Abstract
Objectives
Many cisgender women affected by homelessness and substance use desire pregnancy and parenthood. Provider discomfort with patient-centered counseling about reproductive choices and supporting reproductive decisions of these women poses barriers to reproductive healthcare access.
Methods
We used participatory research methods to develop a half-day workshop for San Francisco-based medical and social service providers to improve reproductive counseling of women experiencing homelessness and/or who use substances. Guided by a stakeholder group comprising cisgender women with lived experience and providers, goals of the workshop included increasing provider empathy, advancing patient-centered reproductive health communication, and eliminating extraneous questions in care settings that perpetuate stigma. We used pre/post surveys to evaluate acceptability and effects of the workshop on participants’ attitudes and confidence in providing reproductive health counseling. We repeated surveys one month post-event to investigate lasting effects.
Results
Forty-two San Francisco-based medical and social service providers participated in the workshop. Compared to pre-test, post-test scores indicated reduced biases about: childbearing among unhoused women (p < 0.01), parenting intentions of pregnant women using substances (p = 0.03), and women not using contraception while using substances (p < 0.01). Participants also expressed increased confidence in how and when to discuss reproductive aspirations (p < 0.01) with clients. At one month, 90% of respondents reported the workshop was somewhat or very beneficial to their work, and 65% reported increased awareness of personal biases when working with this patient population.
Conclusions for Practice
A half-day workshop increased provider empathy and improved provider confidence in reproductive health counseling of women affected by homelessness and substance use.
Significance Statement
In the setting of significant trauma histories, untreated mental illness, and trauma directly related to housing instability, women experiencing homelessness (WEH) in the United States are also frequently affected by substance use. Facing stigma, judgment, mistreatment, and under-trained providers, WEH using substances often have limited access to reproductive health services and experience poor reproductive health outcomes. A half-day provider training, designed in collaboration with a stakeholder group of women with lived experience and community partners in San Francisco, CA increased provider empathy and improved provider confidence in reproductive health counseling of women affected by homelessness and substance use.
Similar content being viewed by others
Introduction
Cisgender women comprise a sizable share of people experiencing homelessness, with unsheltered homelessness growing by 5% among women and girls between 2020 and 2022 (U.S. Department of Housing & Urban Development, 2022), and face immense health and healthcare inequities. These include disproportionate rates of poor reproductive and pregnancy outcomes (Clark et al., 2019; DiTosto et al., 2021; St Martin et al., 2021) and inadequate and inconsistent access to reproductive health care (Corey et al., 2020; Dasari et al., 2016; Lewis et al., 2003; McGeough et al., 2020; Schmidt et al., 2023; Teruya et al., 2010). A number of interconnected individual and structural challenges contribute to these inequities, including lack of social support and stability, difficulty accessing and navigating unwelcoming healthcare and social service systems, fear of child welfare involvement and removal of children, and poor treatment in healthcare settings (Allen & Vottero, 2020; Frazer et al., 2019; Gelberg et al., 2004; McGeough et al., 2020; Schmidt et al., 2023).
Substance use disorders disproportionately affect people experiencing homelessness for myriad reasons. People experiencing homelessness may manage the trauma of homelessness with substance use, and access to substance use disorder treatment is more challenging in the setting of unstable housing (Frazer et al., 2019; Magwood et al., 2020). In addition, people experiencing homelessness have disproportionately experienced childhood trauma, which is associated with future substance use (Khoury et al., 2010; Liu et al., 2021; Magwood et al., 2020). Thus, women and other people capable of pregnancy experiencing homelessness may present to a diverse range of low-barrier healthcare settings, including homeless health outreach programs, drop-in centers, and substance use treatment facilities, with the desire to address a wide range of health issues including preconception care, pregnancy care, and pregnancy prevention.
Given complex access challenges, intentional, patient-centered interaction in these settings is critical to facilitate reproductive healthcare engagement. However, providers may have unchecked assumptions about reproductive aspirations and capabilities of people affected by homelessness and substance use that affect if and how they engage with women and other individuals about their reproductive goals and needs. Women experiencing homelessness and with substance use disorders have reported feeling dehumanized, disrespected and judged during reproductive health care encounters; receiving substandard care; feeling unable to advocate for themselves; and being coerced into contraception use (Begun et al., 2019; Dasari et al., 2016; Frazer et al., 2019; Kennedy et al., 2014; MacAfee et al., 2020; Sznajder-Murray & Slesnick, 2011; Terplan et al., 2015). Demeaning treatment from providers and a lack of agency in clinical spaces decreases trust and rapport (Azarmehr et al., 2018; Bloom et al., 2004). Thus, unsurprisingly, provider attitudes toward and poor treatment of women affected by homelessness and substance use has served as a barrier to entry and retention in care, in particular contraceptive care and antenatal care (Allen & Vottero, 2020; Begun et al., 2019; Kennedy et al., 2014; MacAfee et al., 2020; Sznajder-Murray & Slesnick, 2011).
Some limited evidence suggests that provider and staff training, promoting critical self-awareness of biases and attitudes, can improve care engagement of people experiencing homelessness (Aparicio et al., 2019; Rew et al., 2008). However, interventions addressing provider communication and biases toward the reproductive health and well-being of cisgender women and other people capable of pregnancy affected by substance use and homelessness are rare, and few incorporate the perspectives of affected individuals themselves. Recent work aimed at decreasing racial disparities in pregnancy and birth outcomes uplifts the importance of centering the voices of the impacted populations in defining reproductive care priorities and development of robust and just healthcare systems (Altman et al., 2020; Franck et al., 2020). These lessons resonate in the context of women affected by homelessness and substance use, whose reproduction is frequently devalued and who are rarely invited to engage in the development of care priorities.
Motivated by the voiced needs of affected women and under the guidance of a stakeholder group including individuals with lived experience, we developed a workshop to improve provider-patient reproductive health communication and address provider attitudes that may result in enacted stigma and discrimination. We hosted the workshop for providers who cisgender women frequently contacted: homelessness services providers, reproductive health providers, and substance use treatment providers. Here, we describe (1) workshop development in partnership with a community advisory board of relevant stakeholders; (2) a quasi-experimental, single group pretest–posttest questionnaire with one-month-post intervention follow-up; and (3) qualitative interviews with study participants to understand workshop acceptability and effect on provider attitude among providers serving women affected by homelessness and substance use in San Francisco, CA.
Methods
Workshop Development Process
To guide the intervention development, we conducted a 6-month needs assessment with cisgender women experiencing homelessness and using substances in San Francisco and the providers that serve them. This assessment is described elsewhere (Schmidt et al., 2023). Briefly, we found a striking disconnect between patients’ and providers’ recommendations to improve reproductive services for affected individuals: while provider recommendations focused on improving access, patients focused on improving patient-provider communication and respectful care. Guided by this discordance, we developed a community-informed intervention to educate providers.
Community-Driven Intervention Development
We used an iterative process to develop workshop content over six months, guided by semi-structured participatory discussions with a community stakeholder group. Group members (n = 10) were recruited to represent the experiences of people who had been pregnant while experiencing homelessness and/or using substance, and/or service providers in the areas of homelessness, substance use treatment, or reproductive health. The group convened for 2-h, monthly, and guided the workshop development process.
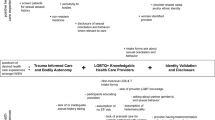
Through facilitated discussions and generative activities, we identified group priorities. The project manager took notes at each stakeholder group meeting and incorporated feedback into workshop development. Prominent themes included lack of respect and empathy during reproductive health care, provider anxiety about the complexity of client needs, triggering and harmful questions employed in care settings, and an overarching feeling of dehumanization in healthcare spaces. Based on these topic areas, we drafted a workshop outline (Fig. 1). Stakeholder group members then guided the development of interactive sessions to be held at the workshop and received training in facilitation.
The stakeholder group agreed that community stories were a critical addition to workshop content. We recruited community members to share personal stories about their experiences accessing and receiving reproductive health care services. A peer story-telling expert used qualitative interviewing techniques to elicit stories and develop them into scripts to be delivered at the workshop. Final scripts were reviewed and approved by each community member who contributed the story.
Workshop Structure
In consultation with the stakeholder group members and other key informants, we planned a four-hour workshop. Derived from priorities identified by the stakeholder group, goals of the workshop included: to increase provider empathy, advance patient-centered reproductive health communication, and eliminate extraneous questions in care settings that may perpetuate stigma or trauma (Fig. 1, column 2).
The workshop consisted of didactic, storytelling, and interactive sessions on managing personal biases and exploring intake and counseling approaches specific to women affected by homelessness and substance use (Fig. 1, column 3). Between each session, a member of the stakeholder group presented one of the scripted personal stories. Finally, participants received a description of and contact information for organizations represented in the room to facilitate knowledge of resources and motivate cross-agency collaboration.
Workshop Participant Recruitment
We recruited workshop participants who work at the nexus of homelessness services, substance use, and reproductive health. We employed a purposive sampling strategy, sending invitations to contacts in health and social service city agencies, university-affiliated programs, and non-profit organizations across San Francisco. We asked participants to register for the workshop and reviewed the proportion of providers working in different areas who registered during the registration period, so that we could conduct targeted outreach to under-represented agencies.
Study Design and Analysis
Our evaluation aimed to measure reaction, learning, and behavior change (Kirkpatrick, 1994). Participants completed questionnaires immediately before and after the workshop, providing responses about professional characteristics and pre-post attitude measures. Pre-post items were chosen to indicate degrees of bias toward reproductive aspirations of people experiencing homelessness or using substances and provider confidence on engaging around core topic areas with affected individuals. Items were measured on a 5-point Likert scale and adapted from existing measures (Fine et al., 2013; Goggin et al., 2018), and from themes identified in our local needs assessment. We also asked participants to complete a questionnaire one month after the workshop and invited participants to participate in semi-structured phone interviews about their workshop experience. Both the immediate- and one month-post questionnaires included short answer prompts as well as multiple-choice questions. We remunerated participants with a $20 gift card for completing the one-month follow-up survey and a $30 gift card for completing an in-depth interview.
We computed frequencies for all quantitative measures in Stata 14 (StataCorp LLC, College Station, TX). We calculated median scores and interquartile ranges for each pre/post-test measure of attitudes and confidence and used Wilcoxon sign tests to measure changes before and after the workshop and between directly post and one-month following the workshop.
Short answers and in-depth interviews were analyzed in Atlas.ti version 8 (Scientific Software Development GmbH, Berlin, Germany). Three authors developed a codebook based on a priori established domains. Codes were then applied by a single coder and refined based on emergent themes. Analysis was considered complete when no new themes emerged.
The evaluation protocol was reviewed and deemed exempt by the institutional review board of the University of California, San Francisco.
Results
Participant Professional Characteristics
Forty-two San Francisco-based medical and social service providers who work in reproductive health (70%), substance use (59%), and/or homelessness (80%) participated in the workshop in June 2019 (Table 1). Twenty-six percent were clinicians, (MDs or DOs), 29% were nurses, with additional representation from case managers and outreach workers, social workers, health services mangers, and health educators. Further professional characteristics are presented in Table 1.
Pre-Post Assessment
Compared to pre-test, post-test scores indicated a decrease in negative feelings about childbearing among women experiencing homelessness (p < 0.01), parenting intentions of women using substances during pregnancy (p < 0.05), and women not using contraception while using substances (p < 0.001; Table 2). Regarding assumptions about contraceptive need, respondents more frequently disagreed with the following statement after the workshop: “people experiencing homelessness do not use contraception because they don’t know where to access it” (p < 0.01). Additionally, participants expressed increased confidence in how and when to discuss substance use (p = 0.01) and reproductive aspirations (p < 0.01) with clients. Finally, post-test results indicated a trend towards participants feeling more overwhelmed by the life complexity of women experiencing homelessness (p < 0.10), though this was not statistically significant.
Impact Survey Findings
Thirty participants (71% of workshop participants) completed the one-month follow up survey. Of those participants, ninety percent reported that the workshop was somewhat or very beneficial to their work. Many participants reported that they continued to have increased confidence in when and how to initiate conversations about reproductive health (64%), substance use (55%), and housing status (52%) with clients experiencing homelessness and/or using substances (Table 3). Sixty-six percent reported increased awareness of personal biases when working with women affected by homelessness or substance use.
Interview Findings
We conducted follow-up interviews with eight workshop participants in July and August 2019: four with providers who work in homeless health, three in reproductive health, and one in substance use treatment. Interviews averaged 27 min. As a result of the workshop, participants indicated that they modified the ways that they ask questions, had greater awareness of personal biases, and initiated conversations within their organizations about revising protocols.
Some participants discussed reflecting on and refining the questions they ask clients. One participant, a lactation consultant, reported that she changed how she inquired about previous children after learning that the topic of children could be triggering for clients who may have experienced forced child separation. Others spoke more generally about a greater sense of intentionality when engaging with clients as a result of the workshop. A case manager working in homelessness health said:
Since our conversation at the workshop, I think it's been more on the back of my mind that when I'm asking a client for some information, am I asking it because I need that information, and it actually pertains, or do I not need that information, you know, for the activity that I need to do with this client?
She felt that this reflection and self-evaluation “helped solidify the way in which [she] would treat another client with more dignity, with more mindfulness, or for their rights as a client.”
Others described how the workshop helped them reflect on their own personal biases. Three interview participants reflected on their responses to the pre-post questionnaire and how their biases changed after the workshop:
There was a lot of questions about what do you think about homeless women who use [substances], who want to be pregnant. When I did [the pre-questionnaire], I was just like absolutely no. They should not. I think a lot of it wasn't coming from clients that I have worked with. I think it all came from personal bias. […] But, after hearing everyone speak, after going through the class, I thought that, you know, definitely my perspective has changed.
Many participants identified the story-telling activity of the workshop as instrumental in their reflection process. The above participant further described the importance of stories: they “have a really big impact on people that maybe aren't familiar with working with that population or have a lot of biases to kind of see it and not just read about. It's different, and it's powerful.”
Finally, several participants also shared what they learned with their organizations in order to make a broader impact. One participant who works in homeless health engaged her coworkers about record keeping practices:
I had good conversations with some colleagues around the questions piece […] When we're doing case notes, we're not over-indulging in terms of the narratives that we're creating for people. Don't make assumptions about things that you may be picking up on but really only document what happened.
Another participant reported working with her supervisor, who also attended the workshop, to integrate anti-bias activities into future trainings within their organization.
Discussion
This study demonstrates that a half-day training, developed in collaboration with a community and provider stakeholder group, resulted in decreased provider biases towards and increased provider confidence in addressing the reproductive health needs of women affected by homelessness and substance use. Key components of this workshop include its being developed in collaboration with a stakeholder group involving people with lived experience and inclusion of storytelling to increase providers’ empathy and decrease biases. Additionally, providers responded positively to having dedicated time to reflect in community with other providers and engage with intentional reflection on counseling approaches and the impact of standardized questions.
Provider bias in clinical decision making, particularly beliefs about who should or should not reproduce, can diminish reproductive autonomy and decrease healthcare utilization of marginalized and stigmatized groups. For example, providers may recommend and even pressure patients to use long-acting contraceptive methods because of judgment that, due to identity or circumstance, they should not become pregnant (Gomez et al., 2014; Holt et al., 2020). Studies have demonstrated that these patient-provider interactions can impact a variety of reproductive outcomes including future contraception use and birth experience (Altman et al., 2019; Dehlendorf et al., 2016). This holds true in the limited literature on unhoused cisgender women’s experiences accessing reproductive care, where, ultimately, biased treatment offered by providers creates barriers to entry and retention in care, including prenatal care and contraceptive services (Kennedy et al., 2014; Sznajder-Murray & Slesnick, 2011). Creating opportunities for providers to unpack their biases about the reproduction of people affected by homelessness and using substances and practice patient-centered care strategies may serve to uplift reproductive autonomy and encourage engagement in reproductive health services in diverse healthcare settings.
Centering the voices of those with lived experience in the development and execution of interventions serves to both challenge provider attitudes and ensure that interventions are relevant to the population being served (Julian et al., 2020). In this project, the stakeholder group set the workshop priorities, contributed intervention components, and reviewed and provided feedback on all components of the intervention. Including both individuals with lived experience with homelessness and substance involvement and providers who serve these communities as stakeholders in the process facilitated development of a nuanced intervention that prioritized affected women’s perspectives and respected the practical and emotional challenges of providers. The value of community-involved intervention development is reflected in our study results. Many participants stated that community perspectives and storytelling integrated into the training left the strongest impressions and may have had the greatest impact on provider attitudes. Involving providers, alongside individuals with lived experience, in our development process also allowed us to focus on key needs and intervention points uplifted by participants. Specifically, participants highlighted the importance of including intentional group time to reflect on and share uncertainties about serving patients with complex needs, and interrogating questions frequently asked in clinical encounters.
Interventions addressing patient-provider interactions are crucial and should be implemented together with actions to address structural barriers to care that impact person-centeredness. Our intervention addressed many areas desired by providers serving unhoused populations and people with substance use disorders, including resource sharing, networking, and a focus on empathy (Twis et al., 2021), as well as the priorities identified by our stakeholder group. However, after the workshop, participants reported feeling more overwhelmed by the complexity of the lives of affected clients. This finding is not surprising; there are few (if any) known interventions to address complex needs of this population in a time-limited setting. Interpersonal interventions, such as our project, should be integrated with structural changes to care delivery, both to improve patient-centered care and reduce provider burnout—a known result of providers’ feeling overwhelmed. For example, investing in gender-responsive, trauma-informed approaches to service delivery may both empower affected women to share their reproductive aspirations and feel heard and respected, while simultaneously improving support for providers (Covington et al., 2008; SAMHSA, 2014).
While the results of this evaluation show promise with respect to feasibility and short-term impact, our study had limitations. First, the workshop was conducted in San Francisco, where there has recently been an increase of health services focused on people experiencing homelessness and with substance use disorders. Our audience may have been primed to this topic and their receptivity may not be reflective of providers working in different contexts. Moreover, even within San Francisco, selection bias was likely at play as individuals elected (and were not required) to attend the workshop. Secondly, our community perspectives only included those of cisgender women. There is also, to our knowledge, no literature describing the reproductive aspirations and related healthcare needs of transgender people experiencing homelessness or using substances. Thus, while we used gender-neutral language during our pilot workshop, we did not account for the perspectives, or specific needs and challenges of transgender men and gender-expansive people at this intersection. We are not aware whether the workshop as framed would improve the care experience of these populations as they access reproductive health services.
Methodologically, our study included a small sample size, a lack of a control group, and attrition, which also limit transferability to other similar communities in different localities and contexts. In particular, individuals who did not complete the follow-up survey may have been less engaged in the workshop than those who chose to continue to participate, resulting in an over-estimation of impact. Results were based on self-report and could be exaggerated due to social desirability bias. Follow-up time was limited to one month, so we were unable to measure longer-term effects. Lastly, we did not directly measure provider behavior or how clients experienced counseling. Despite these limitations, this is one of the first attempts, to our knowledge, to create and measure the effects of a training specifically focused on reproductive health communication between providers and women experiencing homelessness and using substances. Our process was strengthened by the consistent contributions of community members through a patient-provider stakeholder group.
Conclusions
Our results suggest that a half-day, community-informed workshop can reduce provider bias and increase confidence in counseling about reproductive health topics for providers working with women experiencing homelessness and using substances across a range of settings. Engaging relevant community stakeholders in the development and delivery of provider training may ensure relevance and increase impact.
Data Availability
Data are not posted publicly. Qualitative transcripts contain professional details that could compromise the confidentiality of participants.
Code Availability
Code for descriptive analyses can be made available by request.
References
Allen, J., & Vottero, B. (2020). Experiences of homeless women in accessing health care in community-based settings: A qualitative systematic review. JBI Evidence Synthesis, 18(9), 1970–2010. https://doi.org/10.1124/JBISRIR-D-19-00214
Altman, M. R., Oseguera, T., McLemore, M. R., Kantrowitz-Gordon, I., Franck, L. S., & Lyndon, A. (2019). Information and power: Women of color’s experiences interacting with health care providers in pregnancy and birth. Social Science & Medicine, 238, 112491. https://doi.org/10.1016/j.socscimed.2019.112491
Altman, M. R., McLemore, M. R., Oseguera, T., Lyndon, A., & Franck, L. S. (2020). Listening to women: Recommendations from women of color to improve experiences in pregnancy and birth care. Journal of Midwifery & Women’s Health, 65(4), 466–473. https://doi.org/10.1111/jmwh.13102
Aparicio, E. M., Kachingwe, O. N., Phillips, D. R., Fleishman, J., Novick, J., Okimoto, T., Cabral, M. K., Ka’opua, L. S., Childers, C., Espero, J., & Anderson, K. (2019). Holistic, trauma-informed adolescent pregnancy prevention and sexual health promotion for female youth experiencing homelessness: Initial outcomes of Wahine Talk. Children and Youth Services Review, 107, 104509. https://doi.org/10.1016/j.childyouth.2019.104509
Azarmehr, H., Lowry, K., Sherman, A., Smith, C., & Zuñiga, J. A. (2018). Nursing practice strategies for prenatal care of homeless pregnant women. Nursing for Women’s Health, 22(6), 489–498. https://doi.org/10.1016/j.nwh.2018.09.005
Begun, S., Combs, K. M., Torrie, M., & Bender, K. (2019). “It seems kinda like a different language to us”: Homeless youths’ attitudes and experiences pertaining to condoms and contraceptives. Social Work in Health Care, 58(3), 237–257. https://doi.org/10.1080/00981389.2018.1544961
Bloom, K. C., Bednarzyk, M. S., Devitt, D. L., Renault, R. A., Teaman, V., & Loock, D. M. (2004). Barriers to prenatal care for homeless pregnant women. Journal of Obstetric, Gynecologic, and Neonatal Nursing: JOGNN, 33(4), 428–435.
Clark, R. E., Weinreb, L., Flahive, J. M., & Seifert, R. W. (2019). Homelessness contributes to pregnancy complications. Health Affairs (Project Hope), 38(1), 139–146. https://doi.org/10.1377/hlthaff.2018.05156
Corey, E., Frazin, S., Heywood, S., & Haider, S. (2020). Desire for and barriers to obtaining effective contraception among women experiencing homelessness. Contraception and Reproductive Medicine, 5(1), 12. https://doi.org/10.1186/s40834-020-00113-w
Covington, S. S., Burke, C., Keaton, S., & Norcott, C. (2008). Evaluation of a trauma-informed and gender-responsive intervention for women in drug treatment. Journal of Psychoactive Drugs, 40(5), 387–398. https://doi.org/10.1080/02791072.2008.10400666
Dasari, M., Borrero, S., Akers, A. Y., Sucato, G. S., Dick, R., Hicks, A., & Miller, E. (2016). Barriers to long-acting reversible contraceptive uptake among homeless young women. Journal of Pediatric and Adolescent Gynecology, 29(2), 104–110. https://doi.org/10.1016/j.jpag.2015.07.003
Dehlendorf, C., Henderson, J. T., Vittinghoff, E., Grumbach, K., Levy, K., Schmittdiel, J., Lee, J., Schillinger, D., & Steinauer, J. (2016). Association of the quality of interpersonal care during family planning counseling with contraceptive use. American Journal of Obstetrics and Gynecology, 215(1), 78.e1-78.e9. https://doi.org/10.1016/j.ajog.2016.01.173
DiTosto, J. D., Holder, K., Soyemi, E., Beestrum, M., & Yee, L. M. (2021). Housing instability and adverse perinatal outcomes: A systematic review. American Journal of Obstetrics & Gynecology MFM, 3(6), 100477. https://doi.org/10.1016/j.ajogmf.2021.100477
Fine, A. G., Zhang, T., & Hwang, S. W. (2013). Attitudes towards homeless people among emergency department teachers and learners: A cross-sectional study of medical students and emergency physicians. BMC Medical Education, 13(1), 112. https://doi.org/10.1186/1472-6920-13-112
Franck, L. S., McLemore, M. R., Williams, S., Millar, K., Gordon, A. Y., Williams, S., Woods, N., Edwards, L., Pacheco, T., Padilla, A., Nelson, F., & Rand, L. (2020). Research priorities of women at risk for preterm birth: Findings and a call to action. BMC Pregnancy and Childbirth, 20(1), 10. https://doi.org/10.1186/s12884-019-2664-1
Frazer, Z., McConnell, K., & Jansson, L. M. (2019). Treatment for substance use disorders in pregnant women: Motivators and barriers. Drug and Alcohol Dependence, 205, 107652. https://doi.org/10.1016/j.drugalcdep.2019.107652
Gelberg, L., Browner, C. H., Lejano, E., & Arangua, L. (2004). Access to women’s health care: A qualitative study of barriers perceived by homeless women. Women & Health, 40(2), 87–100. https://doi.org/10.1300/J013v40n02_06
Goggin, K., Hurley, E. A., Wagner, G. J., Staggs, V., Finocchario-Kessler, S., Beyeza-Kashesya, J., Mindry, D., Birungi, J., & Wanyenze, R. K. (2018). Changes in providers’ self-efficacy and intentions to provide safer conception counseling over 24 months. AIDS and Behavior, 22(9), 2895–2905. https://doi.org/10.1007/s10461-018-2049-x
Gomez, A. M., Fuentes, L., & Allina, A. (2014). Women or LARC First? Reproductive autonomy and the promotion of long-acting reversible contraceptive methods. Perspectives on Sexual and Reproductive Health, 46(3), 171–175. https://doi.org/10.1363/46e1614
Holt, K., Reed, R., Crear-Perry, J., Scott, C., Wulf, S., & Dehlendorf, C. (2020). Beyond same-day long-acting reversible contraceptive access A person-centered framework for advancing high-quality equitable contraceptive care. American Journal of Obstetrics and Gynecology, 222(4), S878.e1-S878.e6. https://doi.org/10.1016/j.ajog.2019.11.1279
Julian, Z., Robles, D., Whetstone, S., Perritt, J. B., Jackson, A. V., Hardeman, R. R., & Scott, K. A. (2020). Community-informed models of perinatal and reproductive health services provision: A justice-centered paradigm toward equity among Black birthing communities. Seminars in Perinatology, 44(5), 151267. https://doi.org/10.1016/j.semperi.2020.151267
Kennedy, S., Grewal, M., Roberts, E. M., Steinauer, J., & Dehlendorf, C. (2014). A qualitative study of pregnancy intention and the use of contraception among homeless women with children. Journal of Health Care for the Poor and Underserved, 25(2), 757–770. https://doi.org/10.1353/hpu.2014.0079
Khoury, L., Tang, Y. L., Bradley, B., Cubells, J. F., & Ressler, K. J. (2010). Substance use, childhood traumatic experience, and posttraumatic stress disorder in an urban civilian population. Depression and Anxiety, 27(12), 1077–1086. https://doi.org/10.1002/da.20751
Kirkpatrick, D. L. (1994). Evaluating training programs: The four levels. San Fancisco, CA: Berret-Koehler Publishers, Inc.
Lewis, J. H., Andersen, R. M., & Gelberg, L. (2003). Health care for homeless women. Journal of General Internal Medicine, 18(11), 921–928. https://doi.org/10.1046/j.1525-1497.2003.20909.x
Liu, M., Luong, L., Lachaud, J., Edalati, H., Reeves, A., & Hwang, S. W. (2021). Adverse childhood experiences and related outcomes among adults experiencing homelessness: A systematic review and meta-analysis. The Lancet Public Health, 6(11), e836–e847. https://doi.org/10.1016/S2468-2667(21)00189-4
MacAfee, L. K., Harfmann, R. F., Cannon, L. M., Kolenic, G., Kusunoki, Y., Terplan, M., & Dalton, V. K. (2020). Sexual and reproductive health characteristics of women in substance use treatment in michigan. Obstetrics & Gynecology, 135(2), 361–369. https://doi.org/10.1097/AOG.0000000000003666
Magwood, O., Salvalaggio, G., Beder, M., Kendall, C., Kpade, V., Daghmach, W., Habonimana, G., Marshall, Z., Snyder, E., O’Shea, T., Lennox, R., Hsu, H., Tugwell, P., & Pottie, K. (2020). The effectiveness of substance use interventions for homeless and vulnerably housed persons: A systematic review of systematic reviews on supervised consumption facilities, managed alcohol programs, and pharmacological agents for opioid use disorder. PLOS ONE, 15(1), e0227298. https://doi.org/10.1371/journal.pone.0227298
McGeough, C., Walsh, A., & Clyne, B. (2020). Barriers and facilitators perceived by women while homeless and pregnant in accessing antenatal and or postnatal healthcare: A qualitative evidence synthesis. Health & Social Care in the Community, 28(5), 1380–1393. https://doi.org/10.1111/hsc.12972
Rew, L., Rochlen, A. B., & Murphey, C. (2008). Health educators’ perceptions of a sexual health intervention for homeless adolescents. Patient Education and Counseling, 72(1), 71–77. https://doi.org/10.1016/j.pec.2008.01.022
Schmidt, C. N., Wingo, E. E., Newmann, S. J., Borne, D. E., Shapiro, B. J., & Seidman, D. L. (2023). Patient and provider perspectives on barriers and facilitators to reproductive healthcare access for women experiencing homelessness with substance use disorders in San Francisco. Women’s Health, 19, 174550572311523. https://doi.org/10.1177/17455057231152374
St Martin, B. S., Spiegel, A. M., Sie, L., Leonard, S. A., Seidman, D., Girsen, A. I., Shaw, G. M., & El-Sayed, Y. Y. (2021). Homelessness in pregnancy: Perinatal outcomes. Journal of Perinatology: Official Journal of the California Perinatal Association, 41(12), 2742–2748. https://doi.org/10.1038/s41372-021-01187-3
Substance Abuse and Mental Health Services Administration. (2014). SAMHSA’s Concept of Trauma and Guidance for a Trauma-Informed Approach (HHS Publication No. (SMA) 14–4884). Substance Abuse and Mental Health Services Administration.
Sznajder-Murray, B., & Slesnick, N. (2011). “Don’t Leave Me Hanging”: Homeless Mothers’ perceptions of service providers. Journal of Social Service Research, 37(5), 457–468. https://doi.org/10.1080/01488376.2011.585326
Terplan, M., Kennedy-Hendricks, A., & Chisolm, M. S. (2015). Article commentary: Prenatal substance use: Exploring assumptions of maternal unfitness. Substance Abuse: Research and Treatment. https://doi.org/10.4137/SART.S23328
Teruya, C., Longshore, D., Andersen, R. M., Arangua, L., Nyamathi, A., Leake, B., & Gelberg, L. (2010). Health and health care disparities among homeless women. Women & Health, 50(8), 719–736. https://doi.org/10.1080/03630242.2010.532754
Twis, M. K., Petrovich, J. C., Emily, D., Evans, S., & Addicks, L. A. (2021). Training preferences of homelessness assistance service providers: A brief report. Journal of Social Distress and Homelessness. https://doi.org/10.1080/10530789.2021.1917934
U.S. Department of Housing and Urban Development. (2022). The 2022 Annual Homeless Assessment Report. Retrieved, from https://www.huduser.gov/portal/sites/default/files/pdf/2022-AHAR-Part-1.pdf
Acknowledgements
The authors are incredibly grateful for the advisors without whom this work would not be possible. We would also like to thank additional experts who provided advice, materials, and facilitation contributions to this project: Carrie Hamilton, Mary Howe, Shivaun Nestor, Alissa Perrucci, and Karen Scott. We are indebted to Nora Anderson for coordinating the first phase of this study and Caroline Watson for gathering and cultivating community stories. Lastly, we would like to thank all the community members and service providers in San Francisco that shared their candid opinions and experiences with us.
Funding
This research was supported by a grant from the Society of Family Planning (SFPRF 11-I15). The sponsor had no involvement in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the article for publication. The views and opinions expressed are those of the authors, and do not necessarily represent the views and opinions of the Society of Family Planning Research Fund.
Author information
Authors and Affiliations
Contributions
All authors contributed to the development and design of the project. Ms. Wingo led intervention and evaluation design, data collection, data analysis and manuscript drafting. Drs. Seidman and Newmann designed the research question, oversaw all aspects of intervention development and development of evaluation instruments, and contributed to manuscript development. Drs. Borne and Shapiro contributed to the design of the workshop and evaluation materials and reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
The research protocol was reviewed and deemed exempt by the institutional review board of University of California San Francisco.
Consent to Participate and for Publication
Given the low risk of the project, workshop participants provided verbal consent to participate in pre- and post-survey procedures at the time of registering for the workshop. This consent contained language that survey results would be used in publication. Participants who opted into one-month follow up qualitative interviews completed a separate verbal consent to participate in those procedures and consented to the use of those data for research purposes.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wingo, E.E., Newmann, S.J., Borne, D.E. et al. Improving Reproductive Health Communication Between Providers and Women Affected by Homelessness and Substance Use in San Francisco: Results from a Community-Informed Workshop. Matern Child Health J 27 (Suppl 1), 143–152 (2023). https://doi.org/10.1007/s10995-023-03671-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-023-03671-y