, Jacobs CD, Williamson H et al (2020) Radiation therapy practice patterns for brain metastases in the United States in the stereotactic radiosurgery era. Adv Radiat Oncol 5:43–52. https://doi.org/10.1016/j.adro.2019.07.012
O’Connell K, Romo CG, Grossman SA (2019) Brain metastases as a first site of recurrence in patients on chemotherapy with controlled systemic cancers: an increasingly urgent clinical scenario. J Clin Oncol 37:e13590–e13590. https://doi.org/10.1200/JCO.2019.37.15_suppl.e13590
Ebner DK, Gorovets D, Rava P et al (2017) Patients with long-term control of systemic disease are a favorable prognostic group for treatment of brain metastases with stereotactic radiosurgery alone. World Neurosurg 98:266–272. https://doi.org/10.1016/j.wneu.2016.11.010
Brennan C, Yang TJ, Hilden P et al (2014) A phase 2 trial of stereotactic radiosurgery boost after surgical resection for brain metastases. Int J Radiat Oncol 88:130–136. https://doi.org/10.1016/j.ijrobp.2013.09.051
Mahajan A, Ahmed S, McAleer MF et al (2017) Post-operative stereotactic radiosurgery versus observation for completely resected brain metastases: a single-centre, randomised, controlled, phase 3 trial. Lancet Oncol 18:1040–1048. https://doi.org/10.1016/S1470-2045(17)30414-X
Wilcox JA, Brown S, Reiner AS et al (2021) Salvage resection of recurrent previously irradiated brain metastases: tumor control and radiation necrosis dependency on adjuvant re-irradiation. J Neurooncol 155:277–286. https://doi.org/10.1007/s11060-021-03872-x
Holt DE, Gill BS, Clump DA et al (2015) Tumor bed radiosurgery following resection and prior stereotactic radiosurgery for locally persistent brain metastasis. Front Oncol 5:84. https://doi.org/10.3389/fonc.2015.00084
Wernicke AG, Lazow SP, Taube S et al (2016) Surgical technique and clinically relevant resection cavity dynamics following implantation of cesium-131 (Cs-131) brachytherapy in patients with brain metastases. Oper Neurosurg 12:49–60. https://doi.org/10.1227/NEU.0000000000000986
Raleigh DR, Seymour ZA, Tomlin B et al (2016) Resection and brain brachytherapy with permanent iodine-125 sources for brain metastasis. J Neurosurg 126:1749–1755. https://doi.org/10.3171/2016.4.JNS152530
Mahase SS, Navrazhina K, Schwartz TH et al (2019) Intraoperative brachytherapy for resected brain metastases. Brachytherapy 18:258–270. https://doi.org/10.1016/j.brachy.2019.01.011
Chitti B, Goyal S, Sherman JH et al (2020) The role of brachytherapy in the management of brain metastases: a systematic review. J Contemp Brachytherapy 12:67–83. https://doi.org/10.5114/jcb.2020.93543
Wernicke AG, Smith AW, Taube S et al (2017) Cesium-131 brachytherapy for recurrent brain metastases: durable salvage treatment for previously irradiated metastatic disease. J Neurosurg 126:1212–1219. https://doi.org/10.3171/2016.3.JNS152836
Brachman DG, Youssef E, Dardis CJ et al (2018) Resection and permanent intracranial brachytherapy using modular, biocompatible cesium-131 implants: results in 20 recurrent, previously irradiated meningiomas. J Neurosurg 131:1819–1828. https://doi.org/10.3171/2018.7.JNS18656
Data on file (2019), GT Medical Technologies, Inc, and presented at the American Association of Neurological Surgeons.
Gessler DJ, Neil EC, Shah R et al (2022) GammaTile® brachytherapy in the treatment of recurrent glioblastomas. Neuro-Oncol Adv. https://doi.org/10.1093/noajnl/vdab185
Moss NS, Beal K, Tabar V (2022) Brain metastasis-a distinct oncologic disease best served by an integrated multidisciplinary team approach. JAMA Oncol. https://doi.org/10.1001/jamaoncol.2022.1928
Ellingson BM, Bendszus M, Boxerman J et al (2015) Consensus recommendations for a standardized brain tumor imaging protocol in clinical trials. Neuro-Oncol 17:1188–1198. https://doi.org/10.1093/neuonc/nov095
Jünger ST, Pennig L, Schödel P et al (2021) The debatable benefit of gross-total resection of brain metastases in a comprehensive treatment setting. Cancers 13:1435. https://doi.org/10.3390/cancers13061435
Kiesel B, Prihoda R, Borkovec M et al (2020) Postoperative magnetic resonance imaging after surgery of brain metastases: analysis of extent of resection and potential risk factors for incomplete resection. World Neurosurg 143:e365–e373. https://doi.org/10.1016/j.wneu.2020.07.150
Karschnia P, Vogelbaum MA, van den Bent M et al (2021) Evidence-based recommendations on categories for extent of resection in diffuse glioma. Eur J Cancer 149:23–33. https://doi.org/10.1016/j.ejca.2021.03.002
Yu KKH, Imber BS, Moss NS (2021) Multimodality durable salvage of recurrent brain metastases refractory to LITT, SRS and immunotherapy with resection and cesium-131 brachytherapy: case report and literature review. BMJ Case Rep CP 14:e245369. https://doi.org/10.1136/bcr-2021-245369
Moreau J, Khalil T, Dupic G et al (2018) Second course of stereotactic radiosurgery for locally recurrent brain metastases: safety and efficacy. PLoS ONE 13:e0195608. https://doi.org/10.1371/journal.pone.0195608
Koffer P, Chan J, Rava P et al (2017) Repeat stereotactic radiosurgery for locally recurrent brain metastases. World Neurosurg 104:589–593. https://doi.org/10.1016/j.wneu.2017.04.103
Iorio-Morin C, Mercure-Cyr R, Figueiredo G et al (2019) Repeat stereotactic radiosurgery for the management of locally recurrent brain metastases. J Neurooncol. https://doi.org/10.1007/s11060-019-03323-8
Churilla TM, Chowdhury IH, Handorf E et al (2019) Comparison of local control of brain metastases with stereotactic radiosurgery vs surgical resection: a secondary analysis of a randomized clinical trial. JAMA Oncol 5:243–247. https://doi.org/10.1001/jamaoncol.2018.4610
McKay WH, McTyre ER, Okoukoni C et al (2017) Repeat stereotactic radiosurgery as salvage therapy for locally recurrent brain metastases previously treated with radiosurgery. J Neurosurg 127:148–156. https://doi.org/10.3171/2016.5.JNS153051
Nakaji P, Smith K, Youssef E et al (2020) Resection and surgically targeted radiation therapy for the treatment of larger recurrent or newly diagnosed brain metastasis: results from a prospective trial. Cureus 12:e11570. https://doi.org/10.7759/cureus.11570
Chen WC, Lafreniere M, Phuong C et al (2022) Resection with intraoperative cesium-131 brachytherapy as salvage therapy for recurrent brain tumors. J Neurosurg. https://doi.org/10.3171/2021.10.JNS211886
Gutin PH, Leibel SA, Hosobuchi Y et al (1987) Brachytherapy of recurrent tumors of the skull base and spine with iodine-125 sources. Neurosurgery 20:938–945. https://doi.org/10.1227/00006123-198706000-00020
Nori D, Li X, Pugkhem T (1995) Intraoperative brachytherapy using gelfoam radioactive plaque implants for resected stage iii non-small cell lung cancer with positive margin: a pilot study. J Surg Oncol 60:257–261. https://doi.org/10.1002/jso.2930600409
Bander ED, Yuan M, Reiner AS et al (2021) Durable 5-year local control for resected brain metastases with early adjuvant SRS: the effect of timing on intended-field control. Neuro-Oncol Pract 8:278–289. https://doi.org/10.1093/nop/npab005
Moss NS, Imber BS, Prasad K et al (2020) Permanent intracavitary Cs131 brachytherapy for previously-irradiated recurrent brain metastases: initial clinical and radiation safety experience. Neuro-Oncol Adv. https://doi.org/10.1093/noajnl/vdaa073.056
Newman WC, Goldberg J, Guadix SW et al (2021) The effect of surgery on radiation necrosis in irradiated brain metastases: extent of resection and long-term clinical and radiographic outcomes. J Neurooncol 153:507–518. https://doi.org/10.1007/s11060-021-03790-y
Furuse M, Nonoguchi N, Yamada K et al (2019) Radiological diagnosis of brain radiation necrosis after cranial irradiation for brain tumor: a systematic review. Radiat Oncol 14:28. https://doi.org/10.1186/s13014-019-1228-x
Barajas RF, Chang JS, Segal MR et al (2009) Differentiation of recurrent glioblastoma multiforme from radiation necrosis after external beam radiation therapy with dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging. Radiology 253:486–496. https://doi.org/10.1148/radiol.2532090007
Author information
Authors and Affiliations
Contributions
BSI and NM wrote the main manuscript text. BSI, RJY, KB, AGL, JTY, DAN, GC, CB, VT and NSM collected data. ASR performed the statistical analyses. ASR prepared figures 1 and 3. BSI prepared figure 2, and BSI and RJY prepared figure 4. FDG PET data was collected by Dr Simone Krebs. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Funding
This research was funded in part through the NIH/NCI Cancer Center Support Grant P30 CA008748. BSI reports an honorarium from GT Medical Technologies. NSM is PI of an investigator-initiated trial funded by GT Medical Technologies.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Previous presentations: This work has not been submitted for consideration in part or in whole to another journal to date. It has been partially presented including orally at the AANS annual meeting in May 2022, and will be presented as a podium talk the Society of Neuro-Oncology Brain Metastasis and Clinical Trials meeting in August 2022.
The original version of this article has been revised: A new author has been added as the 6th author.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Imber, B.S., Young, R.J., Beal, K. et al. Salvage resection plus cesium-131 brachytherapy durably controls post-SRS recurrent brain metastases. J Neurooncol 159, 609–618 (2022). https://doi.org/10.1007/s11060-022-04101-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-022-04101-9