Abstract
Background
We aimed to evaluate the various clinicopathodemographical, epidemiological, and molecular contributors to cumulatively worldwide metastatic colorectal cancer (CRC) in CRC patients from a highly populated area in northeastern Iran to pinpoint metastasis risk.
Methods
A retrospective clinical material-based cohort including a total of 6260 registered CRC patients, of whom 3829 underwent surgery, from regional university hospitals, during 2006–2016, were analyzed for the clinicopathodemographical aspects of age, sex, stage of CRC, history of smoking, type 2 diabetes (T2D), hypertension, body mass index (BMI), familial/occupational status, post-surgery survival period and mRNA/protein expression of mucin stabilizer (B3GALNT2), mucin I (MUC1), key cell cycle molecules (i.e., P53 and Ki67), and MMR-related genes. Factors were set to estimate the risk of metastatic CRC and mortality.
Results
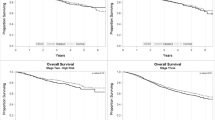
Predominant adenocarcinomatous CRCs were found in colon. Post-surgery survival period of metastatic CRC patients was remarkably longer in patients aged > 50 compared to those aged < 50 years, and worse in females than males. B3GALNT2high, MUChigh, P53low, and Ki67high mRNA/protein expression in the metastatic stage III CRC along with T2D and hypertension were associated with increased metastasis/mortality, with more worsening in males, older, BMI > 25, urban residing, and employed individuals, indicative of non-genetic attributable factors.
Conclusion
B3GALNT2, MUC1, and “Ki67” can be used as promising biomarkers for prognosis and early diagnosis of increasingly/predominantly non-genetic/environmental originated metastatic CRCs.



Similar content being viewed by others
Data availability
All data are available in this article and supporting file.
References
Azimi M, Mehrzad J, Ahmadi A, Ahmadi E, Ghorbani Ranjbary A (2021) Apoptosis Induced by Ziziphora tenuior essential oil in human colorectal cancer cells. Biomed Res Int 2021:5522964. https://doi.org/10.1155/2021/5522964
Fleming M, Ravula S, Tatishchev SF, Wang HL (2012) Colorectal carcinoma: pathologic aspects. J Gastrointest Oncol 3:153–173. https://doi.org/10.3978/j.issn.2078-6891.2012.030
Rawla P, Sunkara T, Barsouk A (2019) Epidemiology of colorectal cancer: incidence, mortality, survival, and risk factors. Prz Gastroenterol 14(2):89–103. https://doi.org/10.5114/pg.2018.81072
Liu Q, Ran D, Wang L, Feng J, Deng W, Mei D, Peng Y, Du C (2023) Association between Ki67 expression and therapeutic outcome in colon cancer. Oncol Lett 25(6):1–6. https://doi.org/10.3892/ol.2023.13858
Balestra A, Larsimont D, Noël JC (2023) HER2 amplification in p53-mutated endometrial carcinomas. Cancers 15(5):1435. https://doi.org/10.3390/cancers15051435
Cox KE, Liu S, Lwin TM, Hoffman RM, Batra SK, Bouvet M (2023) The mucin family of proteins: candidates as potential biomarkers for colon cancer. Cancers 15(5):1491. https://doi.org/10.3390/cancers15051491
Matsuo T, Komatsu M, Yoshimaru T, Kiyotani K, Miyoshi Y, Sasa M, Katagiri T (2014) Involvement of B3GALNT2 overexpression in the cell growth of breast cancer. Int J Oncol 44:427–434. https://doi.org/10.3892/ijo.2013.2187
Raina D, Agarwal P, Lee J et al (2015) Characterization of the MUC1-C cytoplasmic domain as a cancer target. PLoS ONE 10:0135156. https://doi.org/10.1371/journal.pone.0135156
Hiruma T, Togayachi A, Okamura K et al (2004) A novel human β1, 3-N-acetylgalactosaminyltransferase that synthesizes a unique carbohydrate structure, GalNAcβ1-3GlcNAc. J Biol Chem 279:14087–14095. https://doi.org/10.1074/jbc.M310614200
Denk S, Schmidt S, Schurr Y, Schwarz G, Schote F, Diefenbacher M, Armendariz C, Dejure F, Eilers M, Wiegering A (2021) CIP2A regulates MYC translation (via its 5′ UTR) in colorectal cancer. Int J Colorectal Dis 36(5):911–918. https://doi.org/10.1007/s00384-021-03960-4
Siegel RL, Miller KD, Jemal A (2016) Cancer statistics. CA Cancer J Clin 66:7–30. https://doi.org/10.3322/caac.21332
Yatabe S, Eto K, Haruki K, Shiba H, Kosuge M, Ohkuma M, Ito D, Takeda Y, Sugano H, Sasaki S, Yanaga K (2020) Signification of systemic immune-inflammation index for prediction of prognosis after resecting in patients with colorectal cancer. Int J Colorectal Dis 35:1549–1555. https://doi.org/10.1007/s00384-020-03615-w
Ghorbani Ranjbary A, Mehrzad J, Dehghani H, Abdollahi A, Hosseinkhani S (2020) Variation in blood and colorectal Epithelia’s key trace elements along with expression of mismatch repair proteins from localized and metastatic colorectal cancer. Biol Trace Elem Res 194:66–75. https://doi.org/10.1007/s12011-019-01749-9
Dolatkhah R, Somi MH, Bonyadi MJ, Asvadi-Kermani I, Farassati F, Dastgiri S (2015) Colorectal cancer in Iran: molecular epidemiology and screening strategies. J Cancer Epidemiol. https://doi.org/10.1155/2015/643020
Geijsen AJ, Brezina S, Keski-Rahkonen P et al (2019) Plasma metabolites associated with colorectal cancer: a discovery‐replication strategy. Int J Cancer 145:1221–1231. https://doi.org/10.1002/ijc.32146
Sud S, O’Callaghan C, Jonker C et al (2018) Hypertension as a predictor of advanced colorectal cancer outcome and cetuximab treatment response. Curr Oncol 25:516. https://doi.org/10.3747/co.25.4069
Tanjani PT, Motlagh ME, Nazar MM, Najafi F (2015)The health status of the elderly population of Iran in 2012. Arch Gerontol Geriatr Suppl 60:281–287. https://doi.org/10.1016/j.archger.2015.01.004
Danial Z, Motamedi M, Mirhashemi S, Kazemi A, Mirhashemi AH (2014) Aging in Iran. Lancet 384(9958):1927. https://doi.org/10.1016/S0140-6736(14)62278-9
Rafiemanesh H, Pakzad R, Abedi M, Kor Y, Moludi J, Towhidi F, Makhsosi BR, Salehiniya H (2016) Colorectal cancer in Iran: epidemiology and morphology trends. EXCLI J 15:738. https://doi.org/10.17179/excli2016-346
Ranjbary AG, Saleh GK, Azimi M, Karimian F, Mehrzad J, Zohdi J (2023) Superparamagnetic iron oxide nanoparticles induce apoptosis in HT-29 cells by stimulating oxidative stress and damaging DNA. Biol Trace Elem Res 201(3):1163–1173. https://doi.org/10.1007/s12011-022-03229-z
Unver A, Felek S, Paddock CD et al (2001) Western blot analysis of sera reactive to human monocytic ehrlichiosis and human granulocytic ehrlichiosis agents. J Clin Microbiolo 39:3982–3986. https://doi.org/10.1128/JCM.39.11.3982-3986.2001
Lee KS, Kwak Y, Ahn S et al (2017) Prognostic implication of CD274 (PD-L1) protein expression in tumor-infiltrating immune cells for microsatellite unstable and stable colorectal cancer. Cancer Immunol Immunother 66:927–939. https://doi.org/10.1007/s00262-017-1999-6
Clendenning M, Huang A, Jayasekara H et al (2018) Somatic mutations of the coding microsatellites within the beta-2-microglobulin gene in mismatch repair-deficient colorectal cancers and adenomas. Fam Cancer 17:91–100. https://doi.org/10.1007/s10689-017-0013-y
Ghoncheh M, Mohammadian M, Mohammadian-Hafshejani A, Salehiniya H (2016) The incidence and mortality of colorectal cancer and its relationship with the human development index in Asia. Ann Glob Health. 82, 726 – 37 https://doi.org/10.1016/j.aogh.2016.10.004
Chen J, Lin Y, Zhang R, Huang ZJ, Pan XG (2012) Contribution of NAD(P)H quinone oxidoreductase 1 (NQO1) Pro187Ser polymorphism and risk of colorectal adenoma and colorectal cancer in Caucasians: a meta-analysis. Arch Med Res 43:55–66. https://doi.org/10.1016/j.arcmed.2012.01.005
Sobhani I, Amiot A, Le-Baleur Y, Levy M, Auriault ML, Van-Nhieu JT, Delchier JC (2015) Microbial dysbiosis and colon carcinogenesis: could colon cancer be considered a bacteria-related disease? Th Adv Gastroenterol 6:215–229. https://doi.org/10.1177/1756283X12473674
Jiang Y, Ben Q, Shen H, Lu W, Zhang Y, Zhu J (2011) Diabetes mellitus and incidence and mortality of colorectal cancer: a systematic review and meta-analysis of cohort studies. Eur J Epidemiol 26:863–876. https://doi.org/10.1007/s10654-011-9617-y
Peeters PJ, Bazelier MT, Leufkens HG, Vries F, De-Bruin ML (2015) The risk of colorectal cancer in patients with type 2 diabetes: associations with treatment stage and obesity. Diabetes Care 38:495–502. https://doi.org/10.2337/dc14-1175
Zhu B, Wu X, Wu B, Pei D, Zhang L, Wei L (2017) The relationship between diabetes and colorectal cancer prognosis: a meta-analysis based on the cohort studies. PLoS ONE 19:1e0176068. https://doi.org/10.1371/journal.pone.0176068
Navabi SJ, Beiranvand B, Pournia Y et al (2012) Epidemiology of colorectal cancer in patients admitted to Imam Reza hospital in Kermanshah from 2006 to 2011. Basic Clin Cancer Res 27:2–7. https://doi.org/10.7314/APJCP.2015.16.1.133
Papadopoulos VN, Michalopoulos A, Netta S, Basdanis G, Paramythiotis D, Zatagias A, Berovalis P, Harlaftis N (2004) Prognostic significance of mucinous component in colorectal carcinoma. Tech Coloproctol 8(1):s123–s125. https://doi.org/10.1007/s10151-004-0131-z
Mansori K, Solaymani-Dodaran M, Mosavi-Jarrahi A, Motlagh AG, Salehi M, Delavari A, Asadi-Lari M (2014) Spatial inequalities in the incidence of colorectal cancer and associated factors in the neighborhoods of Tehran, Iran: bayesian spatial models. J Prev Med Public Health 51:33–36. https://doi.org/10.3961/jpmph.17.167
Shadmani FK, Ayubi E, Khazaei S et al (2017) Geographic distribution of the incidence of colorectal cancer in Iran: a population-based study. Epidemiol Health 17:1–13. https://doi.org/10.4178/epih.e2017020
Haggar FA, Boushey RP (2009) Colorectal cancer epidemiology: incidence, mortality, survival, and risk factors. Clin Colon Rectal Surg 22:191–197. https://doi.org/10.1055/s-0029-1242458
Hoseini S, Moaddabshoar L, Hemati S, Mohammadianpanah M (2014) An overview of clinical and pathological characteristics and survival rate of colorectal cancer in Iran. Ann Colorectal Res 2:e17264. https://doi.org/10.17795/acr-17264
Yoosefi M, Baghestani AR, Khadembashi N, Pourhoseingholi MA, Baghban AA, Khosrovirad A (2018) Survival analysis of Colorectal Cancer Patients using Exponentiated Weibull distribution. Int J Cancer Management 11:1–6. https://doi.org/10.5812/ijcm.8686
Bracci PM (2012) Obesity and pancreatic cancer: overview of epidemiologic evidence and biologic mechanisms. Mol Carcinog 51:53–63. https://doi.org/10.1002/mc.20778
Wang L, Liu Z, Fisher KW et al (2018) Prognostic value of programmed death ligand 1, p53, and Ki-67 in patients with advanced-stage colorectal cancer. Hum Pathol 71:20–29. https://doi.org/10.1016/j.humpath.2017.07.014
Limsui D, Vierkant RA, Tillmans LS et al (2010) Cigarette smoking and colorectal cancer risk by molecularly defined subtypes. J Natl Cancer Inst. https://doi.org/10.1093/jnci/djq201. 102,1012-22
Peppone LJ, Hyland A, Moysich KB et al (2009) Examining the association between cigarette smoking and colorectal cancer using historical case-control data. Cancer Epidemiol 33:182–188. https://doi.org/10.1016/j.canep.2009.07.004
Byrd JC, Bresalier RS (2004) Mucins and mucin binding proteins in colorectal cancer. Cancer Metast Rev. 23, 77 – 9 https://doi.org/10.1023/a:1025815113599
Bu XD, Li N, Tian X-Q, Li L, Wang JS, Yu XJ, Huang PL (2010) Altered expression of MUC2 and MUC5AC in progression of colorectal carcinoma. World J Gastroenterol 16:4089–4094. https://doi.org/10.3748/wjg.v16.i32.4089
Jing X, Liang H, Hao C, Yang X, Cui X (2019) Overexpression of MUC1 predicts poor prognosis in patients with breast cancer. Oncol Rep 41:801–810. https://doi.org/10.3892/or.2018.6887
Khanh DT, Mekata E, Mukaisho KI et al (2013) Transmembrane mucin MUC1 overexpression and its association with CD10 + myeloid cells, transforming growth factor-β1 expression, and tumor budding grade in colorectal cancer. Cancer Sci 104:958–964. https://doi.org/10.1111/cas.12170
Almaraz RT, Tian Y, Bhattarcharya R et al (2012) Metabolic flux increases glycoprotein sialylation: implications for cell adhesion and cancer metastasis. Mol Cell Proteomics 11:112017558. https://doi.org/10.1074/mcp.M112.017558
Ju T, Aryal RP, Kudelka MR, Wang Y, Cummings RD (2014) The Cosmc connection to the tn antigen in cancer. Cancer Biomark 14:63–81. https://doi.org/10.3233/CBM-130375
Peixoto A, Relvas-Santos M, Azevedo R, Santos LL, Ferreira JA (2019) Protein glycosylation and tumour microenvironment alterations driving cancer hallmarks. Front Oncol 9:380. https://doi.org/10.3389/fonc.2019.00380
Ogawa T, Hirohashi Y, Murai A et al (2017) ST6GALNAC1 plays important roles in enhancing cancer stem phenotypes of colorectal cancer via the akt pathway. Oncotarget 8:112550. https://doi.org/10.18632/oncotarget.22545
Nath S, Mukherjee P (2014) MUC1: a multifaceted oncoprotein with a key role in cancer progression. Trends Mol Med. 20, 332 – 42 https://doi.org/10.1016/j.molmed.2014.02.007
Hu M, Lan Y, Lu A, Ma X, Zhang L (2019) Glycan-based biomarkers for diagnosis of cancers and other diseases: past, present, and future. Prog Mol Biol Transl Sci 162:1–24. https://doi.org/10.1016/bs.pmbts.2018.12.002
Park JH, Katagiri T, Chung S, Kijima K, Nakamura Y (2014) Polypeptide N-acetylgalactosaminyltransferase 6 disrupts mammary acinar morphogenesis through O-glycosylation of fibronectin. Neoplasia 13:320. https://doi.org/10.1593/neo.101440
Johnson K, Bertoli M, Phillips L et al (2018) Detection of variants in dystroglycanopathy-associated genes through the application of targeted whole-exome sequencing analysis to a large cohort of patients with unexplained limb-girdle muscle weakness. Skelet Muscle 8:23. https://doi.org/10.1186/s13395-018-0170-1
Sysel AM, Valli VE, Bauer JA (2015) Immunohistochemical quantification of the cobalamin transport protein, cell surface receptor and Ki-67 in naturally occurring canine and feline malignant tumors and in adjacent normal tissues. Oncotarget 6:2331. https://doi.org/10.18632/oncotarget.3206
Ghorbani Ranjbary A, Mehrzad J, Abdollahi A, Hosseinkhani S, Tabatabaee A, Dehghani H (2019) Clinicodemographical assessment of colorectal cancer with emphasis on B3GALNT2, MUC1, P53 and Ki67-related risk of metastasis. Research Square; view at: https://www.researchsquare.com/article/rs-5427/v2
Acknowledgements
The authors appreciate the supports from Ferdowsi University of Mashhad and University of Tehran. We are grateful to Dr. Per Hydbring for critically reading and editing the manuscript. Part of this manuscript was submitted and then rejected in BMC Cancer, but mistakenly appeared/viewed at the Research Square as a pre-print54, which should have been removed from the Research Square; simultaneously, after rejection we further worked, did more assays, and improved the quality of manuscript for publication.
Funding
This study was (along with specific funding from the main investigator) partially supported from the Ferdowsi University of Mashhad and University of Tehran.
Author information
Authors and Affiliations
Contributions
AGR and JM collected the data, performed the treatments, and designed, wrote, and finalized the study. JM was also responsible for paper and for its supervision. NR and HD reviewed statistical analyses, supported the data collection, and critically revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
The study protocol has been approved by the ethical committee of Mashhad University of Medical Sciences with the commitment of the principles of the declaration of Helsinki.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ghorbani Ranjbary, A., Mehrzad, J., Rahbar, N. et al. Impacts of some clinicopathodemography and colorectal tissues key cell cycle and mucin stabilizing molecules on the metastasis trend in colorectal cancer patients. Mol Biol Rep 50, 8589–8601 (2023). https://doi.org/10.1007/s11033-023-08766-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-023-08766-x