Abstract
Comorbidity of depression and substance abuse is common and a major public health burden. Studies of this form of comorbidity in racial and ethnic minoritized (REM) populations are minimal and have mixed findings. The present study examined the effect of general risk factors (family bonding, supervision, involvement, peer delinquency), depression risk factors (caregiver depression), and substance use risk factors (adult family members, sibling, and peer substance use) in early adolescence (~ ages 13–14) on comorbid depression and substance use in later adolescence (~ ages 15–17) and adulthood (~ ages 29–31) and continuity in comorbidity from adolescence to adulthood. Longitudinal data on 1000 Black (n = 680) Hispanic (n = 170) and White (n = 150) individuals came from the Rochester Youth Development Study. Participants were interviewed 14 times over 17 years beginning in 1988. General risk factors predicted comorbidity across racial/ethnic groups. Substance specific risk predicted comorbidity among Black and Hispanic individuals whereas depression specific risk was predictive among White individuals. Adolescent comorbidity predicted comorbidity in adulthood across race. These findings highlight the importance of substance use intervention for racial and ethnic minoritized individuals and mental health risk factors in Whites. The continuity of comorbidity from adolescence to adulthood highlights the importance of targeting adolescents for intervention to prevent long-term manifestation of this form of comorbidity and its associated consequences.



Similar content being viewed by others
References
Assari, S., Mistry, R., Caldwell, C. H., & Zimmerman, M. A. (2018). Marijuana use and depressive symptoms; gender differences in African American adolescents. Frontiers in Psychology, 9, 2135. https://doi.org/10.3389/fpsyg.2018.02135.
Bailey, J. A., Hill, K. G., Meacham, M. C., Young, S. E., & Hawkins, J. D. (2011). Strategies for characterizing complex phenotypes and environments: General and specific family environmental predictors of young adult tobacco dependence, alcohol use disorder, and co-occurring problems. Drug and Alcohol Dependence, 118(2–3), 444–451. https://doi.org/10.1016/j.drugalcdep.2011.05.002.
Bailey, J. A., Samek, D. R., Keyes, M. A., Hill, K. G., Hicks, B. M., McGue, M., & Hawkins, J. D. (2014). General and substance-specific predictors of young adult nicotine dependence, alcohol use disorder, and problem behavior: Replication in two samples. Drug and Alcohol Dependence, 138, 161–168.
Bailey, J. A., Epstein, M., Steeger, C. M., & Hill, K. G. (2018). Concurrent and prospective associations between Substance-Specific Parenting practices and child cigarette, Alcohol, and Marijuana Use. Journal of Adolescent Health, 62(6), 681–687. https://doi.org/10.1016/j.jadohealth.2017.11.290.
Buka, S. L. (2002). Disparities in health status and substance use: Ethnicity and socioeconomic factors. Public Health Reports, 117(Suppl 1), S118.
Chen, P., & Jacobson, K. C. (2012). Developmental trajectories of substance use from early adolescence to young adulthood: Gender and racial/ethnic differences. Journal of Adolescent Health, 50(2), 154–163.
Costello, E. J., Mustillo, S., Erkanli, A., Keeler, G., & Angold, A. (2003). Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry, 60(8), 837–844.
Cronley, C., White, H. R., Mun, E. Y., Lee, C., Finlay, A., & Loeber, R. (2012). Exploring the intersection of neighborhood racial and economic composition and individual race on substance use among male adolescents. Journal of Ethnicity in Substance Abuse, 11(1), 52–74.
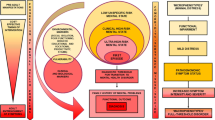
Epstein, M., Hill, K. G., Bailey, J. A., & Hawkins, D. J. (2013). The effect of general and drug-specific family environments on comorbid and drug-specific problem behavior: A longitudinal examination. Developmental Psychology, 49(6), 1151. https://doi.org/10.1037/a0029309.
Farahmand, P., Arshed, A., & Bradley, M. V. (2020). Systemic racism and substance use disorders. Psychiatric Annals, 50(11), 494–498.
Frohlich, K. L., & Potvin, L. (2008). Transcending the known in public health practice: The inequality paradox: The population approach and vulnerable populations. American Journal of Public Health, 98(2), 216–221.
Goodman, S. H. (2020). Intergenerational transmission of depression. Annual Review of Clinical Psychology, 16, 213–238.
Green, K. M., Zebrak, K. A., Fothergill, K. E., Robertson, J. A., & Ensminger, M. E. (2012). Childhood and adolescent risk factors for comorbid depression and substance use disorders in adulthood. Addictive Behaviors, 37(11), 1240–1247.
Heerde, J. A., Bailey, J. A., Toumbourou, J. W., & Catalano, R. F. (2019). Longitudinal associations between the adolescent family environment and young adult substance use in Australia and the United States. Frontiers in Psychiatry, 10, 821.
Hudson, W. W. (1982). A measurement package for clinical workers. The Journal of Applied Behavioral Science, 18(2), 229–238.
Hunt, G. E., Malhi, G. S., Lai, H. M. X., & Cleary, M. (2020). Prevalence of comorbid substance use in major depressive disorder in community and clinical settings, 1990–2019: Systematic review and meta-analysis. Journal of Affective Disorders, 266, 288–304.
Hussong, A. M., Ennett, S. T., Cox, M. J., & Haroon, M. (2017). A systematic review of the unique prospective association of negative affect symptoms and adolescent substance use controlling for externalizing symptoms. Psychology of Addictive Behaviors, 31(2), 137.
Johnson, R. M., Fairman, B., Gilreath, T., Xuan, Z., Rothman, E. F., Parnham, T., & Furr-Holden, C. D. M. (2015). Past 15-year trends in adolescent marijuana use: Differences by race/ethnicity and sex. Drug and Alcohol Dependence, 155, 8–15. https://doi.org/10.1016/j.drugalcdep.2015.08.025.
Jones, T. M., Epstein, M., Hill, K. G., Bailey, J. A., & Hawkins, J. D. (2019). General and specific predictors of comorbid substance use and internalizing problems from adolescence to age 33. Prevention Science, 20(5), 705–714.
Kerr, D. C., Tiberio, S. S., Capaldi, D. M., & Owen, L. D. (2020). Paternal and maternal prescription opioid use and misuse: General and specific risks for early adolescents’ substance use. Addictive Behaviors, 103, 106248.
Kim, G., DeCoster, J., Huang, C. H., & Chiriboga, D. A. (2011). Race/ethnicity and the factor structure of the Center for epidemiologic studies Depression Scale: A meta-analysis. Cultural Diversity and Ethnic Minority Psychology, 17(4), 381.
Köck, P., Meyer, M., Elsner, J., Dürsteler, K. M., Vogel, M., & Walter, M. (2022). Co-occurring mental disorders in transitional aged youth with substance use disorders–a narrative review. Frontiers in Psychiatry, 13, 827658.
Lai, H. M. X., Cleary, M., Sitharthan, T., & Hunt, G. E. (2015). Prevalence of comorbid substance use, anxiety and mood disorders in epidemiological surveys, 1990–2014: A systematic review and meta-analysis. Drug and Alcohol Dependence, 154, 1–13.
Marçal, K. (2020). Caregiver depression and child behaviour problems: A longitudinal mixed effects approach. Child & Family Social Work. https://doi.org/10.1111/cfs.12786.
Mulia, N., Ye, Y., Greenfield, T. K., & Zemore, S. E. (2009). Disparities in alcohol-related problems among White, Black, and hispanic americans. Alcoholism: Clinical and Experimental Research, 33(4), 654–662.
Nam, E., Matejkowski, J., & Lee, S. (2017). Racial/ethnic differences in contemporaneous use of mental health and substance use treatment among individuals experiencing both mental illness and substance use disorders. Psychiatric Quarterly, 88(1), 185–198.
Phelan, J. C., & Link, B. G. (2015). Is racism a fundamental cause of inequalities in health? Annual Review of Sociology, 41, 311–330.
Pinedo, M. (2019). A current re-examination of racial/ethnic disparities in the use of substance abuse treatment: Do disparities persist? Drug and Alcohol Dependence, 202, 162–167.
Radloff, L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401.
Rao, U. (2006). Links between depression and substance abuse in adolescents neurobiological mechanisms. American Journal of Preventive Medicine, 31(6), 161–174.
Reskin, B. (2012). The race discrimination system. Annual Review of Sociology, 38, 17–35.
Rice, F., Harold, G. T., & Thapar, A. (2002). Assessing the effects of age, sex and shared environment on the genetic etiology of depression in childhood and adolescence. Journal of Child Psychology and Psychiatry, 43(8), 1039–1051.
Schulenberg, J., Patrick, M. E., Maslowsky, J., & Maggs, J. L. (2014). Handbook of Developmental Psychopathology. 601–620.
Shafer, K., Fielding, B., & Wendt, D. (2017). Similarities and differences in the Influence of Paternal and maternal depression on Adolescent Well-Being. Social Work Research, 41(2), 85–96. https://doi.org/10.1093/swr/svx006.
Siennick, S. E., Widdowson, A. O., Woessner, M., & Feinberg, M. E. (2016). Internalizing symptoms, peer substance use, and substance use initiation. Journal of Research on Adolescence, 26(4), 645–657.
Stone, A. L., Becker, L. G., Huber, A. M., & Catalano, R. F. (2012). Review of risk and protective factors of substance use and problem use in emerging adulthood. Addictive Behaviors, 37(7), 747–775.
Substance Abuse and Mental Health Services Administration. (2020). Key substance use and mental health indicators in the United States: Results from the 2019 National Survey on Drug Use and Health (HHS Publication No. PEP20-07-01-001, NSDUH Series H-55). Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/data/.
Thornberry, T. P., Henry, K. L., Krohn, M. D., Lizotte, A. J., & Nadel, E. L. (2018). Key findings from the Rochester intergenerational study. Intergenerational Continuity of Criminal and Antisocial Behavior: An International Overview of Current Studies. London, England: Routledge.
United Nations Office on Drugs and Crime (2022). Comorbidities in Drug Use Disorders: No Wrong Door; Discussion Paper: Pre-pubication draft. Commission on Narcotic Drugs, Sixty Fifth Session Vienna. https://www.unodc.org/documents/drug-prevention-and-treatmentes.pdf.
van Buuren, S., & Groothuis-Oudshoorn, K. (2011). Mice: Multivariate imputation by chained equations in R. Journal of Statistical Software, 45(3), 1–67. https://doi.org/10.18637/jss.v045.i03.
Vasilenko, S. A., Evans-Polce, R. J., & Lanza, S. T. (2017). Age trends in rates of substance use disorders across ages 18–90: Differences by gender and race/ethnicity. Drug and Alcohol Dependence, 180, 260–264.
Vilsaint, C. L., NeMoyer, A., Fillbrunn, M., Sadikova, E., Kessler, R. C., Sampson, N. A., & Alegría, M. (2019). Racial/ethnic differences in 12-month prevalence and persistence of mood, anxiety, and substance use disorders: Variation by nativity and socioeconomic status. Comprehensive Psychiatry, 89, 52–60. https://doi.org/10.1016/j.comppsych.2018.12.008.
Whitehead, N. E., Trenz, R. C., Keen, L., Rose, J., & Latimer, W. W. (2014). Younger versus older African americans: Patterns and prevalence of recent illicit drug use. Journal of Ethnicity in Substance Abuse, 13(2), 126–138.
World Health Organization. (2017).Depression and other common mental disorders: Global health estimates (No. WHO/MSD/MER/2017.2). World Health Organization.
Yap, M. B. H., Pilkington, P. D., Ryan, S. M., & Jorm, A. F. (2014). Parental factors associated with depression and anxiety in young people: A systematic review and meta-analysis. Journal of Affective Disorders, 156, 8–23. https://doi.org/10.1016/j.jad.2013.11.007.
Acknowledgements
Support for the Rochester Youth Development Study has been provided by the National Institute on Drug Abuse (R01DA020195, R01DA005512), the Office of Juvenile Justice and Delinquency Prevention (86-JN-CX-0007, 96-MU-FX-0014, 2004-MU-FX-0062), the National Science Foundation (SBR-9123299), and the National Institute of Mental Health (R01MH56486, R01MH63386). Points of view or opinions in this document are those of the authors and do not necessarily represent the official position or policies of the funding agencies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
The questionnaire and methodology for this study were approved by the Human Research Ethics Committee of the University of Albany (Protocol # 19F011). Some parts of the RYDS study are publicly available. Phase I of RYDS is currently available through ICPSR. Phase 2 and Phase 3 are in review for potential archival, upon approval by the original funders. Informed consent was obtained from all individual participants included in the study.
Conflict of interest
All authors certify that they have no conflicts of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jones, T.M., Augustyn, M. & Henry, K.L. Progression of Comorbid Depression and Substance Use among Racially Diverse Adults. J of Prevention 45, 287–302 (2024). https://doi.org/10.1007/s10935-024-00767-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10935-024-00767-1