Abstract
Background
Regulatory T cells (Tregs) have an important role in the control of the immune responses. This study aimed to compare the frequency of peripheral blood (PB) CD4+ CD25+ FoxP3+ Treg cells and PB and duodenal expression levels of pro- and anti-inflammatory mediators in treated celiac disease (CD) patients and healthy controls.
Methods and results
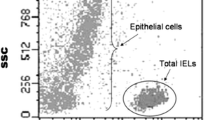
Duodenal biopsy specimens and PB samples were collected from 60 treated CD patients and 60 controls. Flow cytometry analysis was conducted on peripheral blood mononuclear cell (PBMC) specimens and relative PB and duodenal mRNA expression levels of CD25, forkhead box P3 (Foxp3), interleukin (IL)-10 and granzyme B (GrzB) were evaluated using quantitative real-time PCR. The levels of serum IL-10 and IL-6 were tested with sandwich enzyme-linked immunosorbent assay kits. p values < 0.05 were considered significant. Flow cytometry analysis showed a significant decrease in the number of Tregs in CD patients’ PBMC specimens (p = 0.012). CD25 and Foxp3 PB mRNA expressions were also lower in CD patients without reaching the significance level (p > 0.05). IL-10 PB mRNA and protein expression did not differ between the groups (p > 0.05), and GrzB PB expression was significantly reduced in CD patients (p = 0.001). In duodenal specimens of CD patients, while significantly increased CD25, Foxp3 mRNA expression (p = 0.01 and 0.001, respectively) and decreased IL-10 mRNA expression (p = 0.02) were observed, GrzB mRNA expression did not differ between groups (p > 0.05). Moreover, a high serum level of IL-6 was observed in CD patients (p = 0.001).
Conclusions
Despite following the gluten free diet, there may still be residual inflammation in the intestine of CD patients. Accordingly, finding a therapeutic approach based on strengthening the function of Treg cells in CD might be helpful.



Similar content being viewed by others
References
Vriezinga SL, Schweizer JJ, Koning F, Mearin ML (2015) Coeliac disease and gluten-related disorders in childhood. Nat Rev Gastroenterol Hepatol 12:527–536. https://doi.org/10.1038/nrgastro.2015.98
Bascuñán KA, Vespa MC, Araya M (2017) Celiac disease: understanding the gluten-free diet. Eur J Nutr 56:449–459. https://doi.org/10.1007/s00394-016-1238-5
Lebwohl B, Sanders DS, Green PHR (2018) Coeliac disease. Lancet 391:70–81. https://doi.org/10.1016/s0140-6736(17)31796-8
Rostami-Nejad M, Razzaghi Z, Esmaeili S, Rezaei-Tavirani S, Akbarzadeh Baghban A, Vafaee R (2020) Immunological reactions by T cell and regulation of crucial genes in treated celiac disease patients. Gastroenterol Hepatol Bed Bench 13:155–160
Bardella MT, Elli L, Velio P, Fredella C, Prampolini L, Cesana B (2007) Silent celiac disease is frequent in the siblings of newly diagnosed celiac patients. Digestion 75:182–187. https://doi.org/10.1159/000107979
Admou B, Essaadouni L, Krati K et al (2012) Atypical celiac disease: from recognizing to managing. Gastroenterol Res Pract 2012:637187–637187. https://doi.org/10.1155/2012/637187
Gujral N, Freeman HJ, Thomson ABR (2012) Celiac disease: prevalence, diagnosis, pathogenesis and treatment. World J Gastroenterol 18:6036–6059. https://doi.org/10.3748/wjg.v18.i42.6036
Caio G, Volta U, Sapone A et al (2019) Celiac disease: a comprehensive current review. BMC Med 17:142–142. https://doi.org/10.1186/s12916-019-1380-z
Meresse B, Ripoche J, Heyman M, Cerf-Bensussan N (2009) Celiac disease: from oral tolerance to intestinal inflammation, autoimmunity and lymphomagenesis. Mucosal Immunol 2:8–23. https://doi.org/10.1038/mi.2008.75
Asri N, Nazemalhosseini Mojarad E, Mirjalali H et al (2021) Toward finding the difference between untreated celiac disease and COVID-19 infected patients in terms of CD4, CD25 (IL-2 Rα), FOXP3 and IL-6 expressions as genes affecting immune homeostasis. BMC Gastroenterol 21:462–462. https://doi.org/10.1186/s12876-021-02056-1
Gianfrani C, Levings MK, Sartirana C et al (2006) Gliadin-specific type 1 regulatory T cells from the intestinal mucosa of treated celiac patients inhibit pathogenic T cells. J Immunol 177:4178–4186. https://doi.org/10.4049/jimmunol.177.6.4178
Torres MI, López Casado MA, Ríos A (2007) New aspects in celiac disease. World J Gastroenterol 13:1156–1161. https://doi.org/10.3748/wjg.v13.i8.1156
Pabst O, Mowat AM (2012) Oral tolerance to food protein. Mucosal Immunol 5:232–239. https://doi.org/10.1038/mi.2012.4
Schuster M, Plaza-Sirvent C, Visekruna A, Huehn J, Schmitz I (2019) Generation of Foxp3+CD25—regulatory T-cell precursors requires c-Rel and IκBNS. Front Immunol 10:1583. https://doi.org/10.3389/fimmu.2019.01583
Faria AMC, Weiner HL (2006) Oral tolerance: therapeutic implications for autoimmune diseases. Clin Dev Immunol 13:828392. https://doi.org/10.1080/17402520600876804
Coleman MM, Finlay CM, Moran B, Keane J, Dunne PJ, Mills KH (2012) The immunoregulatory role of CD4+ FoxP3+ CD25− regulatory T cells in lungs of mice infected with Bordetella pertussis. Immunol Med Microbiol 64:413–424. https://doi.org/10.1111/j.1574-695X.2011.00927.x
Hmida NB, Ben Ahmed M, Moussa A et al (2012) Impaired control of effector T cells by regulatory T cells: a clue to loss of oral tolerance and autoimmunity in celiac disease? Am J Gastroenterol 107:604–611. https://doi.org/10.1038/ajg.2011.397
Granzotto M, dal Bo S, Quaglia S et al (2009) Regulatory T-cell function is impaired in celiac disease. Dig Dis Sci 54:1513–1519. https://doi.org/10.1007/s10620-008-0501-x
Cook L, Munier CML, Seddiki N et al (2020) Circulating gluten-specific, but not CMV-specific, CD39(+) regulatory T cells have an oligoclonal TCR repertoire. Clin Transl Immunol 9:e1096–e1096. https://doi.org/10.1002/cti2.1096
Workman CJ, Szymczak-Workman AL, Collison LW, Pillai MR, Vignali DAA (2009) The development and function of regulatory T cells. Cell Mol Life Sci 66:2603–2622. https://doi.org/10.1007/s00018-009-0026-2
Li Z, Li D, Tsun A, Li B (2015) FOXP3+ regulatory T cells and their functional regulation. Cell Mol Immunol 12:558–565. https://doi.org/10.1038/cmi.2015.10
Zhao H, Liao X, Kang Y (2017) Tregs: where we are and what comes next? Front Immunol 8:1578. https://doi.org/10.3389/fimmu.2017.01578
Wang J, Ioan-Facsinay A, van der Voort EI, Huizinga TW, Toes RE (2007) Transient expression of FOXP3 in human activated nonregulatory CD4+ T cells. Eur J Immunol 37:129–138. https://doi.org/10.1002/eji.200636435
Lee W, Lee GR (2018) Transcriptional regulation and development of regulatory T cells. Exp Mol Med 50:e456–e456. https://doi.org/10.1038/emm.2017.313
Asri N, Rostami-Nejad M, Barzegar M et al (2020) Suppressive mechanisms induced by tregs in celiac disease. Iran Biomed J 24(3):140–147
Schmidt A, Oberle N, Krammer P (2012) Molecular mechanisms of treg-mediated T cell suppression. Front Immunol 3:51. https://doi.org/10.3389/fimmu.2012.00051
Jordan MA, Field J, Butzkueven H, Baxter AG (2014) Genetic predisposition, humans. In: Rose NR, Mackay IR (eds) The autoimmune diseases, 5th edn. Academic Press, Boston, pp 341–364
Kasper IR, Apostolidis SA, Sharabi A, Tsokos GC (2016) Empowering regulatory T cells in autoimmunity. Trends Mol Med 22:784–797. https://doi.org/10.1016/j.molmed.2016.07.003
Chinen T, Kannan AK, Levine AG et al (2016) An essential role for the IL-2 receptor in Treg cell function. Nat Immunol 17:1322–1333. https://doi.org/10.1038/ni.3540
Verbsky JW, Routes JR (2018) Recurrent fever, infections, immune disorders, and autoinflammatory diseases. In: Kliegman RM, Lye PS, Bordini BJ, Toth H, Basel D (eds) Nelson pediatric symptom-based diagnosis. Elsevier, Amsterdam, pp 746–773
Vella A, Cooper JD, Lowe CE et al (2005) Localization of a type 1 diabetes locus in the IL2RA/CD25 region by use of tag single-nucleotide polymorphisms. Am J Hum Genet 76:773–779. https://doi.org/10.1086/429843
Vignali DAA, Collison LW, Workman CJ (2008) How regulatory T cells work. Nat Rev Immunol 8:523–532. https://doi.org/10.1038/nri2343
Shevyrev D, Tereshchenko V (2020) Treg heterogeneity, function, and homeostasis. Front Immunol. https://doi.org/10.3389/fimmu.2019.03100
Penny HA, Baggus EMR, Rej A, Snowden JA, Sanders DS (2020) Non-Responsive coeliac disease: a comprehensive review from the NHS England national centre for refractory coeliac disease. Nutrients 12:216. https://doi.org/10.3390/nu12010216
Cook L, Munier CML, Seddiki N et al (2017) Circulating gluten-specific FOXP3(+)CD39(+) regulatory T cells have impaired suppressive function in patients with celiac disease. J Allergy Clin Immunol 140:1592-1603.e1598. https://doi.org/10.1016/j.jaci.2017.02.015
Tiittanen M, Westerholm-Ormio M, Verkasalo M, Savilahti E, Vaarala O (2008) Infiltration of forkhead box P3-expressing cells in small intestinal mucosa in coeliac disease but not in type 1 diabetes. Clin Exp Immunol 152:498–507. https://doi.org/10.1111/j.1365-2249.2008.03662.x
Mazzarella G (2015) Effector and suppressor T cells in celiac disease. World J Gastroenterol 21:7349–7356. https://doi.org/10.3748/wjg.v21.i24.7349
Bardella MT, Elli L, Ferretti F (2016) Non celiac gluten sensitivity. Curr Gastroenterol Rep 18:63. https://doi.org/10.1007/s11894-016-0536-7
Anderson RP (2022) Emergence of an adaptive immune paradigm to explain celiac disease: a perspective on new evidence and implications for future interventions and diagnosis. Expert Rev Clin Immunol 18:75–91. https://doi.org/10.1080/1744666x.2021.2006636
Frisullo G, Nociti V, Iorio R et al (2009) Increased CD4+CD25+Foxp3+ T cells in peripheral blood of celiac disease patients: correlation with dietary treatment. Hum Immunol 70:430–435. https://doi.org/10.1016/j.humimm.2009.04.006
Kumar S, Lal S, Bhatnagar A (2017) Regulatory T cell subsets in peripheral blood of celiac disease patients and TLR2 expression: correlation with oxidative stress. APMIS 125:888–901. https://doi.org/10.1111/apm.12735
Brazowski E, Cohen S, Yaron A, Filip I, Eisenthal A (2010) FOXP3 expression in duodenal mucosa in pediatric patients with celiac disease. Pathobiology 77:328–334. https://doi.org/10.1159/000322049
Vorobjova T, Uibo O, Heilman K et al (2009) Increased FOXP3 expression in small-bowel mucosa of children with coeliac disease and type I diabetes mellitus. Scand J Gastroenterol 44:422–430. https://doi.org/10.1080/00365520802624177
Christophersen A, Risnes LF, Bergseng E, Lundin KE, Sollid LM, Qiao SW (2016) Healthy HLA-DQ2.5+ subjects lack regulatory and memory T cells specific for immunodominant gluten epitopes of celiac disease. J Immunol 196:2819–2826. https://doi.org/10.4049/jimmunol.1501152
Acknowledgements
The authors would like to acknowledge the Gastroenterology and Liver Diseases Research Center of Shahid Beheshti University of Medical Sciences for their support and contribution to this study. The authors would also like to thanks Dr Robert P Anderson from Wesley Medical Research—The Wesley Hospital, Brisbane, Queensland, Australia for his critical review.
Funding
Research reported in this publication was supported by Elite Researcher Grant Committee under Award Number (983076) from the National Institute for Medical Research Development (NIMAD), Tehran, Iran and Gastroenterology and Liver Diseases Research Center of Shahid Beheshti University of Medical Sciences.
Author information
Authors and Affiliations
Contributions
Design of experiments by MRN and AN. Analysis of data by NA and EA. First draft of manuscript by NA, and subsequent drafting by MRN, MRZ and HAA. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interest to disclose.
Ethical approval
The study was approved by the ethical committee of the Research Institute for Gastroenterology and Liver Diseases (RIGLD), Shahid Beheshti University of Medical Sciences, Tehran, Iran (IR.SBMU.MSP.REC.1397.564).
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Asri, N., Rostami-Nejad, M., Nikzamir, A. et al. Reduced frequency of circulating regulatory T cells and their related immunosuppressive mediators in treated celiac patients. Mol Biol Rep 49, 8527–8535 (2022). https://doi.org/10.1007/s11033-022-07674-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-022-07674-w