Abstract
Purpose
Assess the rate, rationale, and characteristics of patients who cryopreserved and subsequently discarded their oocytes, and compare their characteristics to patients with continued cryopreservation of oocytes.
Methods
All patients who disposed of cryopreserved oocytes between 2009 and 2022 reported their reason for discarding their oocytes. This was a retrospective cohort study.
Results
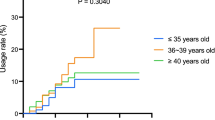
Of 5,010 patients who underwent oocyte cryopreservation (OC) cycles, 201 (4%) patients elected to discard their oocytes and 751 (15%) thawed oocytes for clinical use. The average ages of OC and disposal were 35 and 39 years old, respectively. Of the 201 patients who discarded their oocytes, 71 patients (35%) requested disposal after having a child. Twenty-six (13%) discarded oocytes because of worsening cancer and three (1.4%) discarded because of death. 16 (8%) discarded oocytes due to cost of cryopreservation and eight (4%) due to low oocyte yield. Ten (5%) patients underwent new IVF cycles and discarded previously stored oocytes. Sixty-seven patients (33%) discarded oocytes for unspecified reasons. When comparing patients who discarded oocytes with those who did not, the former had lower AMH (2.7 vs 3.5 ng/ml, p < 0.001) but otherwise comparable age and number of cryopreserved oocytes. The mean age for those with continued cryopreservation was 35.4 years at time of OC and 40 years at time of data collection in June 2023.
Conclusion
Childbirth was the most common reason to dispose of oocytes followed by unspecified reasons. Larger studies of oocyte disposal may better define clinical characteristics of patients most likely to use, maintain or discard their oocytes.


Similar content being viewed by others
Data availability
Data regarding study subjects has not been previously published. Primary data will be made available to editors, reviewers, or researchers upon request.
References
Cobo A, García-Velasco JA, Remohí J, Pellicer A. Oocyte vitrification for fertility preservation for both medical and nonmedical reasons. Fertil Steril. 2021;115(5):1091–101. https://doi.org/10.1016/j.fertnstert.2021.02.006.
Jones BP, Kasaven L, L’Heveder A, Jalmbrant M, Green J, Makki M, Odia R, Norris G, Bracewell Milnes T, Saso S, Serhal P, Ben NJ. Perceptions, outcomes, and regret following social egg freezing in the UK; a cross-sectional survey. Acta Obstet Gynecol Scand. 2020;99(3):324–32. https://doi.org/10.1111/aogs.13763.
Doyle JO, Richter KS, Lim J, Stillman RJ, Graham JR, Tucker MJ. Successful elective and medically indicated oocyte vitrification and warming for autologous in vitro fertilization, with predicted birth probabilities for fertility preservation according to number of cryopreserved oocytes and age at retrieval. Fertil Steril. 2016;105(2):459-66.e2. https://doi.org/10.1016/j.fertnstert.2015.10.026.
Cobo A, García-Velasco JA, Coello A, Domingo J, Pellicer A, Remohí J. Oocyte vitrification as an efficient option for elective fertility preservation. Fertil Steril. 2016;105(3):755-764.e8. https://doi.org/10.1016/j.fertnstert.2015.11.027.
Devine K, Mumford SL, Goldman KN, Hodes-Wertz B, Druckenmiller S, Propst AM, Noyes N. Baby budgeting: oocyte cryopreservation in women delaying reproduction can reduce cost per live birth. Fertil Steril. 2015;103(6):1446–53.e1–2. https://doi.org/10.1016/j.fertnstert.2015.02.029.
Bakkensen JB, Flannagan KSJ, Mumford SL, Hutchinson AP, Cheung EO, Moreno PI, Jordan N, Feinberg EC, Goldman KN. A SART data cost-effectiveness analysis of planned oocyte cryopreservation versus in vitro fertilization with preimplantation genetic testing for aneuploidy considering ideal family size. Fertil Steril. 2022;118(5):875–84. https://doi.org/10.1016/j.fertnstert.2022.07.022.
Patrizio P, Molinari E, Caplan A. Ethics of medical and nonmedical oocyte cryopreservation. Curr Opin Endocrinol Diabetes Obes. 2016;23(6):470–5. https://doi.org/10.1097/MED.0000000000000292.
Hodes-Wertz B, Druckenmiller S, Smith M, Noyes N. What do reproductive-age women who undergo oocyte cryopreservation think about the process as a means to preserve fertility? Fertil Steril. 2013;100(5):1343–9. https://doi.org/10.1016/j.fertnstert.2013.07.201.
Argyle CE, Harper JC, Davies MC. Oocyte cryopreservation: where are we now? Hum Reprod Update. 2016;22(4):440–9. https://doi.org/10.1093/humupd/dmw007.
Caughey LE, Lensen S, White KM, Peate M. Disposition intentions of elective egg freezers toward their surplus frozen oocytes: a systematic review and meta-analysis. Fertil Steril. 2021;116(6):1601–19. https://doi.org/10.1016/j.fertnstert.2021.07.1195.
Caughey LE, White KM. Psychosocial determinants of women’s intentions and willingness to freeze their eggs. Fertil Steril. 2021;115(3):742–52. https://doi.org/10.1016/j.fertnstert.2020.09.150.
Kuwayama M, Vajta G, Kato O, Leibo SP. Highly efficient vitrification method for cryopreservation of human oocytes. Reprod Biomed Online. 2005;11(3):300–8. https://doi.org/10.1016/s1472-6483(10)60837-1.
Center for Disease Control and Prevention, American Society for Reproductive Medicine, Society for Assisted Reproductive Technology. 2018 Assisted Reproductive Technology Success Rates: National Summary and Fertility Clinic Reports. Washington, D.C.: U.S. Dept. of Health and Human Services; 2018.
Richter KS, Ginsburg DK, Shipley SK, Lim J, Tucker MJ, Graham JR, et al. Factors associated with birth outcomes from cryopreserved blastocysts: experience from 4,597 autologous transfers of 7,597 cryopreserved blastocysts. Fertil Steril. 2016;106:354-362.e2.
Petropanagos A, Cattapan A, Baylis F, Leader A. Social egg freezing: risk, benefits and other considerations. CMAJ. 2015;187(9):666–9. https://doi.org/10.1503/cmaj.141605.
Iussig B, Maggiulli R, Fabozzi G, Bertelle S, Vaiarelli A, Cimadomo D, Ubaldi FM, Rienzi L. A brief history of oocyte cryopreservation: Arguments and facts. Acta Obstet Gynecol Scand. 2019;98(5):550–8. https://doi.org/10.1111/aogs.13569.
Practice Committee of the American Society for Reproductive Medicine. Evidence-based outcomes after oocyte cryopreservation for donor oocyte in vitro fertilization and planned oocyte cryopreservation: a guideline. Fertil Steril. 2021;116(1):36–47. https://doi.org/10.1016/j.fertnstert.2021.02.024.
Acknowledgements
The authors would like to thank Shady Grove Fertility for aid in the analysis and research collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
IRB approved—The Advarra Institutional Review Board approved the retrospective review and analysis of the data collected during routine clinical care; Shady Grove Fertility Reproductive Science Center—R2009.1, Retrospective Analysis of Factors Associated with Outcomes of Infertility Treatment (Pro00027148).
Informed consent
Not required.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Namath, A., Jahandideh, S., Devine, K. et al. Examining reasons that patients discard cryopreserved oocytes. J Assist Reprod Genet 40, 2865–2870 (2023). https://doi.org/10.1007/s10815-023-02962-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-023-02962-1