Abstract
Purpose
To determine the utilization of planned oocyte cryopreservation (OC) in the year immediately prior to, and the year of, insurance coverage commencement for employees at our institution.
Methods
Patient demographics and cycle outcomes were retrospectively compared between the first OC cycles occurring in 2017 vs. 2018 according to insurance coverage and type, age, and the number of oocytes retrieved and cryopreserved. Continuous demographic variables including age, BMI, day 3 FSH and E2, AMH, gravidity, and parity were compared using student T-tests. Cycle outcomes, including the number of oocytes retrieved and cryopreserved were compared using linear regression models, adjusting for potential confounders including age, BMI, and ovarian reserve parameters.
Results
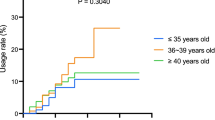
Between January 2017 and December 2018, 123 patients underwent planned OC at our institution. Patient age ranged from 23 to 44 years and did not significantly differ from 2017 to 2018 (mean 34.9 vs. 35.2). There was a 12% increase in planned OC utilization from 2017 (N = 58) to 2018 (N = 65). Significantly, more patients had any insurance coverage in 2018 vs. 2017 (71.9% vs. 40.4%, p = 0.001), a 78% increase. From 2017 to 2018, the number of patients with hospital-based insurance coverage undergoing planned OC increased by a factor of 8 (5 to 41.5%, p < 0.001), while the number of self-pay patients significantly decreased (p = 0.001). No differences were found regarding cycle outcomes.
Conclusion
A greater proportion of women at our institution had insurance coverage for planned OC in 2018 vs. 2017. Employer-based insurance coverage for planned OC was associated with a significant increase in utilization by hospital employees.

Similar content being viewed by others
References
OECD Family Database, SF2.3: mean age of mothers at first childbirth. 2019. Last updated: Available at: https://www.oecd.org/els/soc/SF_2_3_Age_mothers_childbirth.pdf
NCHS Pressroom - 2002 News Release - Mean age of mother.” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, 20 Aug. 2014, Available at: www.cdc.gov/nchs/pressroom/02news/ameriwomen.htm#:~:text=In%201970%20the%20average%20age,over%20the%20past%20three%20decades.).
Matthews TJ, Hamilton BE. Delayed childbearing: more women are having their first child later in life. NCHS Data Brief. 2009;21:1–8.
Heck KE, Schoendorf KC, Ventura SJ, Kiely JL. Delayed childbearing by education level in the United States, 1969–1994. Maternal and child health journal. 1997;1(2):81–88. Availabel at: https://doi.org/10.1023/a:1026218322723
Hook EB. Rates of chromosome abnormalities at different maternal ages. Obstet Gynecol. 1981;58(3):282–5.
Nybo Andersen AM, Wohlfahrt J, Christens P, Olsen J, Melbye M. Maternal age and fetal loss: population based register linkage study. BMJ (Clinical research ed). 2000;320(7251):1708–12. https://doi.org/10.1136/bmj.320.7251.1708.
Sauer MV, Paulson RJ, Lobo RA. Pregnancy after age 50: application of oocyte donation to women after natural menopause. Lancet (London, England). 1993;341(8841):321–3. https://doi.org/10.1016/0140-6736(93)90132-z.
Hodes-Wertz B, Druckenmiller S, Smith M, Noyes N. What do reproductive-age women who undergo oocyte cryopreservation think about the process as a means to preserve fertility? Fertil Steril. 2013;100(5):1343–9. https://doi.org/10.1016/j.fertnstert.2013.07.201.
Cobo A, Pérez S, De los Santos MJ, Zulategui J, Domingo J, Remohí J. Effect of different cryopreservation protocols on the metaphase II spindle in human oocytes. Reprod Biomed Online. 2008;17(3):350–9. https://doi.org/10.1016/s1472-6483(10)60218-0.
Cobo A, Kuwayama M, Pérez S, Ruiz A, Pellicer A, Remohí J. Comparison of concomitant outcome achieved with fresh and cryopreserved donor oocytes vitrified by the Cryotop method. Fertil Steril. 2008;89(6):1657–64. https://doi.org/10.1016/j.fertnstert.2007.05.050.
Cobo A, Meseguer M, Remohí J, Pellicer A. Use of cryo-banked oocytes in an ovum donation programme: a prospective, randomized, controlled, clinical trial. Hum Reprod (Oxford, England). 2010;25(9):2239–46. https://doi.org/10.1093/humrep/deq146.
Rienzi L, Romano S, Albricci L, Maggiulli R, Capalbo A, Baroni E, Colamaria S, Sapienza F, Ubaldi F. Embryo development of fresh ‘versus’ vitrified metaphase II oocytes after ICSI: a prospective randomized sibling-oocyte study. Hum Reprod (Oxford, England). 2010;25(1):66–73. https://doi.org/10.1093/humrep/dep346.
Parmegiani L, Cognigni GE, Bernardi S, Cuomo S, Ciampaglia W, Infante FE, Tabarelli de Fatis C, Arnone A, Maccarini AM, Filicori M. Efficiency of aseptic open vitrification and hermetical cryostorage of human oocytes. Reprod Biomed Online. 2011;23(4):505–12. https://doi.org/10.1016/j.rbmo.2011.07.003.
Ethics Committee of the American Society for Reproductive Medicine. Electronic address: asrm@asrm.org, & Ethics Committee of the American Society for Reproductive Medicine. Planned oocyte cryopreservation for women seeking to preserve future reproductive potential: an Ethics Committee opinion. Fertil Steril. 2018;110(6):1022–8. https://doi.org/10.1016/j.fertnstert.2018.08.027.
Zoll M, Mertes H, Gupta J. Corporate giants provide fertility benefits: have they got it wrong? Eur J Obstet Gynecol Reprod Biol. 2015;195:A1–2. https://doi.org/10.1016/j.ejogrb.2015.10.018.
Bennett J. Egg freezing: Facebook, Apple, Citibank and delaying childbearing. Time. 2014. https://time.com/3509930/company-paid-egg-freezing-will-be-the-great-equalizer/#:~:text=Company%2DPaid%20Egg%20Freezing%20Will%20Be%20the%20Great%20Equalizer,-Egg%20storage&text=Updated%20on%20October%2016%20at%2011%3A25%20am.&text=It%20was%20a%20free%20seminar,already%20be%20reduced%20by%20half
Mertes H. Does company-sponsored egg freezing promote or confine women’s reproductive autonomy? J Assist Reprod Genet. 2015;32(8):1205–9. https://doi.org/10.1007/s10815-015-0500-8.
Mertes H, Pennings G. Elective oocyte cryopreservation: who should pay? Human Reprod (Oxford, England). 2012;27(1):9–13. https://doi.org/10.1093/humrep/der364.
NY State Senate Bill S719. NY State Senate. (2020, January 9). https://www.nysenate.gov/legislation/bills/2019/s719.
Stoop D, van der Veen F, Deneyer M, Nekkebroeck J, Tournaye H. Oocyte banking for anticipated gamete exhaustion (AGE) is a preventive intervention, neither social nor nonmedical. Reprod Biomed Online. 2014;28(5):548–51. https://doi.org/10.1016/j.rbmo.2014.01.007.
Inhorn MC, Birenbaum-Carmeli D, Westphal LM, Doyle J, Gleicher N, Meirow D, Raanani H, Dirnfeld M, Patrizio P. Medical egg freezing: how cost and lack of insurance cover impact women and their families. Reprod Biomed Soc. 2018;5:82–92. https://doi.org/10.1016/j.rbms.2017.12.001.
Quinn GP, Vadaparampil ST, Bell-Ellison BA, Gwede CK, Albrecht TL (2008). Patient-physician communication barriers regarding fertility preservation among newly diagnosed cancer patients. Soc Sci Med 1982, 66(3), 784–789. https://doi.org/10.1016/j.socscimed.2007.09.013
Ajala T, Rafi J, Larsen-Disney P, Howell R. Fertility preservation for cancer patients: a review. Obstet Gynecol Int. 2010;2010: 160386. https://doi.org/10.1155/2010/160386.
Rashedi AS, de Roo SF, Ataman LM, Edmonds ME, Silva AA, Scarella A, Horbaczewska A, Anazodo A, Arvas A, Ramalho de Carvalho B, Sartorio C, Beerendonk C, Diaz-Garcia C, Suh CS, Melo C, Yding Andersen C, Motta E, Greenblatt EM, Van Moer E, Zand E, Woodruff TK. Survey of fertility preservation options available to patients with cancer around the globe. JCO Glob Oncol. 2020, 6, JGO.2016.008144. https://doi.org/10.1200/JGO.2016.008144
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yeshua, A.S., Abittan, B., Bar-El, L. et al. Employer-based insurance coverage increases utilization of planned oocyte cryopreservation. J Assist Reprod Genet 39, 1393–1397 (2022). https://doi.org/10.1007/s10815-022-02506-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-022-02506-z