Abstract
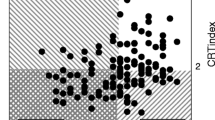
Minimal hepatic encephalopathy (MHE) is intermittently present in up to 2/3 of patients with chronic liver disease. It impairs their daily living and can be treated. However, there is no consensus on diagnostic criteria except that psychometric methods are required. We compared two easy-to-perform reproducible bedside methods: the critical flicker frequency (CFF) and continuous reaction times (CRT) tests. A CFF <39 Hz and CRT-index <1.9 (index: the ratio 50/(90 minus 10) percentiles of reaction times) indicates cerebral dysfunction. 154 patients with acute or chronic liver disease with out overt hepatic encephalopathy (HE) underwent both tests at the same occasion. Both tests were abnormal in 20% of the patients and both tests were normal in 40% of the patients. In more than 1/3 the two tests were not in agreement as CFF classified 32% and CRT-index classified 48% of the patients as having MHE (p < 0.005). The two tests were weakly linearly correlated (r2 = 0.14, p < 0.001) and neither test correlated with the metabolic liver function measured by the Galactose Elimination Capacity (GEC), nor with the blood ammonia concentration. Both tests identified a large fraction of the patients as having MHE and cleared only 40%. The two tests did not show concordant results, likely because they describe different aspects of MHE: the CFF gives a measure of astrocytic metabolic state and hence pathogenic aspects of MHE, whereas the CRT measures a composite key performance, viz. the ability of reacting appropriately to a sensory stimulus. The choice of test depends on the information needed in the clinical and scientific care and study of the patients.


Similar content being viewed by others
References
Amodio P, Quero JC, Del Piccolo F, Gatta A, Schalm SW (1996) Diagnostic tools for the detection of subclinical hepatic encephalopathy: comparison of standard and computerized psychometric tests with spectral-eeg. Metab Brain Dis 11:315–327
Amodio P, Montagnese S, Gatta A, Morgan MY (2004) Characteristics of minimal hepatic encephalopathy. Metab Brain Dis 19:253–267
Bajaj JS (2008) Minimal hepatic encephalopathy matters in daily life. World J Gastroenterol 14:3609–3615
Bao ZJ, Qiu DK, Ma X et al (2007) Assessment of health-related quality of life in chinese patients with minimal hepatic encephalopathy. World J Gastroenterol 13:3003–3008
Dhiman RK, Saraswat VA, Sharma BK et al (2010) Minimal hepatic encephalopathy: consensus statement of a working party of the indian national association for study of the liver. J Gastroenterol Hepatol 25:1029–1041. doi:10.1111/j.1440-1746.2010.06318.x
Elsass P, Christensen SE, Ranek L, Theilgaard A, Tygstrup N (1981) Continuous reaction time in patients with hepatic encephalopathy. A quantitative measure of changes in consciousness. Scand J Gastroenterol 16:441–447
Ferenci P, Lockwood A, Mullen K, Tarter R, Weissenborn K, Blei AT (2002) Hepatic encephalopathy—definition, nomenclature, diagnosis, and quantification: final report of the working party at the 11th world congresses of gastroenterology, vienna, 1998. Hepatology 35:716–721. doi:10.1053/jhep.2002.31250
Groeneweg M, Quero JC, De Bruijn I et al (1998) Subclinical hepatic encephalopathy impairs daily functioning. Hepatology 28:45–49. doi:10.1002/hep.510280108
Groeneweg M, Moerland W, Quero JC, Hop WC, Krabbe PF, Schalm SW (2000) Screening of subclinical hepatic encephalopathy. J Hepatol 32:748–753
Haussinger D, Schliess F, Kircheis G (2002) Pathogenesis of hepatic encephalopathy. J Gastroenterol Hepatol 17(Suppl 3):S256–S259
Jakobsen LH, Sorensen JM, Rask IK, Jensen BS, Kondrup J (2010) Validation of reaction time as a measure of cognitive function and quality of life in healthy subjects and patients. Nutrition.doi:10.1016/j.nut.2010.08.003
Jepsen POP, Andersen PK, Sørensen HT, Vilstrup H (2010) The clinical course of alcoholic cirrhosis with ascites: effects of liver and kidney function, hyponatremia, and alcohol. Hepatology 52:896A
Kircheis G, Wettstein M, Timmermann L, Schnitzler A, Haussinger D (2002) Critical flicker frequency for quantification of low-grade hepatic encephalopathy. Hepatology 35:357–366. doi:10.1053/jhep.2002.30957
Kircheis G, Bode JG, Hilger N, Kramer T, Schnitzler A, Haussinger D (2009a) Diagnostic and prognostic values of critical flicker frequency determination as new diagnostic tool for objective he evaluation in patients undergoing tips implantation. Eur J Gastroenterol Hepatol 21:1383–1394. doi:10.1097/MEG.0b013e328310e0c3
Kircheis G, Knoche A, Hilger N et al (2009b) Hepatic encephalopathy and fitness to drive. Gastroenterology 137:1706–1715. doi:10.1053/j.gastro.2009.08.003
Li YY, Nie YQ, Sha WH et al (2004) Prevalence of subclinical hepatic encephalopathy in cirrhotic patients in China. World J Gastroenterol 10:2397–2401
Montagnese S, Amodio P, Morgan MY (2004) Methods for diagnosing hepatic encephalopathy in patients with cirrhosis: a multidimensional approach. Metab Brain Dis 19:281–312
Ortiz M, Jacas C, Cordoba J (2005) Minimal hepatic encephalopathy: diagnosis, clinical significance and recommendations. J Hepatol 42(Suppl):S45–S53. doi:10.1016/j.jhep.2004.11.028
Prasad S, Dhiman RK, Duseja A, Chawla YK, Sharma A, Agarwal R (2007) Lactulose improves cognitive functions and health-related quality of life in patients with cirrhosis who have minimal hepatic encephalopathy. Hepatology 45:549–559. doi:10.1002/hep.21533
Randolph C, Hilsabeck R, Kato A et al (2009) Neuropsychological assessment of hepatic encephalopathy: ishen practice guidelines. Liver Int 29:629–635. doi:10.1111/j.1478-3231.2009.02009.x
Roback GS, Krasno LR, Ivy AC (1952) Effect of analeptic drugs on the somnifacient effect of seconal and antihistaminics as measured by the flicker fusion threshold. J Appl Physiol 4:566–574
Romero-Gomez M (2010) Pharmacotherapy of hepatic encephalopathy in cirrhosis. Expert Opin Pharmacother 11:1317–1327. doi:10.1517/14656561003724721
Schomerus H, Hamster W (2001) Quality of life in cirrhotics with minimal hepatic encephalopathy. Metab Brain Dis 16:37–41
Sharma P, Sharma BC (2010) Predictors of minimal hepatic encephalopathy in patients with cirrhosis. Saudi J Gastroenterol 16:181–187. doi:10.4103/1319-3767.65189
Shukla S, Shukla A, Mehboob S, Guha S (2011) Meta-analysis: the effects of gut flora modulation using prebiotics, probiotics and synbiotics on minimal hepatic encephalopathy. Aliment Pharmacol Ther. doi:10.1111/j.1365-2036.2010.04574.x
Sjogren P, Olsen AK, Thomsen AB, Dalberg J (2000a) Neuropsychological performance in cancer patients: the role of oral opioids, pain and performance status. Pain 86:237–245
Sjogren P, Thomsen AB, Olsen AK (2000b) Impaired neuropsychological performance in chronic nonmalignant pain patients receiving long-term oral opioid therapy. J Pain Symptom Manage 19:100–108
Smith JM, Misiak H (1976) Critical flicker frequency (cff) and psychotropic drugs in normal human subjects-a review. Psychopharmacologia 47:175–182
Tygstrup N (1964) The galactose elimination capacity in control subjects and in patients with cirrhosis of the liver. Acta Med Scand 175:281–289
Acknowledgements
The authors wish to thank laboratory technicians I. Schjødt and B. Nielsen of the Department of Medicine V Clinical and Research Laboratory and Professor Michael Vaeth of the Institute of Biostatistics, Aarhus University.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lauridsen, M.M., Jepsen, P. & Vilstrup, H. Critical flicker frequency and continuous reaction times for the diagnosis of minimal hepatic encephalopathy. A comparative study of 154 patients with liver disease. Metab Brain Dis 26, 135–139 (2011). https://doi.org/10.1007/s11011-011-9242-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-011-9242-1