Abstract
Purpose
Local impedance (LI) measurement from an ablation catheter is useful in predicting lesion size and acute success of pulmonary vein isolation (PVI). The LI variation can be described by absolute LI drop (ΔLID) or ΔLID/initial LI (%LID). We evaluated the utility of these parameters in predicting acute lesion durability during PVI using a novel catheter capable of measuring both LI and contact force (CF).
Methods
PVI with a targeted CF, power, and duration was performed in 23 consecutive patients with paroxysmal atrial fibrillation. LI was blinded to operators during ablation. Parameters for each RF application were collected and compared for acute successful lesions and gaps.
Results
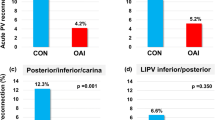
A total of 1633 RF applications including 97 (5.9%) gap lesions were analyzed. Successful lesions were more frequently observed at non-carinal sites and those with higher contact force, FTI, initial LI, and larger variation of LI and generator impedance (GI). Multivariate analysis demonstrated that absolute GI drop (ΔGID) [OR 1.09 (1.04–1.15), p < 0.001], ΔLID [1.12 (1.09–1.16), p < 0.001], ΔGID/initial GI (%GID) [OR 1.04 (1.01–1.07), p = 0.01], and %LID [OR 1.15 (1.12–1.28), p < 0.001] were significantly associated with successful lesions, and carinal site [OR 0.15(0.09–0.24), p < 0.001] was significantly related to gaps. Both ΔLID and %LID equally predicted the acute durability of lesions during PVI. ΔLID ≥ 24Ω and %LID ≥ 15% at the carina, and ΔLID ≥ 21Ω and %LID ≥ 14% at non-carinal sites significantly predicted acute successful lesions with negative predictive values of 93–99%.
Conclusions
Both ΔLID and %LID were equally useful in predicting acute successful lesions during PVI. Larger cut-off values should be applied to carinal sites.




Similar content being viewed by others
References
Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström-Lundqvist C, Boriani G, Castella M, Dan GA, Dilaveris PE, Fauchier L, Filippatos G, Kalman JM, La Meir M, Lane DA, Lebeau JP, Lettino M, Lip GYH, Pinto FJ, Thomas GN, Valgimigli M, Van Gelder IC, Van Putte BP, Watkins CL, ESC Scientific Document Group. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS. Eur Heart J. 2020;42:373–498.
Sulkin MS, Laughner JI, Hilbert S, Kapa S, Kosiuk J, Younan P, Romero I, Shuros A, Hamann JJ, Hindricks G, Bollmann A. Novel measure of local impedance predicts catheter-tissue contact and lesion formation. Circ Arrhythm Electrophysiol. 2018;11:e005831.
Das M, Luik A, Shepherd E, Sulkin M, Laughner J, Oesterlein T, Duffy E, Meyer C, Jais P, Duchateau J, Yue A, Ullah W, Ramos P, García-Bolao I. Local catheter impedance drop during pulmonary vein isolation predicts acute conduction block in patients with paroxysmal atrial fibrillation: initial results of the LOCALIZE clinical trial. Europace. 2021;23:1042–51.
Masuda M, Kanda T, Kurata N, Asai M, Iida O, Okamoto S, Ishihara T, Nanto K, Tsujimura T, Matsuda Y, Hata Y, Uematsu H, Mano T. Clinical utility of local impedance monitoring during pulmonary vein isolation. J Cardiovasc Electrophysiol. 2020;31:2584–91.
Martin CA, Martin R, Gajendragadkar PR, Maury P, Takigawa M, Cheniti G, Frontera A, Kitamura T, Duchateau J, Vlachos K, Bourier F, Lam A, Lord S, Murray S, Shephard E, Pambrun T, Denis A, Derval N, Hocini M, Haissaguerre M, Jais P, Sacher F. First clinical use of novel ablation catheter incorporating local impedance data. J Cardiovasc Electrophysiol. 2018;29:1197–206.
Segreti L, De Simone A, Schillaci V, Bongiorni MG, Pelargonio G, Pandozi C, Di Cori A, Stabile G, Pepe M, Zucchelli G, Shopova G, De Lucia R, Ferrari C, Casati F, Malacrida M, Solimene F. A novel local impedance algorithm to guide effective pulmonary vein isolation in atrial fibrillation patients: preliminary experience across different ablation sites from the CHARISMA pilot study. J Cardiovasc Electrophysiol. 2020;31:2319–27.
Garrott K, Laughner J, Gutbrod S, Sugrue A, Shuros A, Sulkin M, Yasin O, Bush J, Pottinger N, Meyers J, Kapa S. Combined local impedance and contact force for radiofrequency ablation assessment. Heart Rhythm. 2020;17:1371–80.
Szegedi N, Salló Z, Perge P, Piros K, Nagy VK, Osztheimer I, Merkely B, Gellér L. The role of local impedance drop in the acute lesion efficacy during pulmonary vein isolation performed with a new contact force sensing catheter-a pilot study. PLoS ONE. 2021;16:e0257050.
Inaba O, Nagata Y, Sekigawa M, Miwa N, Yamaguchi J, Miyamoto T, Goya M, Hirao K. Impact of impedance decrease during radiofrequency current application for atrial fibrillation ablation on myocardial lesion and gap formation. J Arrhythm. 2018;34:247–53.
Kaneshiro T, Kamioka M, Hijioka N, Yamada S, Yokokawa T, Misaka T, Hikichi T, Yoshihisa A, Takeishi Y. Characteristics of esophageal injury in ablation of atrial fibrillation using a high-power short-duration setting. Circ Arrhythm Electrophysiol. 2020;13:e008602.
Kimura M, Sasaki S, Owada S, Horiuchi D, Sasaki K, Itoh T, Ishida Y, Kinjo T, Tomita H, Okumura K. Comparison of lesion formation between contact force-guided and non-guided circumferential pulmonary vein isolation: a prospective, randomized study. Heart Rhythm. 2014;11:984–91.
Reddy VY, Dukkipati SR, Neuzil P, Natale A, Albenque JP, Kautzner J, Shah D, Michaud G, Wharton M, Harari D, Mahapatra S, Lambert H, Mansour M. Randomized, controlled trial of the safety and effectiveness of a contact force-sensing irrigated catheter for ablation of paroxysmal atrial fibrillation: results of the TactiCath Contact Force Ablation Catheter Study for Atrial Fibrillation (TOCCASTAR) study. Circulation. 2015;132:907–15.
Iwakawa H, Takigawa M, Goya M, Iwata T, Martin CA, Anzai T, Takahashi K, Amemiya M, Yamamoto T, Sekigawa M, Shirai Y, Tao S, Hayashi T, Takahashi Y, Watanabe H, Sasano T. Clinical implications of local impedance measurement using the IntellaNav MiFi OI ablation catheter: an ex vivo study. J Interv Card Electrophysiol. 2022;63:185–95.
Whitaker J, Rajani R, Chubb H, Gabrawi M, Varela M, Wright M, Niederer S, O’Neill MD. The role of myocardial wall thickness in atrial arrhythmogenesis. Europace. 2016;18:1758–72.
Chikata A, Kato T, Sakagami S, Kato C, Saeki T, Kawai K, Takashima S, Murai H, Usui S, Furusho H, Kaneko S, Takamura M. Optimal force-time integral for pulmonary vein isolation according to anatomical wall thickness under the ablation line. J Am Heart Assoc. 2016;5:e003155.
Ho SY, Anderson RH, Sánchez-Quintana D. Atrial structure and fibres: morphologic bases of atrial conduction. Cardiovasc Res. 2002;54:325–36.
Ho SY, Cabrera JA, Sánchez-Quintana D. Left atrial anatomy revisited. Circ Arrhythm Electrophysiol. 2012;5:220–8.
Lin YJ, Tsao HM, Chang SL, Lo LW, Tuan TC, Hu YF, Tsai WC, Chang CJ, Tai CT, Suenari K, Huang SY, Wu TJ, Chen SA. The distance between the vein and lesions predicts the requirement of carina ablation in circumferential pulmonary vein isolation. Europace. 2011;13:376–82.
Valles E, Fan R, Roux JF, Liu CF, Harding JD, Dhruvakumar S, Hutchinson MD, Riley M, Bala R, Garcia FC, Lin D, Dixit S, Callans DJ, Gerstenfeld EP, Marchlinski FE. Localization of atrial fibrillation triggers in patients undergoing pulmonary vein isolation: importance of the carina region. J Am Coll Cardiol. 2008;52:1413–20.
Amemiya M, Takigawa M, Goya M, Martin C, Anzai T, Takahashi K, Shimizu Y, Ikenouchi T, Kamata T, Yamamoto T, Nishimura T, Shirai Y, Tao S, Miyazaki S, Sasano T. Comparison of two catheters measuring local impedance: local impedance variation vs lesion characteristics and steam pops. J Inter Card Electrophy. 2022. https://doi.org/10.1007/s10840-022-01214-z.
Amorós-Figueras G, Jorge E, Alonso-Martin C, Traver D, Ballesta M, Bragós R, Rosell-Ferrer J, Cinca J. Endocardial infarct scar recognition by myocardial electrical impedance is not influenced by changes in cardiac activation sequence. Heart Rhythm. 2018;15:589–96.
Acknowledgements
We are grateful to Mr. Tomohiro Nagao, an employee of Boston Scientific Japan, for a technical support of this study.
Author information
Authors and Affiliations
Contributions
Each author contributes to this study as follows:
・Conception and design of the study: Masateru Takigawa (M.T) and Takashi Ikenouchi (T.I).
Acquisition of data: Yuki Shimizu (Y.S), Miki Amemiya (M.A), Tatsuaki Kamata (T.K), Takurou Nishimura (T.N), Susumu Tao (S.T), Shinsuke Miyazaki (S.M), Yoshihide Takahashi (Y.T), Masahiko Goya (M.G), Tetsuo Sasano (T.S), and M.T, and T.I.
・Analysis and interpretation of data: T.I, M.T, and M.G.
・Drafting of the article: T.I, M.T, and Claire Martin (C.M.)
・Revising the article critically for important intellectual content: T.I, M.T, C.M, M.G, S.M, and T.S
All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Research involving human participants and/or animals
The study was approved by the Ethics Review Board of Tokyo medical and dental university hospital.
Informed consent
All patients provided written informed consent.
Conflict of interest
Dr. Martin and Dr. Miyazaki have received consulting fees from Boston Scientific.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ikenouchi, T., Takigawa, M., Goya, M. et al. Requirement of larger local impedance reduction for successful lesion formation at carinal area during pulmonary vein isolation. J Interv Card Electrophysiol 65, 509–518 (2022). https://doi.org/10.1007/s10840-022-01282-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-022-01282-1