Abstract
Purpose
Assisted reproductive technology (ART) is commonly used to achieve pregnancy and often results in dichorionic diamniotic (DCDA) twin pregnancies. However, the potential risks of ART on maternal and neonatal outcomes in these pregnancies are not well understood. The objective is to compare the maternal and neonatal outcomes in DCDA twin pregnancies between those achieved through ART and those spontaneously conceived (SC).
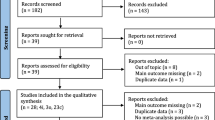
Methods
We carried out a systematic comprehensive search of electronic databases; namely, PubMed, Embase, Scopus, and the Cochrane Library, from inception to March 2023 with a study period of recruitment between 2003 and 2023. We included all studies comparing the maternal and neonatal outcomes of DCDA twin pregnancies between those achieved by ART and those SC.
Results
We analyzed data from 18 cohort studies involving 10,485 women with DCDA twin pregnancies. The meta-analysis showed that ART-conceived pregnancies had a significantly higher risk of preeclampsia or gestational hypertension (GH), gestational diabetes mellitus (GDM), placenta previa (PP), placental abruption (PA), postpartum hemorrhage (PPH), and elective and emergency cesarean sections than SC twin pregnancies. The absolute risks of these complications remained relatively low. We also found a slightly higher risk of respiratory distress syndrome (RDS) and congenital malformations in ART-conceived infants compared to the risks in SC infants. Finally, the risk of neonatal intensive care unit (NICU) admissions was significantly higher in ART-conceived infants than in SC infants, but with high heterogeneity.
Conclusion
We found associations between DCDA twin pregnancies conceived through ART and increased frequencies of adverse maternal outcomes. However, the absolute risks of these complications remained low, and the benefits of ART for achieving successful pregnancies may well outweigh the potential risks. Additionally, ART-conceived DCDA twin pregnancies may pose higher risks of RDS, congenital malformations and NICU, admissions than SC DCDA twin pregnancies.

Similar content being viewed by others
References
de Mouzon J, Chambers GM, Zegers-Hochschild F, Mansour R, Ishihara O, Banker M, et al. International Committee for Monitoring Assisted Reproductive Technologies world report: assisted reproductive technology 2012†. Hum Reprod Oxf Engl. 2020;35:1900–13.
De Geyter C. Assisted reproductive technology: impact on society and need for surveillance. Best Pract Res Clin Endocrinol Metab. 2019;33:3–8.
Baxi A, Kaushal M. Outcome of twin pregnancies conceived after assisted reproductive techniques. J Hum Reprod Sci. 2008;1:25–8.
Wang Y, Shi H, Chen L, Zheng D, Long X, Zhang Y, et al. Absolute risk of adverse obstetric outcomes among twin pregnancies after in vitro fertilization by maternal age. JAMA Netw Open. 2021;4:e2123634.
Martínez-Varea A, Martínez-Gómez M, Novillo B, Domenech J, Morales-Roselló J, Diago-Almela V. Perinatal outcomes of monochorionic twin pregnancies conceived naturally versus through assisted reproductive techniques. J Clin Med. 2023;12:6097.
Kozinszky Z, Surányi A. The high-risk profile of selective growth restriction in monochorionic twin pregnancies. Medicina (Mex). 2023;59:648.
Duy Anh N, Thu Ha NT, Khac Toan N, Tuan Dat D, Huyen Thuong PT, Tra Giang DT, et al. Obstetric and perinatal outcomes of dichorionic-diamniotic twin pregnancies conceived by iVF/ICSI compared with those conceived spontaneously. Clin Ter. 2022;173:155–63.
Elfituri A, Bakker W, Viswanatha R, Robinson E, Jan H, Ganapathy R. Maternal and perinatal outcomes of dichorionic diamniotic twins in women after spontaneous and assisted conception. Eur J Obstet Gynecol Reprod Biol. 2021;263:247–51.
Wang M, Chai J. Comparison of outcomes of monochorionic twin pregnancies conceived by assisted reproductive technology vs. spontaneous conceptions: a systematic review and meta-analysis. Front Pediatr. 2022;10:962190. https://doi.org/10.3389/fped.2022.962190.
Qin JB, Wang H, Sheng X, Xie Q, Gao S. Assisted reproductive technology and risk of adverse obstetric outcomes in dichorionic twin pregnancies: a systematic review and meta-analysis. Fertil Steril. 2016;105:1180–92.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700.
Dai F, Pan S, Lan Y, Tan H, Li J, Hua Y. Pregnancy outcomes and risk factors for preeclampsia in dichorionic twin pregnancies after in vitro fertilization: a five-year retrospective study. BMC Pregnancy Childbirth. 2022;22:830.
Prats P, Zarragoitia J, Rodríguez MÁ, Rodriguez I, Martinez F, Rodríguez-Melcon A, et al. Outcome in a series of 1135 twin pregnancies: does the type of conception play a role? AJOG Glob Rep. 2022;2:100129.
Lin D, Li P, Fan D, Chen G, Wu S, Ye S, et al. Association between IVF/ICSI treatment and preterm birth and major perinatal outcomes among dichorionic-diamnionic twin pregnancies: a seven-year retrospective cohort study. Acta Obstet Gynecol Scand. 2021;100:162–9.
Rashid D, Alalaf S. Maternal and perinatal outcomes in twin pregnancies conceived spontaneously and by assisted reproductive techniques: cross-sectional study. East Mediterr Health J. 2020;26:1285–93.
Seravalli V, Maoloni L, Pasquini L, Bolzonella S, Sisti G, Petraglia F, et al. The impact of assisted reproductive technology on prenatally diagnosed fetal growth restriction in dichorionic twin pregnancies Mastrolia SA, editor. PLOS ONE. 2020;15:e0231028.
Hessami K, Kasraeian M, Moghaddamizadeh Shoushtari S, Hessami A. Maternal and neonatal outcomes of monochorionic and dichorionic twin pregnancies following assisted reproductive technology in Southern Iranian women. Shiraz E-Med J. 2020;21(3):e92201. https://doi.org/10.5812/semj.92201.
Chen H, Wan Y, Xi H, Su W, Cheng J, Zhu C, et al. Obstetric and perinatal outcomes of dizygotic twin pregnancies resulting from in vitro fertilization versus spontaneous conception: a retrospective study. PeerJ. 2019;7:e6638.
Barda G, Gluck O, Mizrachi Y, Bar J. A comparison of maternal and perinatal outcome between in vitro fertilization and spontaneous dichorionic-diamniotic twin pregnancies. J Matern Fetal Neonatal Med. 2017;30:2974–7.
Sun L, Zou G, Wei X, Chen Y, Zhang J, Okun N, et al. Clinical outcomes after assisted reproductive technology in twin pregnancies: chorionicity-based comparison. Sci Rep. 2016;6:26869.
Pourali L, Ayati S, Jelodar S, Zarifian A, Sheikh Andalibi MS. Obstetrics and perinatal outcomes of dichorionic twin pregnancy following ART compared with spontaneous pregnancy. Int J Reprod Biomed. 2016;14:317–22.
Geisler ME, O’Mahony A, Meaney S, Waterstone JJ, O’Donoghue K. Obstetric and perinatal outcomes of twin pregnancies conceived following IVF/ICSI treatment compared with spontaneously conceived twin pregnancies. Eur J Obstet Gynecol Reprod Biol. 2014;181:78–83.
Caserta D, Bordi G, Stegagno M, Filippini F, Podagrosi M, Roselli D, et al. Maternal and perinatal outcomes in spontaneous versus assisted conception twin pregnancies. Eur J Obstet Gynecol Reprod Biol. 2014;174:64–9.
Anbazhagan A, Hunter A, Breathnach FM, Mcauliffe FM, Geary MP, Daly S, et al. Comparison of outcomes of twins conceived spontaneously and by artificial reproductive therapy. J Matern Fetal Neonatal Med. 2014;27:458–62.
Egic AS, Mojovic DV, Milovanovic ZM, Jurisic AB, Srbinovic LP, Krsmanovic SP, et al. Degree and rate of growth discordance in dichorionic twins conceived by in vitro fertilization. Obstet Gynecol Int. 2014;2014:1–6.
Fan C, Sun Y, Yang J, Ye J, Wang S. Maternal and neonatal outcomes in dichorionic twin pregnancies following IVF treatment: a hospital-based comparative study. Int J Clin Exp Pathol. 2013;6:2199–207.
Hu X. Twin pregnancies obtained with <I>in vitro</I> fertilization and embryo transfer and spontaneous pregnancy: a comparison of pregnancy outcomes: twin pregnancies obtained with <I>in vitro</I> fertilization and embryo transfer and spontaneous pregnancy: a comparison of pregnancy outcomes. Acad J Second Mil Med Univ. 2013;32:694–5.
Moini A, Shiva M, Arabipoor A, Hosseini R, Chehrazi M, Sadeghi M. Obstetric and neonatal outcomes of twin pregnancies conceived by assisted reproductive technology compared with twin pregnancies conceived spontaneously: a prospective follow-up study. Eur J Obstet Gynecol Reprod Biol. 2012;165:29–32.
Vasario E, Borgarello V, Bossotti C, Libanori E, Biolcati M, Arduino S, et al. IVF twins have similar obstetric and neonatal outcome as spontaneously conceived twins: a prospective follow-up study. Reprod Biomed Online. 2010;21:422–8.
Elias S, Wolde Z, Tantu T, Gunta M, Zewudu D. Determinants of early neonatal outcomes after emergency cesarean delivery at Hawassa University comprehensive specialised hospital, Hawassa. Ethiopia PLOS ONE. 2022;17:e0263837.
Ghahiri A, Khosravi M. Maternal and neonatal morbidity and mortality rate in caesarean section and vaginal delivery. Adv Biomed Res. 2015;4:193.
Qin J, Sheng X, Wang H, Liang D, Tan H, Xia J. Assisted reproductive technology and risk of congenital malformations: a meta-analysis based on cohort studies. Arch Gynecol Obstet. 2015;292:777–98.
Hoorsan H, Mirmiran P, Chaichian S, Moradi Y, Hoorsan R, Jesmi F. Congenital malformations in infants of mothers undergoing assisted reproductive technologies: a systematic review and meta-analysis study. J Prev Med Pub Health. 2017;50:347–60.
Gupta P, Faridi MMA, Dev G. Congenital malformations in twins: effect of chorionicity and zygosity. Indian Pediatr. 2010;47:343–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed consent
None.
Research involving human participants and/or animals
None.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, L., Dong, Q. & Weng, R. Maternal and neonatal outcomes of dichorionic twin pregnancies achieved with assisted reproductive technology: meta-analysis of contemporary data. J Assist Reprod Genet 41, 581–589 (2024). https://doi.org/10.1007/s10815-024-03035-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-024-03035-7