Abstract
Studies exploring associations between children with Autism Spectrum Disorder (ASD) and depression in parents are limited. This study compares healthcare utilization, depression treatment costs, and risk factors, in parents of children with and without ASD. Using a matched case-control, individuals aged 27 to 64 with continuous enrollment from 2017–2019 and a child diagnosed with ASD were selected from nationally representative administrative claims data. Individuals were randomly matched 1:3 to a non-ASD group based on the child's age, gender, and family characteristics. Statistical models were used to evaluate the association between ASD in children, depression in their respective parents, and resulting healthcare utilization and costs incurred by parents. The study consisted of 23,316 families, out of which 5,779 had children with ASD, and 17,337 had children without ASD. Having a child with ASD was a predictor of depression in parents (OR 1.91, 95% CI 1.73 – 2.10). Mothers of children with ASD had a higher risk of having depression (OR 4.0, 95% CI 2.62 – 6.12). Parents having multiple ASD children were also at higher risk of depression (OR 1.6, 95% CI 1.18 – 2.13). The sex and age of the child were not associated with parental depression. While family-level income and education attainment were not associated, urbanicity (rural) had an association with depression. Parents with ASD children are at a higher risk of depression. Findings suggest that parents of children with ASD may benefit from depression screening at the onset of ASD diagnosis in their children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The prevalence of autism has been steadily increasing over the past decade (Stevenson & Correa, 2019). Using nationally representative data a research study estimated Autism Spectrum Disorder (ASD) prevalence at 3.14%among US children and adolescents in the US in 2019 and 2020 ( Li et al., 2022). ASD is typically diagnosed between 18 months and three years and is characterized by severe impairment in several functioning areas, including communication, behavior, and socialization (Luther et al., 2005). A child with autism presents unique challenges and stressors to the family because of the ambiguity of diagnosis, the severity and duration of the disorder, and problems with the child's lack of adherence to social norms (Altiere & Von Kluge, 2009). The cost of caring for an individual with ASD ranges from $1.5 to $2.6 million throughout a lifetime (Candon et al., 2019). State legislatures passed mandates in 46 states from 2001–2017 requiring insurance companies to cover services associated with ASD. However, most insurance companies are hesitant to cover high costs of Applied Behavior Analysis (ABA) services, citing that ABA services are experimental and are not "medically necessary" (Callaghan & Sylvester, 2019).
Parenting a child with autism can be more stressful than parenting a child with a chronic illness or other developmental disability (Luther et al., 2005). Parents of children with ASD endure substantial financial burdens in high out-of-pocket costs and decreased workforce environment (Lavelle et al., 2014). Caregivers are more likely to experience mental health problems like stress-related conditions and depression (Koyanagi et al., 2018). Caregivers who provide care to a chronically ill family member at home are potentially at risk for care giver burden and declining physical and mental health (Chang et al., 2010). With demand for family caregivers expected to rise by 85% over the next few decades, supporting family caregivers has recently emerged as a national public health priority (Collins & Swartz, 2011). Caregivers of children with ASD reported many unmet needs, including financial and employment burdens (Vohra et al., 2014). Caregivers of ASD children suffer from poor health outcomes compared to the caregivers of children without ASD (Vohra et al., 2014). Family caregivers save American healthcare systems $350 billion annually, however their experiences must be investigated in order to provide appropriate support (Bastawrous, 2013). Thus, one could argue that primary care providers should use a family-centered perspective for identifying caregiver needs, strengths, and resources.
Depression is a leading cause of disability globally, and its prevalence has increased by 18.4% between 2005 and 2015 (Friedrich, 2017). It is associated with high societal costs and more significant functional impairment than many other chronic diseases, including diabetes and arthritis (Brody et al., 2018). Depression is the most expensive mental health disorder in USA with a lifetime prevalence of 20.6% with estimated treatment expenditures ranging widely from $17.1 to $238.3 billion Breslow et al., 2019).
A study by Weinberger et al. (2018) suggests that environmental changes, such as having a child with ASD, are more likely the cause of the increase of depression incidence than biological/genetic factors The authors also suggested that further research is needed to understand the contributing factors to the increase in depression and its impact on healthcare utilization and treatment costs. Thus, the comorbid condition of depression with another psychopathology may exacerbate parenting difficulties, and further research is needed to understand the broad array of child health and development outcomes affected by exposure to a depressed parent (Ertel et al., 2011).
ASD diagnosis is associated with an additional $3,400 in annual healthcare costs and $16,000 in annual non-health care costs (Candon et al., 2019). Applied Behavioral Analysis (ABA) treatment services for ASD costs vary dramatically between $10,000 and $100,000 per year based on severity and state of residence (Callaghan & Sylvester, 2019). Many of the ASD treatment costs have not been covered by insurance companies and instead have been shifted to the parents and families of individuals with ASD (Callaghan & Sylvester, 2019). We hypothesize that the parents of autistic children will be associated with a higher risk of depression than parents with children without an ASD diagnosis. Moreover, in families with ASD children and parental depression, we hypothesize that the competing healthcare needs could be associated with difference in healthcare utilization and cost trends.
Methods and Data
Optum Clinformatics Data Mart ® (CDM) from January 1, 2015, to December 31, 2019, provided inpatient, outpatient, and pharmacy claims data from employer-based and commercially insured individuals in the 50 US states. This database does not have socio-economic indicators like members' education attainment, residence-level income, race, or region. Large sample sizes available from claims can contribute substantively to advancing critical questions in ASD research (Burke et al., 2014). Administrative data are increasingly used to conduct research on depression and inform health services and health policy (Fiest et al., 2014).
The U.S. Census Bureau's American Community Survey (ACS) website, which is publicly available, provides zip code-level socio-economic indicators. We matched the member zip codes from the CDM database to the ACS data's zip codes to abstract education and family-level income information for the study individuals.
Similarly, the U.S. Department of Agriculture's Rural–Urban Commuting Codes (RUCA) website provided a crosswalk data set to abstract urbanicity (urban/suburban/rural categories) for the enrolled parents.
Sample
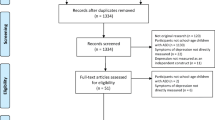
The sample frame consists of all members enrolled in the commercial insurance plans in the Optum Clinformatics® data mart between 2015 and 2019. We included unique subscribers and eligible dependents (hereafter referred to as unique families) with continuous enrollment between 1/1/2015 and 12/31/2019. The study period for outcomes was from 1/1/2017 and 12/31/2019. However, to identify children with ASD, a two year look back was used. We excluded all families where the parent had a depression diagnosis between 1/1/2016 and 12/31/2016. This partially addresses the temporal relationship between the ASD diagnosis in the child and the onset of depression in their respective parents. We also excluded individuals enrolled in non-commercial plans (i.e., Medicare) and those with no dependent children under 18 years were enrolled. Figure 1 depicts the selection criteria.
The sample population consisted of 1) enrollees aged 27–62 years with continuous enrollment between 2017 and 2019 and dependent children less than 18 years of age as of 1/1/2017 and an ASD diagnosis, and 2) a group of enrollees with children without an ASD diagnosis matched in 1:3 ratio on ASD child’s age, gender, parents’ enrollment status, and family-level income. We defined the period between 1/1/2015 and 12/31/2017 as a lookback period and between 1/1/2017 and 12/31/2019 as the study period during which all outcomes were measured. We used methods similar to Epperson et al. (2020) to randomly match without replacing in a 1:3 ratio, resulting in a non-ASD group consisting of 29,547 parents.
ASD-group Selection
ASD-group were defined as parents having children diagnosed with ASD if the child had at least one inpatient or two separate outpatient claims in any year between January 1, 2015, and December 31, 2019. ASD diagnosis is defined as having the values of F84.0 or F84.5 or F84.9 using the International Classification of Disease, 10th Edition (ICD-10-CM) codes or 299.0 or 299.8 or 299.9 using the International Classification of Disease, 9th Edition (ICD-9-CM) documented in the primary or secondary diagnosis of the inpatient or outpatient claim (Cohrs & Leslie, 2017). The presence of one or more of the ICD-10 or ICD-9 codes for ASD during the lookback and study period was considered sufficient to identify ASD diagnosis. If the parent had more than one child with ASD, the oldest child was kept in the cohort, and the fact that the parent had more than one ASD child was documented.
Depression diagnosis is defined as having the values of F32.0 – F33.9 using the International Classification of Disease, 10th Edition (ICD-10-CM) or values of 296.2, 296.3, 296.9, 300.4, 301.1, or 311 using the International Classification of Disease, 9th Edition (ICD-9-CM) documented in the primary or secondary diagnosis of the inpatient or outpatient claim. Any parents with a depression diagnosis during the lookback period of 1/1/2016 through 12/31/2016 were excluded from the sample.
Study Variables
An indicator variable to identify whether the parent(s) had a child with ASD was coded for every parent. Similarly, an indicator variable was created indicating if the parent(s) had a depression diagnosis. We adopted methods used by Croen et al. (2007) and defined utilization across five categories: 1) facility inpatient visits, 2) facility outpatient visits, 3) professional office visits, 4) emergency department (ED) visits, and 5) number of pharmacy prescriptions. We aggregated the number of visits across each of these categories. Using the “allowed amount,” we aggregated costs across the same five categories. The cost variable is the mean annual cost per parent, calculated based on costs for the three years of study period from 1/1/2017 through 12/31/2019.
Covariates
Earlier studies (Cohrs & Leslie, 2017) indicated that the age and sex of the child with ASD, number of children with ASD in the family, enrollment status of parents (single parents vs. both parents), education attainment and residence-level income level, and the urbanicity are known to influence the outcome measure as covariates. As such, child’s age (3–6, 7–10, 11–14, 15–18) and gender, parent’s age (27–34, 35–44, 45–54, 55–64) age and gender, multiple children in the family, parent enrollment status (single vs. both parents enrolled), and zip code in the Optum CDM database were used as covariates. We matched the zip code from the CDM with the ACS data set to abstract income (< $25,000, $-25,001-$50,000, $50,001-$75,000, > $75,000) and educational attainment level (percentage of the population with Associate’s degree or higher education) for the zip code of the parent’s residence. Similarly, we matched the zip code from the CDM database with the RUCA dataset to abstract the urbanicity of the parents (RUCA codes 1 and 1.1 are urban; RUCA codes 2, 3, and 3.1 are suburban; and 4–10 are rural (Li et al., 2019)). We created categorical variables for all these covariates.
Statistical Analyses
Descriptive statistics using Pearson’s chi-square test for categorical variables, and Generalized Estimation Equation (GEE) models, with correlated dichotomous responses (multiple parents per child) determined the association of parental depression and having a child with ASD. Additional logistic regression analyses using the ASD group cohort, determined the risk factors predicting parental depression.
GEE models provide a robust framework for analyzing population-average effects with correlated data common to family and longitudinal research because they account for the correlation of repeated measurements within an individual (Kleine-Budde et al., 2013). Our first binary outcome variable, the presence of depression, required a logit link function. For clustering at the family level, an exchangeable correlation structure was deemed appropriate (Homish et al., 2010). To assess our second and third outcomes, we used zero-inflated binomial regression, due to substantial positive skewness, excess zero values, and significant overdispersion with variance greater than the mean (Elhai et al., 2008).
A two-part regression model was used for analyzing the healthcare utilization costs. This model permits the investigator to distinguish factors that affect the propensity to use any services from factors that affect utilization volume once a person has entered the healthcare system (Diehr et al., 1999). The first part was a probit model for the probability of observing a zero versus a positive healthcare expenditure, and then the second part used a generalized linear model (GLM) to estimate the adjusted association of total healthcare costs conditional on a positive healthcare expenditure (Egede et al., 2016). The two-part model allows the user to leverage the capabilities of prediction and margins to calculate predictions and marginal effects and their standard errors from the combined first- and second-part models (Belotti & Deb, 2015).
All analyses were performed using STATA version 13.0 software (College Station, Texas; USA). The study is determined to qualify for exempt status according to 45 CFR 46.101(b) CATEGORY #4: Research, involving the collection or study of existing data, documents, records, pathological specimens, or diagnostic specimens, if these sources are publicly available or if the information is recorded by the investigator in such a manner that subjects cannot be identified directly or through identifiers linked to the subjects.
Results
There are 5,779 unique families of children diagnosed with ASD, and the Non-ASD group included 17,337 unique families matched using a 1:3 ratio. Before matching, there were no differences between the ASD and non-ASD cohorts based on child’s age and gender, parents’ age and gender, and family-level income. The total sample consisted of 23,316 unique families with 39,396 parents across both ASD-group and non-ASD group cohorts. Descriptive characteristics of these families are presented in Table 1. For families with ASD children 735 (7.3%) have at least one parent diagnosed with depression compared to 1,223 (4.1%) of families in the control group. Parents with an ASD child had almost twice the odds (OR 1.91, 95% CI 1.73 – 2.10) for depression after controlling for multiple children, parent enrollment status, and other household family characteristics (Table 2). Across all families, having both parents enrolled in insurance, rather than only a single parent enrolled, resulted in lower odds of depression (OR 0.85, 95% CI 0.75–0.95), while being female and living in a rural area, rather than urban, showed higher odds for depression (OR 3.5, 95% CI 2.39–5.34; OR 1.52, 95% CI 1.31–1.77 respectively).
Analyses of families with ASD children showed parents with multiple ASD children are 1.6 times at higher odds of being depressed (OR 1.6, 95% CI 1.18 – 2.13) than those with only 1 ASD child (Table 3). However, having multiple children had a protective impact on parental depression (OR 0.84, 95% CI 0.71 – 1.0). Mothers had two and a half times the odds of being depressed than fathers (OR 2.40, 95% CI 2.04 – 2.79). And, families with parents living in rural areas were almost twice more likely to be depressed than families of parents living in urban areas (OR 1.76, 95% CI 1.36 – 2.28).
Healthcare Utilization and Costs
Depressed parents without ASD children were observed to have lower length of stay utilization for depression treatment (IRR = 0.57, 95% CI 0.36–0.92) than the parents with ASD children; yet higher utilization in pharmacy prescriptions (IRR = 1.07, 95% CI 1.02–1.12) (Table 4). Regarding all-cause utilization, depressed parents in the non-ASD group were observed to have lower utilization in the length of stay (IRR = 1.52, 95% CI 1.19–1.95); facility outpatient (IRR = 1.10, 95% CI 1.03–1.17); professional office visits (IRR = 1.18, 95% CI 1.12–1.23); pharmacy prescription (IRR = 1.19, 95% CI 1.14–1.25).
Mean costs and adjusted incremental differences between depressed parents in the ASD group compared to the non-ASD group are presented in Table 5. The adjusted incremental effect is derived from the regression analysis which addresses the skewness in the utilization and cost data. Facility outpatient costs for the ASD group parents had an adjusted incremental cost difference in facility outpatient costs by $287 (p = 0.003). Adjusted incremental costs for depression-related pharmacy prescriptions and total costs were also slightly higher, but not highly significant, for the ASD group ($43, p = 0.074, $438, p = 0.078, respectively). All-cause mean costs per depressed parent for the ASD group were $15,460(SD = $33,084) compared to $12,858(SD = $34,077) for the depressed parent in the non-ASD group. The adjusted incremental effect was $778 for facility outpatient (p = 0.012), $548 for professional office visits (p = 0.01), $1,234 for pharmacy prescriptions (p = 0.002) and $2,050 for total costs (p = 0.067).
Discussion
Data from our study has shown that parents of children with ASD are associated with twice the risk of diagnosed depression compared to parents of children without ASD. Mothers of ASD children had 3.5 times of odds of depression compared to mothers with children without ASD. These findings are consistent with prior research (Cohrs & Leslie, 2017). Additionally, parents with ASD children living in a rural area had 1.5 times the odds of depression compared to those living in urban or suburban areas. Challenges with parental access to specialty healthcare in rural areas compared to urban and suburban areas would support our findings. Depression-related length of stay is higher in parents with an ASD child; however, no differences were found in other depression-related healthcare utilization. However, all-cause utilization for length of stay, professional office visits, outpatient visits and pharmacy were found to be higher for parents with an ASD child.
The mean annual cost of treatment of depression- and all-cause treatment (includes treatment costs for all diagnoses)is higher for ASD-parents across outpatient settings, pharmacy prescriptions, and total costs. Professional office visits were higher in all-cause costs only. Our observation of mean costs per parent for depression treatment services ($2,418) and all-cause treatment services ($15,460) is consistent with the earlier studies' findings. Amos et al. (2018) found the cost per person per year for non-treatment resistance major depressive disorder to be $2,109 for depression-related treatments and $17,261 for all-cause treatment services. Greenberg et al. (2015) reported treatment costs of major depressive disorder (MDD) as $2,366 per patient per year. The higher all-cause utilization and incremental costs suggests that the parents in the ASD group may prioritize their depression treatment lower than other healthcare resource needs in the family. However, further research is needed to better understand the drivers for the cost and utilization differentials between the two cohorts.. The impact of resource prioritization by parents in such potential situations or better understanding the changes in lifestyles are topics for further research.
Conclusion
This research has several strengths, such as using a large nationally representative sample, using clinical diagnosis to identify depression and ASD diagnoses as opposed to self-report, matching ASD-group and Non-ASD group on household characteristics, continuous enrollment, and exclusion of parents with depression before the study period. However, limitations worth noting include the inability to include parents who had depression but did not have a claim during the study period. Lack of individual socio-economic factors like education and income level for the parents. Similarly, children who had ASD but did not seek treatment during the lookback and study period were not captured in the study. The temporal relationship between the initial diagnoses of ASD (child) and depression (parent) was not determined with our dataset, as such causality cannot be determined. We only observed the association of ASD diagnosis in the child with the depression diagnosis in their respective parents. The study data does not include the Medicaid population and hence limits the generalizability of the findings.
Data from our research has shown that parents of children with ASD are associated with significantly higher risk of depression than parents without ASD. We observed that the odds of depression in mothers of ASD children are significantly higher. Similarly, fathers of children with ASD are also at higher risk for depression. The data has also shown that the odds of depression increase significantly if parents had more than one child with ASD. Similarly, the odds of depression in parents with ASD children increased if they were living in a rural area.
Our study suggests differences in incremental costs and utilization exists for depression treatments services and healthcare overall between the ASD and non-ASD cohorts. The strength of the results demonstrates the gap in the literature and the need for further research in this area. The cost burden for depression and ASD as separate mental health disorders has been well researched and understood. However, the impacts of having these two co-occurring chronic diseases and the financial burden on a family are poorly understood.
Based on these findings, support mechanisms for parents should be developed as soon as they receive an ASD diagnosis for their children. Depression among caregivers of young children is increasingly recognized as a devastating public health problem affecting caregivers and the children in their care (Ertel et al., 2011). Caregivers of children with ASD require services beyond the current healthcare system's services (Vohra et al., 2014). Policies and healthcare programs that provide mental health support, insurance benefits for the parents of children with ASD should be developed. Given the interdependencies and the co-occurring mental health conditions between the parents and children, newer policies and programs should include components that consider the family as an integrated unit.
References
Altiere, M. J., & Von Kluge, S. (2009). Family functioning and coping behaviors in parents of children with autism. Journal of Child and Family Studies, 18(1), 83.
Amos, T. B., Tandon, N., Lefebvre, P., Pilon, D., Kamstra, R. L., Pivneva, I., & Greenberg, P. E. (2018). Direct and indirect cost burden and change of employment status in treatment-resistant depression: A matched-cohort study using a US commercial claims database. The Journal of Clinical Psychiatry, 79(2). https://doi.org/10.4088/JCP.17m11725
Bastawrous, M. (2013). Caregiver burden—A critical discussion. International Journal of Nursing Studies, 50(3), 431–441.
Belotti, F., & Deb, P. (2015). TWOPM: Stata module to estimate two-part models.
Breslow, A. S., Tran, N. M., Lu, F. Q., Alpert, J. E., & Lê Cook, B. (2019). Depression treatment expenditures for adults in the USA: A systematic review. Current Psychiatry Reports, 21(10), 105.
Brody, D. J., Pratt, L. A., & Hughes, J. P. (2018). Prevalence of depression among adults aged 20 and over: United states, 2013–2016. NCHS Data Brief, (303)(303), 1–8.
Burke, J. P., Jain, A., Yang, W., Kelly, J. P., Kaiser, M., Becker, L., ... Newschaffer, C. J. (2014). Does a claims diagnosis of autism mean a true case? Autism: The International Journal of Research & Practice, 18(3), 321–330. https://doi.org/10.1177/1362361312467709
Callaghan, T., & Sylvester, S. (2019). Autism spectrum disorder, politics, and the generosity of insurance mandates in the united states. PLoS ONE, 14(5), 1–22. https://doi.org/10.1371/journal.pone.0217064
Candon, M. K., Barry, C. L., Marcus, S. C., Epstein, A. J., Kennedy-Hendricks, A., Xie, M., & Mandell, D. S. (2019). Insurance mandates and out-of-pocket spending for children with autism spectrum disorder. Pediatrics, 143(1), https://doi.org/10.1542/peds.2018-0654. Epub 2018 December 12
Chang, H., Chiou, C., & Chen, N. (2010). Impact of mental health and caregiver burden on family caregivers' physical health. Archives of Gerontology and Geriatrics, 50(3), 267–271.
Cohrs, A., & Leslie, D. (2017). Depression in parents of children diagnosed with autism spectrum disorder: A claims-based analysis. Journal of Autism & Developmental Disorders, 47(5), 1416–1422. https://doi.org/10.1007/s10803-017-3063-y
Collins, L. G., & Swartz, K. (2011). Caregiver care. American Family Physician, 83(11), 1309.
Croen, L. A., Najjar, D. V., Ray, G. T., Lotspeich, L., & Bernal, P. (2007). A comparison of health care utilization and costs of children with and without autism spectrum disorders in a large group-model health plan. Journal of the American Academy of Child & Adolescent Psychiatry, 46(4), 523.
Diehr, P., Yanez, D., Ash, A., Hornbrook, M., & Lin, D. (1999). Methods for analyzing health care utilization and costs. Annual Review of Public Health, 20(1), 125–144.
Egede, L. E., Bishu, K. G., Walker, R. J., & Dismuke, C. E. (2016). Impact of diagnosed depression on healthcare costs in adults with and without diabetes: United States, 2004–2011. Journal of Affective Disorders, 195, 119–126.
Elhai, J. D., Calhoun, P. S., & Ford, J. D. (2008). Statistical procedures for analyzing mental health services data. Psychiatry Research, 160(2), 129–136.
Epperson, C. N., Huang, M. Y., Cook, K., Gupta, D., Chawla, A., Greenberg, P. E., & Eldar-Lissai, A. (2020). Healthcare resource utilization and costs associated with postpartum depression among commercially insured households. Current Medical Research and Opinion, 36(10), 1707–1716. https://doi.org/10.1080/03007995.2020.1799772
Ertel, K. A., Rich-Edwards, J. W., & Koenen, K. C. (2011). Maternal depression in the united states: Nationally representative rates and risks. Journal of Women's Health (2002), 20(11), 1609–1617. https://doi.org/10.1089/jwh.2010.2657
Friedrich, M. (2017). Depression is the leading cause of disability around the world. JAMA, 317(15), 1517–1517.
Fiest, K. M., Jette, N., Quan, H., St Germaine-Smith, C., Metcalfe, A., Patten, S. B., & Beck, C. A. (2014). Systematic review and assessment of validated case definitions for depression in administrative data. BMC Psychiatry, 14, 289-014-0289-5. https://doi.org/10.1186/s12888-014-0289-5
Greenberg, P. E., Fournier, A. A., Sisitsky, T., Pike, C. T., & Kessler, R. C. (2015). The economic burden of adults with major depressive disorder in the United States (2005 and 2010). The Journal of Clinical Psychiatry, 76(2), 5356.
Homish, G. G., Edwards, E. P., Eiden, R. D., & Leonard, K. E. (2010). Analyzing family data: A GEE approach for substance use researchers. Addictive Behaviors, 35(6), 558–563.
Kleine-Budde, K., Müller, R., Kawohl, W., Bramesfeld, A., Moock, J., & Rössler, W. (2013). The cost of depression–a cost analysis from a large database. Journal of Affective Disorders, 147(1–3), 137–143.
Koyanagi, A., DeVylder, J. E., Stubbs, B., Carvalho, A. F., Veronese, N., Haro, J. M., & Santini, Z. I. (2018). Depression, sleep problems, and perceived stress among informal caregivers in 58 low-, middle-, and high-income countries: A cross-sectional analysis of community-based surveys. Journal of Psychiatric Research, 96, 115–123.
Lavelle, T. A., Weinstein, M. C., Newhouse, J. P., Munir, K., Kuhlthau, K. A., & Prosser, L. A. (2014). Economic burden of childhood autism spectrum disorders. Pediatrics, 133(3), e520-9. https://doi.org/10.1542/peds.2013-0763
Li, G., Andrews, H. F., Chihuri, S., Lang, B. H., Leu, C. S., Merle, D. P., ... & Hill, L. L. (2019). Prevalence of potentially inappropriate medication use in older drivers. BMC Geriatrics, 19(1), 1–8.
Li, Q., Li, Y., Liu, B., Chen, Q., Xing, X., Xu, G., & Yang, W. (2022). Prevalence of autism spectrum disorder among children and adolescents in the United States from 2019 to 2020. JAMA Pediatrics, 176(9), 943–945.
Luther, E. H., Canham, D. L., & Cureton, V. Y. (2005). Coping and social support for parents of children with autism. The Journal of School Nursing, 21(1), 40–47.
Stevenson, B. S., & Correa, V. I. (2019). Applied behavior analysis, students with autism, and the requirement to provide a free appropriate public education. Journal of Disability Policy Studies, 29(4), 206–215.
Vohra, R., Madhavan, S., Sambamoorthi, U., & St Peter, C. (2014). Access to services, quality of care, and family impact for children with autism, other developmental disabilities, and other mental health conditions. Autism: The International Journal of Research & Practice, 18(7), 815–826. https://doi.org/10.1177/1362361313512902
Weinberger, A., Gbedemah, M., Martinez, A., Nash, D., Galea, S., & Goodwin, R. (2018). Trends in depression prevalence in the USA from 2005 to 2015: Widening disparities in vulnerable groups. Psychological Medicine, 48(8), 1308–1315.
Author information
Authors and Affiliations
Contributions
Concept and design (SVK); acquisition of data (SVK, TMK); analysis and interpretation of data (SVK); drafting of the manuscript (SVK, RT); critical revision of the manuscript for important intellectual content (SVK, FLR, TMK, JMY, NTO, RT); statistical analysis (SVK); supervision (FLR).
Corresponding author
Ethics declarations
Conflict of Interest
All authors report no relationship or financial interest with any entity that would pose a conflict of interest with the subject matter. The authors have no financial or proprietary interests in any material discussed in this article.
Ethical Approval
This research involved secondary de-identified data and was deemed exempt by the University of Texas Health Science Center Houston IRB committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Karra, S.V., Krause, T.M., Yamal, JM. et al. Autism Spectrum Disorder and Parental Depression. J Dev Phys Disabil 36, 575–589 (2024). https://doi.org/10.1007/s10882-023-09924-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10882-023-09924-6