Abstract
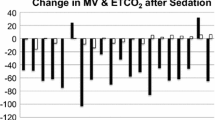
Endoscopic procedures performed under conscious sedation require careful monitoring of respiratory status to prevent adverse outcomes. This study utilizes a non-invasive respiratory volume monitor (RVM) that provides continuous real-time measurements of minute ventilation (MV), tidal volume and respiratory rate (RR) to assess the adequacy of ventilation during endoscopy. Digital respiratory traces were collected from 51 patients undergoing upper endoscopy with propofol sedation using an impedance-based RVM. Baseline MV for each patient was derived from a 30 s period of quiet breathing prior to sedation (MVBASELINE). Capnography data were also collected. Because RR from capnography was frequently unavailable, the RVM RR’s were used for analysis. RR rate values were compared the MV measurements and sensitivity and specificity of RR to predict inadequate ventilation (MV <40 % MVBASELINE) were calculated. Initial analysis revealed that there is a weak correlation between an MV measurement and its corresponding RR measurement (r = 0.05). If MV is an actual indictor of respiratory performance, using RR as a proxy is grossly inadequate. Simulating a variety of RR alarm conditions [4–8 breaths/min (bpm)] showed that a substantial fraction of low MV measurements (MV <40 % MVBASELINE) went undetected (at 8 bpm, >70 % low MV measurements were missed; at 6 bpm, >82 % were missed; and at 4 bpm, >90 % were missed). A cut-off of 6 bpm had a sensitivity of only 18.2 %; while <40 % of all RR alarms would have coincided with a low MV (39.4 % PPV). Low RR measurements alone do not reflect episodes of low MV and are not sufficient for accurate assessment of respiratory status. RVM provides a new way to collect MV measurements which provide more comprehensive data than RR alone. Further work is ongoing to evaluate the use of MV data during procedural sedation.




Similar content being viewed by others
References
Al-Awabdy B, Wilcox CM. Use of anesthesia on the rise in gastrointestinal endoscopy. World J Gastrointest Endosc. 2013;5(1):1–5.
Downs JB. Prevention of hypoxemia: the simple, logical, but incorrect solution. J Clin Anesth. 1994;6:180–1.
Downs JB. Has oxygen administration delayed appropriate respiratory care? Fallacies regarding oxygen therapy. Respir Care. 2003;48(6):611–20.
Jabre P, Jacob L, Auger H, Jaulin C, Monribot M, Aurore A, Margenet A, Marty J, Combes X. Capnography monitoring in nonintubated patients with respiratory distress. Am J Emerg Med. 2009;27:1056–9.
van Loon K, van Rheineck Leyssius AT, van Zaane B, Denteneer M, Kalkman CJ. Capnography during deep sedation with propofol by nonanesthesiologists: a randomized controlled trial. Anesth Analg. 2014;119:49–55.
Bhananker SM, Posner KL, Cheney FW, Caplan RA, Lee LA, Domino KB. Injury and liability associated with monitored anesthesia care: a closed claims analysis. Anesthesiology. 2006;104:228–34.
Mimoz O, Benard T, Gaucher A, Frasca D, Debaene B. Accuracy of respiratory rate monitoring using a non-invasive acoustic method after general anaesthesia. Br J Anaesth. 2012;108:872–5.
Miner JR, Heegaard W, Plummer D. End-tidal carbon dioxide monitoring during procedural sedation. Acad Emerg Med. 2002;9:275–80.
Ramsay MA, Usman M, Lagow E, Mendoza M, Untalan E, De Vol E. The accuracy, precision and reliability of measuring ventilatory rate and detecting ventilatory pause by rainbow acoustic monitoring and capnometry. Anesth Analg. 2013;117:69–75.
Berzin TM, Sanaka S, Barnett SR, et al. A prospective assessment of sedation-related adverse events and patient and endoscopist satisfaction in ERCP with anesthesiologist-administered sedation. Gastrointest Endosc. 2011;73:710–7.
Voscopoulos C, Brayanov J, Ladd D, Lalli M, Panasyuk A, Freeman J. Special article: evaluation of a novel noninvasive respiration monitor providing continuous measurement of minute ventilation in ambulatory subjects in a variety of clinical scenarios. Anesth Analg. 2013;117:91–100.
Voscopoulos C, MacNabb CM, Freeman J, Galvagno SM, Ladd D, George E. Continuous non-invasive respiratory volume monitoring for the identification of patients at risk for opioid induced respiratory depression and obstructive breathing patterns. J Trauma Acute Surg. 2014;77:S208–15. doi:10.1097/TA.0000000000000400.
Voscopoulos C, MacNabb CM, Brayanov J, Qin L, Freeman J, Mullen GJ, Ladd D, George E. The evaluation of a non-invasive respiratory volume monitor in surgical patients undergoing elective surgery with general anesthesia. J Clin Monit Comput. 2014. doi:10.1007/s10877-014-9596-0.
Blouin RT, Seifert HA, Babenco HD, Conard PF, Gross JB. Propofol depresses the hypoxic ventilatory response during conscious sedation and isohypercapnia. Anesthesiology. 1993;79:1177–82.
Lee MH, Yang KH, Lee CS, et al. The effect-site concentration of propofol producing respiratory depression during spinal anesthesia. Korean J Anesthesiol. 2011;61:122–6.
American Society of Anesthesiologists Task Force on S. Analgesia by N-A. Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology. 2002;96:1004–17.
Goudra BG, Singh PM, Sinha AC. Outpatient endoscopic retrograde cholangiopancreatography: safety and efficacy of anesthetic management with a natural airway in 653 consecutive procedures. Saudi J Anaesth. 2013;7:259–65.
Lawrence M. PCO2 and alveolar ventilation. In: Pulmonary physiology in clinical practice: the essentials for patient care and evaluation, Illustrated edition. St Louis: C.V. Mosby; 1987. p. 74–88.
Acknowledgments
This study was supported by Respiratory Motion, Inc.
Conflict of interest
C. Marshall MacNabb is employed by Respiratory Motion, Inc. Drs. Holley, Georgiadis, Minasyan, Shukla, and Mathews declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Holley, K., MacNabb, C.M., Georgiadis, P. et al. Monitoring minute ventilation versus respiratory rate to measure the adequacy of ventilation in patients undergoing upper endoscopic procedures. J Clin Monit Comput 30, 33–39 (2016). https://doi.org/10.1007/s10877-015-9674-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-015-9674-y