Abstract
Technology may help adolescents with chronic illnesses overcome barriers to accessing peer support, which has been associated with better quality of life and health outcomes. This review aimed to describe technology-based peer support interventions for adolescents with chronic illness following Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Of 3781 articles identified, 32 met inclusion criteria. The most common technologies were websites with discussion forums (n = 18), chat messaging (n = 9), and video conferencing (n = 7). Most studies (69%) focused on feasibility and had small sample sizes. Results support the feasibility and acceptability of these interventions. Results suggested positive effects on social support, but were mixed on isolation, quality of life, and disease self-management. There were too few adequately powered randomized controlled trials to determine efficacy of these interventions at this time. Future work should use rigorous methods to evaluate efficacy and account for rapid shifts in technology for adolescent communication.
Similar content being viewed by others
Introduction
The period of adolescence is marked by profound physical and mental growth and is recognized as formative years for identity development (Stangor & Walinga, 2010). As part of normal growth, adolescents develop independence from parents and form strong peer attachments as they develop autonomy (Christie & Viner, 2005). The World Health Organization has estimated that up to 15% of adolescents worldwide may have a chronic illness, and reported that for these teens, treatment regimens and disabilities related to chronic illness can impact the socialization process for adolescents (Michaud et al., 2007). Peer-to-peer support, which connects people with the same illness, has been shown to both improve disease management and quality of life outcomes among adults with chronic illnesses, as well as reach groups that other healthcare services fail to engage, such as those from low socioeconomic backgrounds, rural communities, and racial/ethnic minorities (Bennett et al., 2018; Dennis, 2003; Fisher et al., 2012; Sokol & Fisher, 2016; Warshaw et al., 2019). Peer mentoring and support can be highly useful to teens with chronic illness and can improve their social connectedness, disease self-management, adherence, and quality of life (Ahola Kohut et al., 2014; Merianos et al., 2015).
Although peer support can be helpful, individuals may face geographic or logistical obstacles in obtaining peer support from others with the same illness. Particularly in the context of the global pandemic, where many patient visits were converted to telehealth and previously established support groups and other meetings were either put on hold or converted to a virtual format, the use of technology to connect with peers may overcome many of these obstacles. Indeed, in recent nationwide surveys, 95% of teens report access to a smartphone or home computer, with 45% of teens reporting being on the Internet “almost constantly” (Anderson & Jiang, 2018). A systematic review showed that adults with chronic illness use online communities to rebuild their social networks and share knowledge (Kingod et al., 2016). A prior systematic review of peer support interventions for adolescents with chronic illness found that only three of eleven studies featured technology-based communication despite the prevalence of technology use by teens (Ahola Kohut et al., 2014).
Technology has rapidly become a form of communication and connection for adolescents since the last published review of peer support interventions. In particular, adolescents almost universally use social media for a variety of reasons, including to seek health information and disease- related advice, as well as to share their experiences and connect with others (Fergie et al., 2016; Patel et al., 2015; Villanti et al., 2017). Social media creates virtual communities that help develop relationships with peers, reduce feelings of isolation or loneliness, increase experiential knowledge sharing, and may foster feelings of belonging (Wilson & Stock, 2021). Youth with chronic illnesses use social media to seek and provide social, emotional, and experiential support (Patel et al., 2015).
There is growing evidence that suggests that the usage of technology in providing healthcare in pediatric populations is comparable to or better than in-person care in a variety of settings and can improve outcomes such as adherence (Badawy et al., 2017a, 2017b; Radovic & Badawy, 2020; Shah & Badawy, 2021). Therefore, this study aimed to systematically review and describe the literature on technology-based peer support interventions for adolescents with chronic illness. The specific research questions addressed were: (1) Which chronic conditions do technology-based peer support interventions target?; (2) What types of technology are used?; (3) What study designs and outcomes are implemented?; (4) Are the interventions feasible and acceptable?; and (5) If sufficient intervention outcome data exist, what is the efficacy of technology-based peer support for adolescents diagnosed with chronic illness?
Methods
Design
To address the research questions, the PubMed database was queried for studies meeting inclusion through 6/28/2020. Search terms were expanded from a prior review of peer support interventions (Ahola Kohut et al., 2014) and included terms related to “youth” or “adolescents” with “chronic illness” or specific diseases, as well as “peer support” and related terms. The search algorithm is in Supplementary File 1. Only published literature was reviewed; no other methods were employed to identify relevant studies such as contacting researchers. If an article identified was a secondary analysis, the reference list was scanned to identify the primary analysis and include if not already identified.
Study Selection
Inclusion criteria were: (1) written in the English language and published in a peer-reviewed journal; (2) the mean age of participants was in the adolescent age group, defined as ages 11–21 years old (based on guidelines from the American Academy of Pediatrics, Hardin & Hackell, 2017); (3) participants were previously diagnosed with a chronic medical condition (including but not limited to those listed in the second group of search terms); (4) must evaluate an intervention, using the National Institute of Health (2017) definition of intervention as “a manipulation of the subject or subject’s environment for the purpose of one of more health-related biomedical or behavioral processes and/or endpoints”; and (5) the intervention must involve technology-based peer support with communication between peers with the same chronic illness. Technologies included but were not limited to: cell phone calls, Skype, mobile applications, text messaging, forums, social media (including Facebook, Twitter, Instagram), web games, comment exchange. Multifaceted interventions that included a peer support component were allowed. Studies were excluded if they did not meet the criteria above, including studies focusing on the prevention of a chronic condition, studies with adolescents diagnosed with a psychiatric disorder, technology interventions that did not involve active communication from a peer (e.g., automated supportive texts or reminders), studies focusing on development and/or usability testing of a prototype, protocol papers, and systematic reviews. If there were multiple publications from a single study, only the primary analysis or most recent study was included.
Review Process
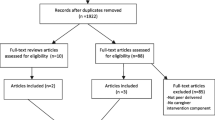
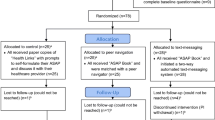
First, titles and abstracts were screened using the inclusion/exclusion criteria. Next, potential studies underwent a full text review. Two independent reviewers conducted all steps; any disagreements were discussed with a third reviewer for consensus on inclusion. The numbers of studies meeting criteria through each step of the review are reported using a PRISMA flow diagram (Moher et al., 2009).
One reviewer extracted study characteristics such as author, year of publication, study design, technology used, length of intervention, participant characteristics, and results. Finally, two reviewers independently rated the quality of each study using the Evidence Project risk of bias tool (Kennedy et al., 2019). This tool was selected because it assesses risk of bias across randomized and non-randomized studies. The tool includes eight items related to study design (i.e., whether participants are followed over time, whether a comparison group is included, whether pre/post intervention outcome data are included), participant representativeness (i.e., random assignment of participants to the intervention, random selection of participants for assessment, adequate follow-up rate of 80% or higher), and the equivalence of comparison groups (i.e., equivalence on baseline sociodemographic and baseline outcome measures). For each study, each item was rated as present, absent, not applicable, or not reported. Any discrepancies were resolved by a third reviewer.
Results
A total of 3780 articles were obtained from the search criteria and screened for inclusion. One article was added from the reference list of a secondary analysis for a total of 3781 records. After excluding studies that did not meet our inclusion criteria at the title and abstract level, the full texts of 114 studies were reviewed for inclusion. Of these studies, 32 studies met inclusion criteria. See Fig. 1 for the PRISMA flow diagram. Study characteristics and outcomes are detailed in Table 1. Papers are presented in alphabetical order, with detailed descriptions of the intervention, the type of technology used, whether the peer support component was a primary or supplemental aspect of the intervention, participant characteristics, primary and secondary outcomes, and results.
Populations
The average age of subjects ranged from 12.1 to 21 years old. The sample sizes ranged from 6 to 728, with a mean number of 84.7 subjects and median of 34. Only six studies (19%) had sample sizes greater than 100. Sixteen studies (50%) were conducted in the USA; five (16%) were conducted in Canada. Interventions targeted adolescents with a number of different chronic conditions. The condition most represented in these studies was Type 1 diabetes mellitus (T1DM; n = 12 studies). Five studies involved adolescents with cancer across the cancer survivorship trajectory (n = 5). Other conditions studied included: human immunodeficiency virus (HIV; n = 3), cystic fibrosis (n = 2), juvenile idiopathic arthritis (JIA; n = 2), solid organ transplant (n = 1), cardiac disease (n = 1), chronic pain (n = 1), any chronic illness (n = 1), severe obesity (n = 1), inflammatory bowel disease (IBD; n = 1), lupus (n = 1), asthma and allergies (n = 1).
Types of Technology
There were myriad technologies used including Facebook groups, chat messaging, Instagram, websites with discussion forums, mobile applications (“apps”), online environments, and online video conferencing interfaces. Types of communication included synchronous (n = 11 studies), asynchronous (n = 15 studies), or both (n = 6 studies). Discussion forums, where group members can post to all members of the group, were the most common feature utilized within these interventions (n = 18 studies). Within these 18 studies, Facebook was used in six studies and the remaining studies used other types of asynchronous message forums. In general, these groups were private for study participants rather than being open to the public.
Nine studies used chat messaging, including text messaging. Chat was often one of several features of an intervention. Videoconferencing was included in 7 studies, with use of Skype (n = 3), Zoom (n = 1), Vidyo (n = 1), and other unspecified platforms (n = 2). Email messaging was included in two interventions. Three studies created mobile phone applications.
Authors also commented on the involvement of facilitators who monitored and prompted conversations. There was variability in who the facilitators were if they were used. Health care providers were the facilitators in several of the studies (Gonzalez-Morkos et al., 2014; Griffiths et al., 2015; Letourneau et al., 2012; Troncone et al., 2019), with one study also using peer mentors as facilitators (Letourneau et al., 2012).
Study Designs and Outcomes
All studies were published within the past ten years, except for one study published in 2001 (Johnson et al.). Twenty of the studies were published in the past 5 years. The majority of the studies were single arm studies (n = 22 feasibility studies; n = 1 content analysis). There were 12 randomized two-arm trials and two unique study designs. The study described by Johnson et al. (2001) used a modified waitlist control design. The study described by Gonzalez-Morkos et al. (2014) utilized a single arm design, but one subdivision of the participants attended a live, in-person intervention, while another subdivision participated via webcast. This was due to the H1N1 pandemic, in which certain patients were not able to attend the live session safely due to concern for infection (Gonzalez-Morkos et al., 2014).
The primary outcome for most studies was feasibility (n = 22). Other outcomes include A1C (Boogerd et al., 2014; Grey et al., 2013; Iafusco et al., 2011; Whittemore et al., 2010, 2016), quality of life (Ammerlaan et al., 2017; Grey et al., 2013; Iafusco et al., 2011; Newton & Ashley, 2013; Plevinsky & Greenley, 2014; Whittemore et al., 2010, 2016;), disease knowledge (Boogerd et al., 2014; Dulli et al., 2020; Johnson et al., 2001), social support (Dulli et al., 2020; Letourneau et al., 2012; Nicholas et al., 2012), self-management (Ammerlaan et al., 2017; Newton & Ashley, 2013), medication initiation or adherence (Dulli et al., 2020; Hacking et al., 2019; Scalzi et al., 2018), retention in care (Dulli et al., 2020), stress and coping (Freedenberg et al., 2017; Whittemore et al., 2010), anxiety and depression (Freedenberg et al., 2017), disease activity (Ammerlaan et al., 2017), viral load suppression (Hacking et al., 2019), retention in healthcare (Ammerlaan et al., 2017; Dulli et al., 2020), engagement with healthcare (Hacking et al., 2019), and absenteeism (Ammerlaan et al., 2017).
Feasibility and Acceptability
All of the studies found interventions to be feasible and acceptable to participants. The majority of studies used a mixed methods approach, in that data were obtained about how frequently the technology was used and followed up with qualitative interviews. Participants reported positive engagement with the intervention in most studies (n = 22) (Ammerlaan et al., 2017; Boogerd et al., 2014; Cafazzo et al., 2012; Chadi et al., 2018; Donovan et al., 2019; Dulli et al., 2018; Francis et al., 2020; Mendoza et al., 2017; Prout Parks et al., 2018). In one study, subjects that had previously performed the intervention in a live setting were unsatisfied when it was changed to delivery via technology, but participants who first participated in the technology intervention found it satisfactory (Gonzalez-Morkos et al., 2014).
Participant engagement data were variable across studies and was measured differently depending on type of technology (e.g., number of messages posted, number of sessions completed). Studies found anywhere from 50 to 75% of participants met participation milestones such as posting in sessions or completing videoconferences (Dulli et al., 2018; Sansom‐Daly et al., 2019; Stinson et al., 2016; Yi-Frazier et al., 2015). One study found that the number of messages exchanged doubled with the use of a facilitator (Griffiths et al., 2015). Overall, adolescents found the technology easy to use (Francis et al., 2020; Johnson et al., 2001; Raymond et al., 2016).
Efficacy
While most studies (n = 22) concluded that these types of interventions were feasible, several also evaluated intervention effects on mental and physical health outcomes. Thirteen interventions positively impacted social support, social network, or isolation (Ammerlaan et al., 2017; Bers et al., 2010; Chadi et al., 2018; Donovan et al., 2019; Dulli et al., 2020; Freedenberg et al., 2017; Gonzalez-Morkos et al., 2014; Griffiths et al., 2015; Johnson et al., 2001; Letourneau et al., 2012; Nicholas et al., 2012; Plevinsky & Greenley, 2014; Raymond et al., 2016). While four of these studies identified statistically significant improvement on measures of social support (Johnson et al., 2001; Letourneau et al., 2012; Nicholas et al., 2012; Plevinsky & Greenley, 2014), at least seven of the studies reported improved social support as a qualitative outcome from interview data. Two studies demonstrated no significant change in social support measures (Donovan et al., 2019; Dulli et al., 2020). Effect sizes were not reported or small (e.g., Cohen’s d = .2 to .3).
Other commonly reported outcomes were HbA1C (in studies involving adolescents with T1DM), and quality of life (in studies of patients with T1DM, IBD, and cancer). For studies evaluating HbA1C, three studies showed improvement in levels compared to baseline (Boogerd et al., 2014; Iafusco et al., 2011; Petrovski & Zivkovic, 2019), while three other studies showed no change (Grey et al., 2013; Whittemore et al., 2010, 2016). Similarly, for studies evaluating quality of life, three showed improvements (Boogerd et al., 2014; Iafusco et al., 2011; Plevinsky & Greenley, 2014), and four showed no change from baseline (Mendoza et al., 2017; Newton & Ashley, 2013; Whittemore et al., 2010, 2016;). One study found a significant decrease in illness-related stress in patients with cardiac disease (Freedenberg et al., 2017).
Other studies focused on disease self-management. Among studies that evaluated self-management and self-efficacy as an outcome, half of the studies demonstrated improvement (Ahola Kohut et al., 2016; Grey et al., 2013; Stinson et al., 2016), while the other half demonstrated no change (Ammerlaan et al., 2017; Boogerd et al., 2014; Newton & Ashley, 2013). Studies evaluating changes in disease knowledge found no significant differences in disease knowledge in patients with CF (Johnson et al., 2001) and in patients with HIV (Dulli et al., 2020). Three studies evaluated continued engagement with health care facilities and found no difference from baseline (Dulli et al., 2020; Hacking et al., 2019; Prout Parks et al., 2018).
Quality Review
As demonstrated in Table 2, there were several potential biases present in the studies reviewed. Although most studies (n = 19 of 32) had a control or comparison group, four of those 19 did not randomly assign participants to the groups or did not report about this aspect. Within studies that had a comparison group, only three studies reported that the comparison groups were equivalent on both sociodemographic and outcomes at baseline; the remaining were not reported or not equivalent and therefore failed to control for confounders. None of the studies randomly selected participants for assessment, as most solely recruited convenience samples from clinic, suggesting potential for selection bias and limiting the generalizability of these studies. Only thirteen studies demonstrated a follow-up rate of 80% or more, further limiting the generalizability of these studies.
Discussion
Given the omnipresence of technology in modern adolescents’ daily lives (Anderson & Jiang, 2018) and its potential to overcome access barriers to reach social support, this review examined the current landscape of technology-based peer support interventions among teens with chronic disease, including whether such interventions are acceptable and useful for adolescents. The total number of studies meeting inclusion criteria was 32, which represents an overall dearth of studies relative to the scope of the search. Almost all of the studies were published in the past ten years, coinciding with the surge of social media and daily technology use within society more broadly, as well as researcher interest in harnessing mobile technologies for health (Faiola et al., 2019; Perrin, 2015).
The studies used a variety of technologies to facilitate peer support. Discussion boards utilizing asynchronous communication were overwhelmingly popular. Facebook groups also utilize asynchronous messaging, and, in addition, offer an interface that is readily used in daily life. Other studies used video conferencing or developed novel mobile applications. Interestingly, all of the studies using video conferencing were published in 2016 or later, suggesting a more recent trend toward video conferencing. Despite extremely high use of mobile phones by adolescents (Anderson & Jiang, 2018), very few studies relied on mobile technology or text messaging. Likewise, as of 2018, YouTube, Instagram, and Snapchat were the most popular online tools used by teens, though only one included study involved Instagram (Yi-Frazier et al., 2015). Thus, variability in engagement seen within the different studies may be due in part to inconsistency between the types of technology that teens use for their own social connection and what is being used in research studies. Additionally, facilitator differences, such as whether they were known to the subjects as part of the healthcare team versus a peer facilitator, as well as the degree to which facilitators prompted users, likely influenced the extent of participation and candor of exchange between participants. It is important that researchers continue to define and report on the characteristics and involvement of facilitators such that more thorough and repeatable analyses can be performed on their utility.
The state of the literature on peer support for chronic illness reflects mostly feasibility and acceptability studies, with 22 of the 32 studies reviewed being feasibility studies. This is consistent with a prior review of peer mentoring studies in adolescents with chronic disease that was not specific to technology (Ahola Kohut et al., 2014). The large proportion of feasibility studies underscores the early phase of development for these interventions, in part due to the rapidly evolving field of eHealth.
Though efficacy studies were limited, half were conducted with youth with T1DM. However, outcomes varied widely across studies and there is too little data to make conclusions regarding efficacy. Additionally, the overall rigor of most studies was low to moderate, with a minority of studies being randomized studies (n = 12), possible selection bias, and difficulties with retention. Of the studies that measured quantitatively measured medical outcomes (n = 10), 6 studies had a large study size (> 72 participants) and 2 studies showed statistically significant results. Nonetheless, general trends in the data were apparent. Importantly, the general satisfaction of participants across studies was notable, suggesting adolescents find these types of interventions acceptable. Indeed, several studies indicated that participants contacted each other outside of the study (Griffiths et al., 2015; Johnson et al., 2001; Raymond et al., 2016). This presumed openness to continuing a relationship outside of the technology intervention suggests that participants are engaging in meaningful relationships.
Strengths of the current review include the focus on technology-based interventions, which is timely given the increased reliance on technology among youth and in healthcare. Additionally, we followed the PRISMA guidelines to conduct a rigorous review, used extensive search terms to identify relevant studies, and had two independent reviewers conduct each step of screening.
The current review was limited in that it included only published data in English language from a single database, which may introduce publication bias, as null or negative findings may be less likely to be published, and may have missed relevant articles published in other databases. However, PubMed/MEDLINE is the largest, most relevant database for this search focusing on the intersection of chronic illness and behavioral interventions. Limitations of the literature more broadly include the wide variability in behavioral targets, validated measures, and outcomes across studies, making it difficult to compare across studies and draw conclusions. Most study designs reflect early development and feasibility work (n = 22), with a focus on mixed methods and qualitative results. The targeted age range for studies varied; one study found non-significant differences in the use of different features by age (e.g., older participants used the medication reminders more, while younger participants like the virtual computerized buddy check-in; Francis et al., 2020). No study evaluated whether response to the intervention differed as a function of age or developmental maturity. Future research should consider these factors in the development and evaluation of peer support interventions. There was a paucity of quantitative health outcome endpoints, making it difficult to synthesize outcome data at this time. Additionally, nearly one third of the studies identified in the current literature were focused on patients with T1DM. As the disease experiences and needs of patients vary greatly across disease populations, the generalizability of these results may be limited due to many studies with one population.
Together, these studies demonstrate feasibility and acceptability of using technology to facilitate peer support among adolescents with chronic disease. These results are consistent with other literature demonstrating the feasibility, acceptability, and beneficial effects of telehealth and other digital interventions on quality of life, symptom management, medication adherence, and satisfaction outcomes among children and adolescents (Radovic & Badawy, 2020; Shah & Badawy, 2021). There is a need for more rigorous evaluation of efficacy, including adequately powered randomized controlled trials, prior to recommending widespread clinical application of these interventions. Related topics within the field, such as telemental health for adolescents and electronic mentoring for youth with disabilities, demonstrate similar limitations in the number of high quality randomized control trials performed (Lau et al., 2021; Lindsay et al, 2018). Peer support in adults with diabetes has been rigorously studied using randomized controlled trials, which allow for efficacy study; this should be looked to as a goal for the field (Qi et al., 2015). Future studies should specify the behavioral targets of each intervention and the outcomes expected to change. Studies that use validated scoring systems for outcomes, which are clear and reproducible, should be modeled after (Whittemore et al., 2016). Studies demonstrating specific mediators of change are also notable (Jaser et al., 2013). Further, there is a lack of economic data to support the use digital health interventions; future studies should include comprehensive economic evaluations of digital interventions (Badawy & Kuhns, 2016; Iribarren et al., 2017). Finally, there was significant variability in the types of medical and patient-reported outcomes in the studies identified in this review, with notable gaps in critical outcomes like suicide prevention. While some studies show promise in using technology to decrease suicidal ideation and attempts in adolescents, more research is needed on the usage of peer support in these interventions (Forte et al., 2021).
Given the rapid adoption of telehealth and virtual communication due to the COVID-19 pandemic, there will likely be greater interest in and research involving virtual peer support interventions for adolescents with chronic disease. The COVID-19 pandemic has brought psychosocial challenges for youth with chronic disease, including reduced physical and psychosocial support from peers and healthcare providers, which may be addressed through digital support (Serlachius et al., 2020). The pandemic rapidly increased the use of telehealth and other digital interventions in pediatric care (Badawy & Radovic 2020). More research is needed to understand the cost-effectiveness of telemedicine and other digital health approaches, as well as their impact on quality of care (Badawy & Radovic 2020).
A major challenge for future research and clinical applications of digital interventions is how rapidly technology and the preferences of adolescents can change. The results of the intervention by Gonzalez-Morkos et al. (2014) showed that changing an intervention from in-person to telehealth due to the H1N1 influenza epidemic in 2010 resulted in lower satisfaction among those who changed to virtual versus those had started with a virtual intervention only. This underscores the need for user-centered design and working with adolescent “end users” to “codesign” an intervention to meet their needs and expectations (Elsbernd et al., 2018). Involving patients in the development process is critical to their engagement with the digital health platform (Badawy et al., 2017b). Engagement can be conceptualized as both a subjective experience in interacting with the technology and as usage behaviors (Perski et al., 2017); it is important to seek the input of adolescents early in the process of development to ensure short- and long-term engagement with the tool (Badawy et al., 2016; Badawy et al., 2017a, 2017b). It will also be important to frequently re-evaluate the state of the literature to remain up to date. Ongoing work is needed to evaluate the usefulness of rapidly changing technologies and identify who benefits most from different interventions.
Conclusion
The state of the literature regarding technology-based peer support interventions for adolescents with chronic disease is currently in an early phase, with overall low quality of study designs. However, the growing number of interventions being evaluated and the consistently positive feasibility data point to the promise of these interventions. This review identified websites with discussion forums as the most commonly used technology, followed by chat messaging and then videoconferencing. Early efficacy data suggest social support is improved by these interventions, but future studies of adequately powered randomized control trials with validated outcome measures are needed. Finally, the COVID-19 pandemic underscores the importance of evaluating virtual interventions for adolescents with chronic disease to support patients no matter their geographic location.
Data Availability
All data relevant to the study are included in the article.
Code Availability
N/A.
References
Ahola Kohut, S., Stinson, J., van Wyk, M., et al. (2014). Systematic review of peer support interventions for adolescents with chronic illness. International Journal of Child Adolescent Health, 7, 183–197.
Ahola Kohut, S., Stinson, J. N., Ruskin, D., et al. (2016). iPeer2Peer program: A pilot feasibility study in adolescents with chronic pain. Pain, 157, 1146–1155.
Ammerlaan, J., van Os-Medendorp, H., de Boer-Nijhof, N., et al. (2017). Short term effectiveness and experiences of a peer guided web-based self-management intervention for young adults with juvenile idiopathic arthritis. Pediatric Rheumatology, 15(1), 1–13.
Anderson, M., & Jiang, J. (2018). Teens, Social Media & Technology. Retrieved from https://www.pewresearch.org/internet/2018/05/31/teens-social-media-technology-2018/.
Badawy, S. M., Barrera, L., Sinno, M. G., Kaviany, S., O’Dwyer, L. C., & Kuhns, L. M. (2017a). Text messaging and mobile phone apps as interventions to improve adherence in adolescents with chronic health conditions: A systematic review. JMIR mHealth and uHealth, 5(5), e66.
Badawy, S. M., & Radovic, A. (2020). Digital approaches to remote pediatric health care delivery during the COVID-19 pandemic: Existing evidence and a call for further research. JMIR Pediatrics and Parenting, 3(1), e20049.
Badawy, S. M., Thompson, A. A., & Kuhns, L. M. (2017b). Medication adherence and technology-based interventions for adolescents with chronic health conditions: A few key considerations. JMIR mHealth and uHealth, 5(12), e202.
Badawy, S. M., & Kuhns, L. M. (2016). Economic evaluation of text-messaging and smartphone-based interventions to improve medication adherence in adolescents with chronic health conditions: A systematic seview. JMIR mHealth and uHealth, 4(4), e121.
Badawy, S. M., Thompson, A. A., & Liem, R. I. (2016). Technology access and smartphone app preferences for medication adherence in adolescents and young adults with sickle cell disease. Pediatric Blood & Cancer, 63(5), 848–852.
Bennett, P. N., St. Clair Russell, J., Atwal, J., et al. (2018). Patient-to-patient peer mentor support in dialysis: Improving the patient experience. Seminars in Dialysis, 31, 455–461.
Bers, M. U., Beals, L. M., Chau, C., et al. (2010). Use of a virtual community as a psychosocial support system in pediatric transplantation. Pediatric Transplantation, 14, 261–267.
Boogerd, E. A., Noordam, C., Kremer, J. A. M., et al. (2014). Teaming up: Feasibility of an online treatment environment for adolescents with type 1 diabetes. Pediatric Diabetes, 15, 394–402.
Cafazzo, J. A., Casselman, M., Hamming, N., et al. (2012). Design of an mHealth app for the self-management of adolescent type 1 diabetes: A pilot study. Journal of Medical Internet Research, 14, e70.
Chadi, N., Weisbaum, E., Malboeuf-Hurtubise, C., et al. (2018). Can the Mindful Awareness and Resilience Skills for Adolescents (MARS-A) Program be provided online? Voices from the youth. Children, 5(9), 115.
Christie, D., & Viner, R. (2005). ABC of adolescence: Adolescent development. British Medical Journal, 330, 301–304.
Dennis, C.-L. (2003). Peer support within a health care context: A concept analysis. International Journal of Nursing Studies, 40, 321–332.
Donovan, E., Martin, S. R., Seidman, L. C., et al. (2019). A mobile-based mindfulness and social support program for adolescents and young adults with sarcoma: Development and pilot testing. JMIR mHealth and uHealth, 7, e10921.
Dulli, L., Ridgeway, K., Packer, C., et al. (2018). An online support group intervention for adolescents living with HIV in Nigeria: A pre-post test study. JMIR Public Health and Surveillance, 4, e12397.
Dulli, L., Ridgeway, K., Packer, C., et al. (2020). A social media-based support group for youth living with HIV in Nigeria (SMART Connections): Randomized controlled trial. Journal of Medical Internet Research, 22, e18343.
Elsbernd, A. B., Hjerming, M., Visler, C., et al. (2018). Using cocreation in the process of designing a smartphone app for adolescents and young adults with cancer: Prototype development study. JMIR Formative Research, 2(2), e9842.
Faiola, A., Papautsky, E. L., & Isola, M. (2019). Empowering the aging with mobile health: A mHealth framework for supporting sustainable healthy lifestyle behavior. Current Problems in Cardiology, 44, 232–266.
Fergie, G., Hilton, S., & Hunt, K. (2016). Young adults’ experiences of seeking online information about diabetes and mental health in the age of social media. Health Expectations : An International Journal of Public Participation in Health Care and Health Policy, 19(6), 1324–1335.
Fisher, E. B., Boothroyd, R. I., Coufal, M. M., et al. (2012). Peer support for self-management of diabetes improved outcomes in international settings. Health Affairs, 31, 130–139.
Forte, A., Sarli, G., Polidori, L., Lester, D., & Pompili, M. (2021). The role of new technologies to prevent suicde in adolescence: A systematic review of the literature. Medicina, 57(109), 1–13.
Francis, J., Cross, D., Schultz, A., et al. (2020). Developing a smartphone application to support social connectedness and wellbeing in young people with cystic fibrosis. Journal of Cystic Fibrosis, 19, 277–283.
Freedenberg, V. A., Hinds, P. S., & Friedmann, E. (2017). Mindfulness-based stress reduction and group support decrease stress in adolescents with cardiac diagnoses: A randomized two-group study. Pediatric Cardiology, 38, 1415–1425.
Gonzalez-Morkos, B., Zavala, O., Malogolowkin, M., et al. (2014). The teen impact experience: A webcast pilot project for teens with cancer and blood diseases. Journal of Pediatric Oncology Nursing, 31, 272–276.
Grey, M., Whittemore, R., Jeon, S., et al. (2013). Internet psycho-education programs improve outcomes in youth with type 1 diabetes. Diabetes Care, 36, 2475–2482.
Griffiths, C., Panteli, N., Brunton, D., et al. (2015). Designing and evaluating the acceptability of Realshare: An online support community for teenagers and young adults with cancer. Journal of Health Psychology, 20, 1589–1601.
Hacking, D., Mgengwana-Mbakaza, Z., Cassidy, T., et al. (2019). Peer mentorship via mobile phones for newly diagnosed HIV-positive youths in clinic care in Khayelitsha, South Africa: Mixed methods study. Journal of Medical Internet Research, 21, e14012.
Hardin, A. P., & Hackell, J. M. (2017) Age limit of pediatrics. American Academy of Pediatrics 140.
Iafusco, D., Galderisi, A., Nocerino, I., et al. (2011). Chat line for adolescents with type 1 diabetes: A useful tool to improve coping with diabetes: A 2-year follow-up study. Diabetes Technology & Therapeutics, 13, 551–555.
Iribarren, S. J., Cato, K., Falzon, L., & Stone, P. W. (2017). What is the economic evidence for mHealth? A systematic review of economic evaluations of mHealth solutions. PLoS ONE, 12(2), e0170581.
Johnson, K. B., Ravert, R. D., & Everton, A. (2001). Hopkins Teen Central: Assessment of an internet-based support system for children with cystic fibrosis. Pediatrics, 107, E24.
Kennedy, C. E., Fonner, V. A., Armstrong, K. A., et al. (2019). The Evidence Project risk of bias tool: Assessing study rigor for both randomized and non-randomized intervention studies. Systematic Reviews, 8(1), 3.
Kingod, N., Cleal, B., Wahlberg, A., et al. (2016). Online peer-to-peer communities in the daily lives of people with chronic illness. Qualitative Health Research, 27, 89–99.
Lau, N., Colt, S. F., Waldbaum, S., O’Daffer, A., Fladeboe, K., Yi-Frazier, J. P., McCauley, E., & Rosenberg, A. R. (2021). Telemental health for youth with chronic illnesses: Systematic review. JMIR Mental Health, 8(8), e30098.
Letourneau, N., Stewart, M., Masuda, J. R., et al. (2012). Impact of online support for youth with asthma and allergies: Pilot study. Journal of Pediatric Nursing, 27, 65–73.
Lindsay, S., Kolne, K., & Cagliostro, E. (2018). Electronic mentoring programs and interventions for children and youth with disabilities: Systematic review. JMIR Pediatrics and Parenting, 1(2), e11679.
Mendoza, J. A., Baker, K. S., Moreno, M. A., et al. (2017). A Fitbit and Facebook mHealth intervention for promoting physical activity among adolescent and young adult childhood cancer survivors: A pilot study. Pediatric Blood & Cancer, 64, e26660.
Merianos, A. L., King, K. A., Vidourek, R. A., et al. (2015). Mentoring and peer-led interventions to improve quality of life outcomes among adolescents with chronic illnesses. Applied Research in Quality of Life, 11, 1009–1023.
Michaud, P.-A., Suris, J.-C., & Viner, R. (2007). The adolescent with a chronic condition: Epidemiology, developmental issues and health care provision. World Health Organization.
Moher, D., Liberati, A., Tetzlaff, J., et al. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Annals of Internal Medicine, 151, 264–270.
National Institutes of Health. (2017). NIH clinical trail definition. Retrieved from https://grants.nih.gov/grants/policy/faq_clinical_trial_definition.htm#5243.
Newton, K. T., & Ashley, A. (2013). Pilot study of a web-based intervention for adolescents with type 1 diabetes. Journal of Telemedicine and Telecare, 19, 443–449.
Nicholas, D. B., Fellner, K. D., Frank, M., et al. (2012). Evaluation of an online education and support intervention for adolescents with diabetes. Social Work in Health Care, 51, 815–827.
Patel, R., Chang, T., Greysen, S. R., & Chopra, V. (2015). Social media use in chronic disease: A systematic review and novel taxonomy. The American Journal of Medicine, 128(12), 1335–1350.
Perrin A. (2015). Social media usage: 2005–2015. Pew Research Center. Retrieved from http://www.pewinternet.org/2015/10/08/2015/Social-Networking-Usage-2005-2015/.
Perski, O., Blandford, A., West, R., & Michie, S. (2017). Conceptualising engagement with digital behaviour change interventions: A systematic review using principles from critical interpretive synthesis. Translational Behavioral Medicine, 7(2), 254–267.
Petrovski, G. M., & Zivkovic, M. M. (2019). Are we ready to treat our diabetes patients using social media? Yes, we are. Journal of Diabetes Science and Technology, 13, 171–175.
Plevinsky, J. M., & Greenley, R. N. (2014). Exploring health-related quality of life and social functioning in adolescents with inflammatory bowel diseases after attending camp oasis and participating in a Facebook group. Inflammatory Bowel Diseases, 20, 1611–1617.
Prout Parks, E., Moore, R. H., Li, Z., et al. (2018). Assessing the feasibility of a social media to promote weight management engagement in adolescents with severe obesity: Pilot study. JMIR Research Protocols, 7, e52.
Qi, L., Liu, Q., Qi, X., Wu, N., Tang, W., & Xiong, H. (2015). Effectiveness of peer support for improving glycaemic control in patients with type 2 diabetes: A meta-analysis of randomized controlled trials. BMC Public Health, 15, 471.
Radovic, A., & Badawy, S. M. (2020). Technology use for adolescent health and wellness. Pediatrics, 145(Suppl 2), S186–S194.
Raymond, J. K., Berget, C. L., Driscoll, K. A., et al. (2016). CoYoT1 clinic: Innovative telemedicine care model for young adults with Type 1 diabetes. Diabetes Technology & Therapeutics, 18, 385–390.
Sanson-Daly, U. M., Wakefield, C. E., Bryant, R. A., et al. (2019). Feasibility, acceptability, and safety of the Recapture Life videoconferencing intervention for adolescent and young adult cancer survivors. Psycho-Oncology, 28, 284–292.
Scalzi, L. V., Hollenbeak, C. S., Mascuilli, E., et al. (2018). Improvement of medication adherence in adolescents and young adults with SLE using web-based education with and without a social media intervention, a pilot study. Pediatric Rheumatology, 16(1), 18.
Serlachius, A., Badawy, S. M., & Thabrew, H. (2020). Psychosocial challenges and opportunities for youth with chronic health conditions during the COVID-19 pandemic. JMIR Pediatrics and Parenting, 3(2), e23057.
Shah, A. C., & Badawy, S. M. (2021). Telemedicine in pediatrics: Systematic review of randomized controlled trials. JMIR Pediatric Parent., 4(1), e22696.
Sokol, R. B., & Fisher, E. P. (2016). Peer support for the hardly reached: A systematic review. American Journal of Public Health, 106(7), e1–e8.
Stangor, C., & Walinga, J. (2010) Introduction to psychology. 1st Canadian Edition ed. Victoria BCcampus, BC Open Textbook Project.
Stinson, J., Ahola Kohut, S., Forgeron, P., et al. (2016). The iPeer2Peer Program: A pilot randomized controlled trial in adolescents with Juvenile Idiopathic Arthritis. Pediatric Rheumatology, 14(1), 1–10.
Troncone, A., Cascella, C., Chianese, A., et al. (2019). Psychological support for adolescents with type 1 diabetes provided by adolescents with type 1 diabetes: The chat line experience. Pediatric Diabetes, 20(6), 800–810.
Villanti, A. C., Johnson, A. L., Ilakkuvan, V., Jacobs, M. A., Graham, A. L., & Rath, J. M. (2017). Social media use and access to digital technology in US young adults in 2016. Journal of Medical Internet Research, 19(6), e196.
Warshaw, H., Hodgson, L., Heyman, M., et al. (2019). The role and value of ongoing and peer support in diabetes care and education. The Diabetes Educator, 45, 569–579.
Whittemore, R., Liberti, L. S., Jeon, S., et al. (2016). Efficacy and implementation of an Internet psychoeducational program for teens with type 1 diabetes. Pediatric Diabetes, 17, 567–575.
Whittemore, R., Grey, M., Lindemann, E., et al. (2010). Development of an internet coping skills training program for teenagers with type 1 diabetes. CIN: Computers Informatics, Nursing, 28, 103–111.
Wilson, C., & Stock, J. (2021). “Social media comes with good and bad sides, doesn’t it?” A balancing act of the benefits and risks of social media use by young adults with long-term conditions. Health, 25(5), 515–534.
Yi-Frazier, J. P., Cochrane, K., Mitrovich, C., et al. (2015). Using instagram as a modified application of photovoice for storytelling and sharing in adolescents with type 1 diabetes. Qualitative Health Research, 25, 1372–1382.
Funding
This work was supported in part by the National Cancer Institute of the National Institutes of Health under Award number R21CA222936. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
Conceptualization: PB, KD; Literature Search/Data Abstraction: PB, AV, SP, QR; Writing – original draft: PB, KD; Writing—revision and final review: all authors.
Corresponding author
Ethics declarations
Conflict of interest
Patricia Berkanish, Samuel Pan, Adrienne Viola, Quinn Rademaker and Katie A. Devine declare that they have no conflict of interest.
Ethical Approval
N/A.
Consent to Participate
N/A.
Consent for Publication
N/A.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Berkanish, P., Pan, S., Viola, A. et al. Technology-Based Peer Support Interventions for Adolescents with Chronic Illness: A Systematic Review. J Clin Psychol Med Settings 29, 911–942 (2022). https://doi.org/10.1007/s10880-022-09853-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10880-022-09853-0