Abstract
Purpose
This study aims to better understand the knowledge and attitudes of men and women internationally towards oocyte cryopreservation (OC).
Methods
An online 25-question survey was distributed internationally via email and social media. Knowledge and attitudes towards OC among different regions and genders were assessed. The study population consisted of adults from North America (NA, 15.7%), Southeastern and Eastern Europe (SE, 34.7%), Central and Western Europe (CWE, 12.7%), Asia (12.7%), and Middle East (ME, 8.9%).
Results
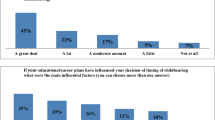
A total of 496 respondents initiated the survey and the completion rate was 80.2%. The mean (SD) age was 35.2 (12.1) years. Over 70% were aware of OC, but only 4.8% had previously undergone the procedure. Most considered ages 26–31 as optimal for OC and correctly identified conditions that could impact the chance of spontaneous conception.
Significant differences were observed regarding etiologies that would render OC acceptable. Only in NA and ME did solid majorities strongly agree that it is acceptable to proceed with OC to allow more time to find the right partner or for professional opportunities. More similar opinions were observed between genders. When medical conditions existed, large majorities across all nationalities and genders strongly agreed that OC is acceptable.
In NA, SE, and ME most respondents would consider or recommend OC for any reason, whereas most respondents in CWE and Asia would do that only for certain social reasons or medical necessity.
Conclusion
A good understanding of OC was observed. Nationality appeared to impact opinions on appropriate indications for this procedure, though overall positive attitudes were documented.






Similar content being viewed by others
Data availability
Data can be available upon request.
References
Johnston M, Richings NM, Leung A, Sakkas D, Catt S. A major increase in oocyte cryopreservation cycles in the USA, Australia and New Zealand since 2010 is highlighted by younger women but a need for standardized data collection. Hum Reprod. 2021;36(3):624–35. https://doi.org/10.1093/humrep/deaa320.
Peate M, Sandhu S, Braat S, Hart R, Norman R, Parle A, et al. Randomized control trial of a decision aid for women considering elective egg freezing: the Eggsurance study protocol. Womens Health (Lond). 2022;18:17455057221139672. https://doi.org/10.1177/17455057221139673.
Argyle CE, Harper JC, Davies MC. Oocyte cryopreservation: where are we now? Hum Reprod Update. 2016;22(4):440–9. https://doi.org/10.1093/humupd/dmw007.
Katler QS, Shandley LM, Hipp HS, Kawwass JF. National egg-freezing trends: cycle and patient characteristics with a focus on race/ethnicity. Fertil Steril. 2021;116(2):528–37. https://doi.org/10.1016/j.fertnstert.2021.02.032.
Kawwass JF, Shandley LM, Boulet SL, Hipp HS. Oncologic oocyte cryopreservation: national comparison of fertility preservation between women with and without cancer. J Assist Reprod Genet. 2020;37(4):883–90. https://doi.org/10.1007/s10815-020-01715-8.
Kawwass JF, Crawford S, Hipp HS. Frozen eggs: national autologous oocyte thaw outcomes. Fertil Steril. 2021;116(4):1077–84. https://doi.org/10.1016/j.fertnstert.2021.05.080.
Calhaz-Jorge C, De Geyter CH, Kupka MS, Wyns C, Mocanu E, Motrenko T, et al. 2020) Survey on ART and IUI: legislation, regulation, funding and registries in European countries: The European IVF-monitoring Consortium (EIM) for the European Society of Human Reproduction and Embryology (ESHRE. Hum Reprod Open. 2020;1(2020):hoz044. https://doi.org/10.1093/hropen/hoz044.
Europe EWGoOCi, Shenfield F, de Mouzon J, Scaravelli G, Kupka M, Ferraretti AP, et al. (2017) Oocyte and ovarian tissue cryopreservation in European countries: statutory background, practice, storage and use. Hum Reprod Open. 2017(1):hox003https://doi.org/10.1093/hropen/hox003
Pai HD, Baid R, Palshetkar NP, Pai A, Pai RD, Palshetkar R. Oocyte cryopreservation — current scenario and future perspectives: a narrative review. J Hum Reprod Sci. 2021;14(4):340–9. https://doi.org/10.4103/jhrs.jhrs_173_21.
Doyle JO, Richter KS, Lim J, Stillman RJ, Graham JR, Tucker MJ. Successful elective and medically indicated oocyte vitrification and warming for autologous in vitro fertilization, with predicted birth probabilities for fertility preservation according to number of cryopreserved oocytes and age at retrieval. Fertil Steril. 2016;105(2):459-66 e2. https://doi.org/10.1016/j.fertnstert.2015.10.026.
Jones BP, Kasaven L, L’Heveder A, Jalmbrant M, Green J, Makki M, et al. Perceptions, outcomes, and regret following social egg freezing in the UK; a cross-sectional survey. Acta Obstet Gynecol Scand. 2020;99(3):324–32. https://doi.org/10.1111/aogs.13763.
Seyhan A, Akin OD, Ertas S, Ata B, Yakin K, Urman B. A survey of women who cryopreserved oocytes for non-medical indications (social fertility preservation). Reprod Sci. 2021;28(8):2216–22. https://doi.org/10.1007/s43032-021-00460-2.
Ethics Committee of the American Society for Reproductive Medicine. (2018) Electronic address aao, Ethics Committee of the American Society for Reproductive M. Planned oocyte cryopreservation for women seeking to preserve future reproductive potential: an Ethics Committee opinion. Fertil Steril. 110(6):1022–8. https://doi.org/10.1016/j.fertnstert.2018.08.027.
Borovecki A, Tozzo P, Cerri N, Caenazzo L. Social egg freezing under public health perspective: just a medical reality or a women’s right? An ethical case analysis. J Public Health Res. 2018;7(3):1484. https://doi.org/10.4081/jphr.2018.1484.
Bracewell-Milnes T, Norman-Taylor J, Nikolaou D. Social egg freezing should be offered to single women approaching their late thirties: AGAINST: women should be freezing their eggs earlier. BJOG. 2018;125(12):1580. https://doi.org/10.1111/1471-0528.15295.
Chronopoulou E, Raperport C, Sfakianakis A, Srivastava G, Homburg R. Elective oocyte cryopreservation for age-related fertility decline. J Assist Reprod Genet. 2021;38(5):1177–86. https://doi.org/10.1007/s10815-021-02072-w.
Kostenzer J, Bos AME, Bont A, Exel JV. Unveiling the controversy on egg freezing in The Netherlands: a Q-methodology study on women’s viewpoints. Reprod Biomed Soc Online. 2021;12:32–43. https://doi.org/10.1016/j.rbms.2020.09.009.
Ismaili M’hamdi H, Hilhorst M, Steegers EAP, de Beaufort I. (2017) Nudge me, help my baby: on other-regarding nudges. J Med Ethics. 43(10):702–6. https://doi.org/10.1136/medethics-2016-103656.
Gupta S, Amir J, Petersen A, Haider S, York S. Insurance coverage for planned oocyte cryopreservation and infertility across US Medical, Law, and Master of Business Administration schools. Fertil Steril. 2023;120(2):384–5. https://doi.org/10.1016/j.fertnstert.2023.04.025.
Tozzo P, Fassina A, Nespeca P, Spigarolo G, Caenazzo L. Understanding social oocyte freezing in Italy: a scoping survey on university female students’ awareness and attitudes. Life Sci Soc Policy. 2019;15(1):3. https://doi.org/10.1186/s40504-019-0092-7.
Lallemant C, Vassard D, Nyboe Andersen A, Schmidt L, Macklon N. Medical and social egg freezing: internet-based survey of knowledge and attitudes among women in Denmark and the UK. Acta Obstet Gynecol Scand. 2016;95(12):1402–10. https://doi.org/10.1111/aogs.13024.
Stoop D, Nekkebroeck J, Devroey P. A survey on the intentions and attitudes towards oocyte cryopreservation for non-medical reasons among women of reproductive age. Hum Reprod. 2011;26(3):655–61. https://doi.org/10.1093/humrep/deq367.
O’Brien Y, Martyn F, Glover LE, Wingfield MB. What women want? A scoping survey on women’s knowledge, attitudes and behaviours towards ovarian reserve testing and egg freezing. Eur J Obstet Gynecol Reprod Biol. 2017;217:71–6. https://doi.org/10.1016/j.ejogrb.2017.08.024.
Tan SQ, Tan AW, Lau MS, Tan HH, Nadarajah S. Social oocyte freezing: a survey among Singaporean female medical students. J Obstet Gynaecol Res. 2014;40(5):1345–52. https://doi.org/10.1111/jog.12347.
Nargund G. Declining birth rate in developed countries: a radical policy re-think is required. Facts Views Vis Obgyn. 2009;1(3):191–3.
Mills M, Rindfuss RR, McDonald P, te Velde E, Reproduction E, Society Task F. (2011) Why do people postpone parenthood? Reasons and social policy incentives. Hum Reprod Update. 17(6):848-60https://doi.org/10.1093/humupd/dmr026
Skouteris H, Savaglio M. (2021) The use of social media for preconception information and pregnancy planning among young women. J Clin Med. 10(9). https://doi.org/10.3390/jcm10091892.
Sormunen T, Westerbotn M, Aanesen A, Fossum B, Karlgren K. Social media in the infertile community—using a text analysis tool to identify the topics of discussion on the multitude of infertility blogs. Womens Health (Lond). 2021;17:17455065211063280. https://doi.org/10.1177/17455065211063280.
Matsuda S, Aoki K, Tomizawa S, Sone M, Tanaka R, Kuriki H, et al. Analysis of patient narratives in disease blogs on the Internet: an exploratory study of social pharmacovigilance. JMIR Public Health Surveill. 2017;3(1): e10. https://doi.org/10.2196/publichealth.6872.
Sormunen T, Karlgren K, Aanesen A, Fossum B, Westerbotn M. The role of social media for persons affected by infertility. BMC Womens Health. 2020;20(1):112. https://doi.org/10.1186/s12905-020-00964-0.
Schick M, Sexty R, Ditzen B, Wischmann T. Attitudes towards social oocyte freezing from a socio-cultural perspective. Geburtshilfe Frauenheilkd. 2017;77(7):747–55. https://doi.org/10.1055/s-0043-111412.
Wennberg AL, Rodriguez-Wallberg KA, Milsom I, Brannstrom M. Attitudes towards new assisted reproductive technologies in Sweden: a survey in women 30–39 years of age. Acta Obstet Gynecol Scand. 2016;95(1):38–44. https://doi.org/10.1111/aogs.12781.
Ikhena-Abel DE, Confino R, Shah NJ, Lawson AK, Klock SC, Robins JC, et al. Is employer coverage of elective egg freezing coercive?: a survey of medical students’ knowledge, intentions, and attitudes towards elective egg freezing and employer coverage. J Assist Reprod Genet. 2017;34(8):1035–41. https://doi.org/10.1007/s10815-017-0956-9.
Bloom G, Katsuma Y, Rao KD, Makimoto S, Yin JDC, Leung GM. Next steps towards universal health coverage call for global leadership. BMJ. 2019;365:l2107. https://doi.org/10.1136/bmj.l2107.
Acknowledgements
The authors thank all the colleagues who assisted with the distribution of surveys in the different regions as well as all the respondents who participated in the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These findings were presented as an abstract in the American Society for Reproductive Medicine (ASRM) Scientific Congress & Expo 2023.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vagios, S., Sun, B., Yeh, J. et al. International attitudes towards medical and planned oocyte cryopreservation. J Assist Reprod Genet (2024). https://doi.org/10.1007/s10815-024-03116-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10815-024-03116-7