Abstract
Introduction
Pediatric spinal tumors are unique pathologies treated by pediatric neurosurgeons. Special attention is required for the preservation of neural function and bony alignment. We reported our experience in the management of these challenging lesions.
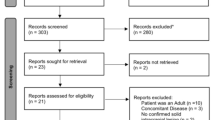
Methods
A total of 75 pediatric patients with spinal tumors treated at the National Taiwan University Hospital from 1998 to 2018 were identified retrospectively. Clinical data, radiographic image, and pathological report were reviewed for analysis.
Results
There were 37 females and 38 males. The median age was 9 years. Thirty-eight tumors (50.6%) were extradural, 20 (26.7%) intradural extramedullary, and 17 (22.6%) intramedullary. The most common pathologies were glioma, ependymoma, and neuroblastoma. The rate of total and subtotal resection was 45.3% and 21.3%. Thirty-four patients (45.3%) required post-operative adjuvant therapy. Eight patients (10.6%) with spinal deformity had simultaneous tumor excision and spinal fusion surgery. Additional six (8%) patients had subsequent spinal fixation and fusion for deformity after primary tumor operation. Eighty-four percent of patients were ambulatory 3 years after operation. For patients with intradural extramedullary and intramedullary tumors, worse survival outcome was associated with tumor derived from CSF seeding and cranial involvement of spinal tumor, while poorer functional outcome was correlated with cranial involvement and adjuvant therapy with chemotherapy or radiotherapy.
Conclusions
Pediatric spinal tumor surgery carries low surgical morbidity and mortality under current standard of neurosurgical practice. Post-operative adjuvant therapy is required for nearly half of the cases. Spinal deformity requires special attention and sometimes surgical correction. Contemporary management of pediatric spinal tumors enables effective ablation of the lesion and delivers favorable outcome for the majority of patients.

Similar content being viewed by others
References
Ostrom QT, de Blank PM, Kruchko C, Petersen CM, Liao P, Finlay JL, Stearns DS, Wolff JE, Wolinsky Y, Letterio JJ, Barnholtz-Sloan JS (2015) Alex's Lemonade stand foundation infant and childhood primary brain and central nervous system tumors diagnosed in the United States in 2007–2011. Neuro Oncol 16(Suppl 10):x1–x36. https://doi.org/10.1093/neuonc/nou327
McGirt MJ, Chaichana KL, Atiba A, Attenello F, Woodworth GF, Jallo GI (2008) Neurological outcome after resection of intramedullary spinal cord tumors in children. Child's Nerv Syst 24:93–97. https://doi.org/10.1007/s00381-007-0446-y
Garces-Ambrossi GL, McGirt MJ, Mehta VA, Sciubba DM, Witham TF, Bydon A, Wolinksy JP, Jallo GI, Gokaslan ZL (2009) Factors associated with progression-free survival and long-term neurological outcome after resection of intramedullary spinal cord tumors: analysis of 101 consecutive cases. J Neurosurg Spine 11:591–599. https://doi.org/10.3171/2009.4.SPINE08159
Ahmed R, Menezes AH, Awe OO, Torner JC (2014) Long-term disease and neurological outcomes in patients with pediatric intramedullary spinal cord tumors: clinical article. J Neurosurg 13:600–612. https://doi.org/10.3171/2014.1.PEDS13316
Ahmed R, Menezes AH, Torner JC (2016) Role of resection and adjuvant therapy in long-term disease outcomes for low-grade pediatric intramedullary spinal cord tumors. J Neurosurg 18:594–601. https://doi.org/10.3171/2016.5.PEDS15356
McGirt MJ, Chaichana KL, Atiba A, Attenello F, Yao KC, Jallo GI (2008) Resection of intramedullary spinal cord tumors in children: assessment of long-term motor and sensory deficits. J Neurosurg 1:63–67. https://doi.org/10.3171/PED-08/01/063
Nakamura M, Ishii K, Watanabe K, Tsuji T, Takaishi H, Matsumoto M, Toyama Y, Chiba K (2008) Surgical treatment of intramedullary spinal cord tumors: prognosis and complications. Spinal Cord 46:282–286. https://doi.org/10.1038/sj.sc.3102130
Sala F, Palandri G, Basso E, Lanteri P, Deletis V, Faccioli F, Bricolo A (2006) Motor evoked potential monitoring improves outcome after surgery for intramedullary spinal cord tumors: a historical control study. Neurosurgery 58:1129–1143. https://doi.org/10.1227/01.NEU.0000215948.97195.58. (discussion 1129–1143)
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42:377–381. https://doi.org/10.1016/j.jbi.2008.08.010
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O'Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J, Duda SN, Consortium RE (2019) The REDCap consortium: building an international community of software platform partners. J Biomed Inform 95:103208. https://doi.org/10.1016/j.jbi.2019.103208
Nicholas MW, Corey R, Meghan M (2015) Spinal extradural neoplasms and intradural extramedullary neoplasms. In: Albright AL, Pollack PD, Adelson PD (eds) Principles and practice of pediatric neurosurgery, 3rd edn. Thieme Medical Publishers, New York, pp 594–604
Wang ZY, Sun JJ, Xie JC, Li ZD, Ma CC, Liu B, Chen XD, Liao HI, Yu T, Zhang J (2012) Comparative analysis on the diagnosis and treatments of multisegment intramedullary spinal cord tumors between the different age groups. Neurosurg Rev 35:85–92. https://doi.org/10.1007/s10143-011-0345-2
Bansal S, Suri A, Borkar SA, Kale SS, Singh M, Mahapatra AK (2012) Management of intramedullary tumors in children: Analysis of 82 operated cases. Child's Nerv Syst 28:2063–2069. https://doi.org/10.1007/s00381-012-1835-4
Hayden Gephart MG, Lober RM, Arrigo RT, Zygourakis CC, Guzman R, Boakye M, Edwards MSB, Fisher PG (2012) Trends in the diagnosis and treatment of pediatric primary spinal cord tumors: clinical article. J Neurosurg 10:555–559. https://doi.org/10.3171/2012.9.PEDS1272
Sciubba DM, Liang D, Kothbauer KF, Noggle JC, Jallo GI (2009) The evolution of intramedullary spinal cord tumor surgery. Neurosurgery 65:84–91. https://doi.org/10.1227/01.NEU.0000345628.39796.40. (discussion 91–82)
Epstein FJ, Farmer JP (1991) Trends in surgery: laser surgery, use of the cavitron, and debulking surgery. Neurol Clin 9:307–315
Regelsberger J, Fritzsche E, Langer N, Westphal M (2005) Intraoperative sonography of intra- and extramedullary tumors. Ultrasound Med Biol 31:593–598. https://doi.org/10.1016/j.ultrasmedbio.2005.01.016
Epstein FJ, Farmer JP, Schneider SJ (1991) Intraoperative ultrasonography: an important surgical adjunct for intramedullary tumors. J Neurosurg 74:729–733. https://doi.org/10.3171/jns.1991.74.5.0729
Gonzalez AA, Jeyanandarajan D, Hansen C, Zada G, Hsieh PC (2009) Intraoperative neurophysiological monitoring during spine surgery: a review. Neurosurg Focus 27:E6. https://doi.org/10.3171/2009.8.FOCUS09150
Daniel JW, Botelho RV, Milano JB, Dantas FR, Onishi FJ, Neto ER, Bertolini EF, Borgheresi MAD, Joaquim AF (2018) Intraoperative neurophysiological monitoring in spine surgery: a systematic review and meta-analysis. Spine (Phila Pa 1976) 43:1154–1160. https://doi.org/10.1097/BRS.0000000000002575
Kumar R, Singh V (2005) Benign intradural extramedullary masses in children of Northern India. Pediatr Neurosurg 41:22–28. https://doi.org/10.1159/000084861
Kumar R, Giri PJ (2008) Pediatric extradural spinal tumors. Pediatr Neurosurg 44:181–189. https://doi.org/10.1159/000120147
Bouffet E, Marec-Berard P, Thiesse P, Carrie C, Risk T, Jouvet A, Brunat-Mentigny M, Mottolese C (1997) Spinal cord compression by secondary epi- and intradural metastases in childhood. Child's Nerv Syst 13:383–387. https://doi.org/10.1007/s003810050105
Yang T, Wu L, Yang C, Deng X, Xu Y (2014) Clinical features and long-term outcomes of intraspinal ependymomas in pediatric patients. Child's Nerv Syst 30:2073–2081. https://doi.org/10.1007/s00381-014-2528-y
Benesch M, Weber-Mzell D, Gerber NU, Von Hoff K, Deinlein F, Krauss J, Warmuth-Metz M, Kortmann RD, Pietsch T, Driever PH, Quehenberger F, Urban C, Rutkowski S (2010) Ependymoma of the spinal cord in children and adolescents: a retrospective series from the HIT database: clinical article. J Neurosurg 6:137–144. https://doi.org/10.3171/2010.5.PEDS09553
Szathmari A, Zerah M, Vinchon M, Dufour C, Gimbert E, Di Rocco F, Chabaud S, Conter C, Mottolese C, Frappaz D (2019) Ependymoma of the spinal cord in children: a retrospective french study. World Neurosurg 126:e1035–e1041. https://doi.org/10.1016/j.wneu.2019.03.033
Abd-El-Barr MM, Huang KT, Chi JH (2016) Infiltrating spinal cord astrocytomas: epidemiology, diagnosis, treatments and future directions. J Clin Neurosci 29:15–20. https://doi.org/10.1016/j.jocn.2015.10.048
Scheinemann K, Bartels U, Huang A, Hawkins C, Kulkarni AV, Bouffet E, Tabori U (2009) Survival and functional outcome of childhood spinal cord low-grade gliomas. J Neurosurg 4:254–261. https://doi.org/10.3171/2009.4.PEDS08411
Townsend N, Handler M, Fleitz J, Foreman N (2004) Intramedullary spinal cord astrocytomas in children. Pediatr Blood Cancer 43:629–632. https://doi.org/10.1002/pbc.20082
Guss ZD, Moningi S, Jallo GI, Cohen KJ, Wharam MD, Terezakis SA (2013) Management of pediatric spinal cord astrocytomas: outcomes with adjuvant radiation. Int J Radiat Oncol Biol Phys 85:1307–1311. https://doi.org/10.1016/j.ijrobp.2012.11.022
Tsai CJ, Wang Y, Allen PK, Mahajan A, McCutcheon IE, Rao G, Rhines LD, Tatsui CE, Armstrong TS, Maor MH, Chang EL, Brown PD, Li J (2014) Outcomes after surgery and radiotherapy for spinal myxopapillary ependymoma: update of the MD anderson cancer center experience. Neurosurgery 75:205–214. https://doi.org/10.1227/NEU.0000000000000408
Teo WY, Chintagumpala M, Okcu MF, Dauser RC, Mahajan A, Adesina AM, Whitehead WE, Jea A, Bollo R, Paulino AC (2013) A retrospective analysis of the patterns of failure in pediatric myxopapillary ependymoma. J Radiat Oncol 2:21–26. https://doi.org/10.1007/s13566-012-0066-3
Keil VC, Schmitt AJ, Martin SC, Cadoux-Hudson TA, Pereira EA (2016) Optimising treatment strategies in spinal ependymoma based on 20 years of experience at a single centre. J Clin Neurosci 29:52–58. https://doi.org/10.1016/j.jocn.2016.01.003
Akyurek S, Chang EL, Yu TK, Little D, Allen PK, McCutcheon I, Mahajan A, Maor MH, Woo SY (2006) Spinal myxopapillary ependymoma outcomes in patients treated with surgery and radiotherapy at M.D. Anderson Cancer Center. J Neuro-Oncol 80:177–183. https://doi.org/10.1007/s11060-006-9169-2
Neumann JE, Spohn M, Obrecht D, Mynarek M, Thomas C, Hasselblatt M, Dorostkar MM, Wefers AK, Frank S, Monoranu CM, Koch A, Witt H, Kool M, Pajtler KW, Rutkowski S, Glatzel M, Schuller U (2019) Molecular characterization of histopathological ependymoma variants. Acta Neuropathol. https://doi.org/10.1007/s00401-019-02090-0
Witt H, Gramatzki D, Hentschel B, Pajtler KW, Felsberg J, Schackert G, Loffler M, Capper D, Sahm F, Sill M, von Deimling A, Kool M, Herrlinger U, Westphal M, Pietsch T, Reifenberger G, Pfister SM, Tonn JC, Weller M (2018) DNA methylation-based classification of ependymomas in adulthood: implications for diagnosis and treatment. Neuro Oncol 20:1616–1624. https://doi.org/10.1093/neuonc/noy118
Saito R, Kumabe T, Jokura H, Shirane R, Yoshimoto T (2003) Symptomatic spinal dissemination of malignant astrocytoma. J Neuro-Oncol 61:227–235. https://doi.org/10.1023/A:1022536828345
Jallo GI, Freed D, Epstein F (2003) Intramedullary spinal cord tumors in children. Child's Nerv Syst 19:641–649. https://doi.org/10.1007/s00381-003-0820-3
Ahmed R, Menezes AH, Awe OO, Mahaney KB, Torner JC, Weinstein SL (2014) Long-term incidence and risk factors for development of spinal deformity following resection of pediatric intramedullary spinal cord tumors: clinical article. J Neurosurg 13:613–621. https://doi.org/10.3171/2014.1.PEDS13317
Yao KC, McGirt MJ, Chaichana KL, Constantini S, Jallo GI (2007) Risk factors for progressive spinal deformity following resection of intramedullary spinal cord tumors in children: an analysis of 161 consecutive cases. J Neurosurg 107:463–468
McGirt MJ, Chaichana KL, Atiba A, Bydon A, Witham TF, Yao KC, Jallo GI (2008) Incidence of spinal deformity after resection of intramedullary spinal cord tumors in children who underwent laminectomy compared with laminoplasty. J Neurosurg 1:57–62. https://doi.org/10.3171/PED-08/01/057
McGirt MJ, Garcés-Ambrossi GL, Parker SL, Sciubba DM, Bydon A, Wolinksy JP, Gokaslan ZL, Jallo G, Witham TF (2010) Short-term progressive spinal deformity following laminoplasty versus laminectomy for resection of intradural spinal tumors: analysis of 238 patients. Neurosurgery 66:1005–1012. https://doi.org/10.1227/01.NEU.0000367721.73220.C9
Hsu W, Pradilla G, Constantini S, Jallo GI (2009) Surgical considerations of spinal ependymomas in the pediatric population. Child's Nerv Syst 25:1253–1259. https://doi.org/10.1007/s00381-009-0882-y
Acknowledgements
The authors acknowledge statistical assistance provided by the Center of Statistical Consultation and Research in the Department of Medical Research, National Taiwan University Hospital, Taipei, Taiwan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in the study involving human participants were in accordance with the ethical standards of the research ethics committee of the National Taiwan University Hospital, Taipei, Taiwan.
Informed consent
A waiver of consent was obtained from the research ethics committee for this retrospective, minimal-risk study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chou, SC., Kuo, MF., Lai, DM. et al. Contemporary management of pediatric spinal tumors: a single institute's experience in Taiwan in the modern era. J Neurooncol 146, 501–511 (2020). https://doi.org/10.1007/s11060-020-03400-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-020-03400-3