Abstract
Purpose
Discordant prognostic awareness (PA) can cause distress, impact goals of care and future planning, especially in patients with high grade glioma (pwHGG) who have limited survival. We aimed to evaluate the feasibility of assessing PA of pwHGG, caregivers and clinicians using a single question and to evaluate these responses for discord, alignment and fluctuation over time.
Methods
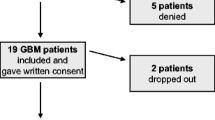
This is a sub-study of an IRB-approved pilot study evaluating early palliative care and longitudinal symptom monitoring via a smart-device tool in 16 pwHGG and their caregivers receiving treatment at the Mayo Clinic Arizona (United States). Eligible patients were ≥ 18 years, English-speaking, newly-diagnosed, and had a willing caregiver. Participants answered a multiple-choice question asking for an estimate of their own or their loved one’s survival on a monthly basis.
Results
All except one patient/caregiver dyad answered the question each time it was asked. The question did not appear to cause discomfort or increase conversations with clinicians around prognosis. PA of patients and caregivers fluctuated monthly, ranging from dismal to overtly optimistic, with a discordance frequency of 68%. Patients tended to be more optimistic than caregivers, and a higher QOL correlated to a more optimistic response. Clinicians’ were more hopeful; their prediction tended to fluctuate less than those of patients and caregivers.
Conclusions
PA may be assessed in pwHGG and caregivers with a single, frank question. There is clear discordance between PA of patients, their caregivers and clinicians. Understanding fluctuates longitudinally through disease and treatment course. Additional studies on timing and ways of discussing prognosis in this population are needed.
Clinical Trial Registration
NCT04630379.





Similar content being viewed by others
Data availability
The datasets generated during and analyzed during the study are not publicly available due to concern that the detailed nature of the information may compromise confidentiality of the participants. In addition, patients and caregivers may not want the other party to see their own responses to various questions. The datasets are therefore available from the corresponding author on reasonable request.
References
Stupp R et al (2009) Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol 10(5):459–466. https://doi.org/10.1016/S1470-2045(09)70025-7 (in eng)
Bent MJVD et al (2019) Second interim and first molecular analysis of the EORTC randomized phase III intergroup CATNON trial on concurrent and adjuvant temozolomide in anaplastic glioma without 1p/19q codeletion. J Clin Oncol 37(15):2000–2000. https://doi.org/10.1200/JCO.2019.37.15_suppl.2000
Davies E, Clarke C (2004) Early symptoms of brain tumours. J Neurol Neurosurg Psychiatry 75(8):1205–1206. https://doi.org/10.1136/jnnp.2003.033308 (in eng)
Halkett GK, Lobb EA, Oldham L, Nowak AK (2010) The information and support needs of patients diagnosed with High Grade Glioma. Patient Educ Couns 79(1):112–119. https://doi.org/10.1016/j.pec.2009.08.013 (in eng)
Janda M, Steginga S, Dunn J, Langbecker D, Walker D, Eakin E (2008) Unmet supportive care needs and interest in services among patients with a brain tumour and their carers. Patient Educ Couns 71(2):251–258. https://doi.org/10.1016/j.pec.2008.01.020 (in eng)
Fried TR, Bradley EH, O’Leary J (2003) Prognosis communication in serious illness: perceptions of older patients, caregivers, and clinicians. J Am Geriatr Soc 51(10):1398–1403. https://doi.org/10.1046/j.1532-5415.2003.51457.x (in eng)
Nipp RD et al (2017) Coping and prognostic awareness in patients with advanced cancer. J Clin Oncol 35(22):2551–2557. https://doi.org/10.1200/JCO.2016.71.3404 (in eng)
Lobb EA, Halkett GK, Nowak AK (2011) Patient and caregiver perceptions of communication of prognosis in high grade glioma. J Neurooncol 104(1):315–322. https://doi.org/10.1007/s11060-010-0495-z (in eng)
The AM, Hak T, Koëter G, van der Wal G (2001) Collusion in doctor-patient communication about imminent death: an ethnographic study. West J Med 174(4):247–253. https://doi.org/10.1136/ewjm.174.4.247 (in eng)
Lamont EB, Christakis NA (2001) Prognostic disclosure to patients with cancer near the end of life. Ann Intern Med 134(12):1096–1105. https://doi.org/10.7326/0003-4819-134-12-200106190-00009 (in eng)
Golden JS, Johnston GD (1970) Problems of distortion in doctor-patient communications. Psychiatry Med 1(2):127–149. https://doi.org/10.2190/5ucc-9pnh-qpw0-y2wr (in eng)
McConigley R, Halkett G, Lobb E, Nowak A (2010) Caring for someone with high-grade glioma: a time of rapid change for caregivers. Palliat Med 24(5):473–479. https://doi.org/10.1177/0269216309360118 (in eng)
Fallowfield LJ, Jenkins VA, Beveridge HA (2002) Truth may hurt but deceit hurts more: communication in palliative care. Palliat Med 16(4):297–303. https://doi.org/10.1191/0269216302pm575oa (in eng)
Ridgeway JL et al (2013) A brief Patient-Reported Outcomes Quality of Life (PROQOL) instrument to improve patient care. PLoS Med 10(11):e1001548. https://doi.org/10.1371/journal.pmed.1001548 (in eng)
Locke DE et al (2007) Validation of single-item linear analog scale assessment of quality of life in neuro-oncology patients. J Pain Symptom Manag 34(6):628–638. https://doi.org/10.1016/j.jpainsymman.2007.01.016 (in eng)
Diamond EL et al (2017) Prognostic awareness, prognostic communication, and cognitive function in patients with malignant glioma. Neuro Oncol 19(11):1532–1541. https://doi.org/10.1093/neuonc/nox117 (in eng)
Applebaum AJ et al (2018) Prognostic awareness and communication preferences among caregivers of patients with malignant glioma. Psychooncology 27(3):817–823. https://doi.org/10.1002/pon.4581 (in eng)
Davies E, Clarke C, Hopkins A (1996) Malignant cerebral glioma–II: perspectives of patients and relatives on the value of radiotherapy. BMJ 313(7071):1512–1516. https://doi.org/10.1136/bmj.313.7071.1512 (in eng)
Salander P, Spetz A (2002) How do patients and spouses deal with the serious facts of malignant glioma? Palliat Med 16(4):305–313 (in eng)
Sizoo EM et al (2012) Decision-making in the end-of-life phase of high-grade glioma patients. Eur J Cancer 48(2):226–232. https://doi.org/10.1016/j.ejca.2011.11.010 (in eng)
Sharma A, Graber JJ (2020) Overview of prognostic factors in adult gliomas. Ann Palliat Med 9(6):37
Quill TE (2000) Perspectives on care at the close of life. initiating end-of-life discussions with seriously ill patients: addressing the “elephant in the room.” JAMA 284(19):2502–2507. https://doi.org/10.1001/jama.284.19.2502 (in eng)
Triebel KL, Martin RC, Nabors LB, Marson DC (2009) Medical decision-making capacity in patients with malignant glioma. Neurology 73(24):2086–2092. https://doi.org/10.1212/WNL.0b013e3181c67bce (in eng)
Diamond EL et al (2016) Rates and risks for late referral to hospice in patients with primary malignant brain tumors. Neuro Oncol 18(1):78–86. https://doi.org/10.1093/neuonc/nov156 (in eng)
A. Sharma and L. P. Taylor(2019), "Malignant Brain Tumors," In Neuropalliative Care, C. J. Creutzfeldt, B. M. Kluger, and R. G. Holloway (Eds)., 1 ed.: Springer International Publishing,.
Back AL, Arnold RM (2006) Discussing prognosis: “how much do you want to know?” talking to patients who do not want information or who are ambivalent. J Clin Oncol 24(25):4214–4217. https://doi.org/10.1200/JCO.2006.06.008 (in eng)
Hagerty RG et al (2005) Communicating with realism and hope: incurable cancer patients’ views on the disclosure of prognosis. J Clin Oncol 23(6):1278–1288. https://doi.org/10.1200/JCO.2005.11.138 (in eng)
Childers JW, Back AL, Tulsky JA, Arnold RM (2017) REMAP: a framework for goals of care conversations. J Oncol Pract 13(10):e844–e850. https://doi.org/10.1200/JOP.2016.018796 (in eng)
Childers JW, White DB, Arnold R (2020) “Has anything changed since then?”: a framework to incorporate prior GOC conversations into decision making for acutely ill patients. J Pain Symptom Manag. https://doi.org/10.1016/j.jpainsymman.2020.10.030 (in eng)
Christakis NA, Lamont EB (2000) Extent and determinants of error in doctors’ prognoses in terminally ill patients: prospective cohort study. BMJ 320(7233):469–472. https://doi.org/10.1136/bmj.320.7233.469 (in eng)
Temel JS et al (2011) Longitudinal perceptions of prognosis and goals of therapy in patients with metastatic non-small-cell lung cancer: results of a randomized study of early palliative care. J Clin Oncol 29(17):2319–2326. https://doi.org/10.1200/JCO.2010.32.4459 (in eng)
Acknowledgements
We are extremely grateful to our patients and their caregivers who participated in this study and its parent trial. We appreciate the support of Dr Jan Buckner and would also like to thank Mr. Eric Wolfe for his help with developing the survey tool. Our gratitude to our study coordinators at MCA, Ms. Ashley Napier and Ms. Regina Becker.
Funding
This study was awarded funds from the Richard J and Barbara E Franke Fund for research in Palliative Care from the Mayo Clinic.
Author information
Authors and Affiliations
Contributions
AS conceptualized and designed the study, wrote the IRB application and protocol, was involved in data collection and analysis, and drafted the manuscript. BF provided statistical support with data review and analysis, created figures, and wrote the statistical sections of the manuscript. CB provided palliative care insight for the study design and execution, provided palliative care to patients on Group B, was involved in data collection, and reviewed the final manuscript. HNF provided palliative care to the patients in Group B and was involved in data collection. MMM provided neuro-oncology insight for the study design and execution, provided neuro-oncological care to patients in all groups, was involved in data collection, and reviewed/edited the final manuscript. ME provided palliative care insight and support for study design and execution, provided palliative care to patients in Group B, and reviewed the final manuscript. JS designed the Beacon application that was used for the trial, assisted with study design and provided statistical support. AP was the faculty primary investigator, helped with conceptualization and study design, reviewed the protocol and IRB application, was involved in data collection, provided neuro-oncological care to patients in all groups, and was involved with major revisions and editing of the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant conflicts of interests or disclosures.
Ethical approval
The study was granted IRB approval from Mayo Clinic Arizona.
Informed Consent
All patients and their caregivers were provided with an informed consent which the study coordinator reviewed with them. Informed consent was obtained from all individual participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sharma, A., Fruth, B., Barrera, C. et al. How much time do we have? Longitudinal perception of prognosis in newly-diagnosed high grade glioma patients and caregivers compared to clinicians. J Neurooncol 152, 313–323 (2021). https://doi.org/10.1007/s11060-021-03700-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-021-03700-2