Abstract
Purpose
This study aimed to investigate the relationship between the number of oocytes retrieved and clinical outcomes in young women with normal ovarian reserve who were undergoing their first in vitro fertilization and embryo transfer (IVF-ET) cycle. The transfer strategy based on yielded oocytes was also discussed in this article.
Methods
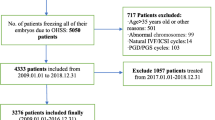
A total of 1567 patients who underwent first long protocol of IVF treatment in our reproductive medical center between January 2010 and June 2014 were categorized into five groups based on the retrieved oocyte number, namely, 4∼6, 7∼9, 10∼12, 13∼15, and ≥16. Baseline parameters were similar among the groups. Primary outcome was defined as the cumulative live birth rate (CLBR), and secondary outcomes included the rate of patients with high risks for ovarian hyperstimulation syndrome (OHSS).
Results
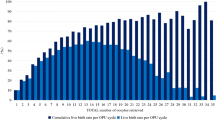
It was found that the CLBR increased with the number of oocytes, as well as the rate for high risks of OHSS. In fresh cycles, 10∼12 oocyte group demonstrated the highest implantation rate (53.32 %), clinical pregnancy rate (CPR) (73.13 %), and live birth rate (LBR) (61.14 %), with no significant differences. Moreover, both cumulative CPR (CCPR) and CLBR became significantly higher in the 10∼12 oocyte group, compared with 4∼6 and 7∼9 groups. However, when the retrieved oocytes increased to 13∼15 or ≥16, the cumulative results did not have a significant increase. Also, the high risk rate of OHSS was much lower in the 10∼12 group (11.53 %) than that in the 13∼15 group (29.97 %) and ≥16 group (77.30 %). Unconditional multivariate logistic regression analysis showed that when ≥10 oocytes were retrieved, the CLBR increased significantly (P < 0.01). When oocyte number exceeded 16, the CPR of frozen embryo transfer cycle was much higher than that of fresh cycle (P < 0.05).
Conclusions
For young women with normal ovarian reserve, retrieving 10∼12 oocytes might result in optimized pregnancy outcomes in a fresh cycle with low OHSS risk and would not compromise cumulative outcomes. When ≥16 oocytes were retrieved, a “freeze-all” embryo strategy might be preferable.





Similar content being viewed by others
References
Steptoe PC, Edwards RG. Birth after the reimplantation of a human embryo. Lancet. 1978;12:366.
Evans J, Hannan NJ, Edgell TA, Vollenhoven BJ, Lutjen PJ, Osianlis T, et al. Fresh versus frozen embryo transfer: backing clinical decisions with scientific and clinical evidence. Hum Reprod Update. 2014;20:808–21.
Delbaere A, Devreker F, Hannes M, Koenig I, Holoye A, Englert Y. Evolution of ovarian stimulation in in vitro fertilization. Rev Med Brux. 1999;20:A446–52.
Stanger JD, Yovich JL. Follicle recruitment determines IVF productivity rate via the number of embryos frozen and subsequent transfers. Reprod Biomed Online. 2013;27:286–96.
Kably Ambe A, Estévez González S, Carballo Mondragón E, Durán ML. Comparative analysis of pregnancy rate/captured oocytes in an in vitro fertilization program. Ginecol Obstet Mex. 2008;76:256–60.
Bosch E, Ezcurra D. Individualised controlled ovarian stimulation (iCOS): maximising success rates for assisted reproductive technology patients. Reprod Biol Endocrino. 2011;9:82.
Briggs R, Kovacs G, MacLachlan V, Motteram C, Baker HW. Can you ever collect too many oocytes? Hum Reprod. 2015;30:81–7.
Sunkara SK, Rittenberg V, Raine-Fenning N, Bhattacharya S, Zamora J, Coomarasamy A. Association between the number of eggs and live birth in IVF treatment: an analysis of 400 135 treatment cycles. Hum Reprod. 2011;26:1768–74.
Hamoda H, Sunkara S, Khalaf Y, Braude P, El-Toukhy T. Outcome of fresh IVF/ICSI cycles in relation to the number of oocytes collected: a review of 4,701 treatment cycles. Hum Reprod. 2010;25:i47.
Steward RG, Lan L, Shah AA, Yeh JS, Price TM, Goldfarb JM, et al. Oocyte number as a predictor for ovarian hyperstimulation syndrome and live birth: an analysis of 256,381 in vitro fertilization cycles. Fertil Steril. 2014;101:967–73.
Ji J, Liu Y, Tong XH, Luo L, Ma J, Chen Z. The optimum number of oocytes in IVF treatment: an analysis of 2455 cycles in China. Hum Reprod. 2013;28:2728–34.
Baker VL, Brown MB. Luke B3, Conrad KP4. Association of number of retrieved oocytes with live birth rate and birth weight: an analysis of 231,815 cycles of in vitro fertilization. Fertil Steril. 2015;14:02551–5.
Meniru GI, Craft IL. Utilization of retrieved oocytes as an index of the efficiency of superovulation strategies for in-vitro fertilization treatment. Hum Reprod. 1997;12:2129–32.
Patrizio P, Sakkas D. From oocyte to baby: a clinical evaluation of the biological efficiency of in vitro fertilization. Fertil Steril. 2009;91:1061–6.
Brian Dale, Kay Elder. In vitro fertilization [M]. Cambridge University Press. 1997, 115.
He Q, Liang L, Zhang C, Li H, Ge Z, Wang L, et al. Effects of different doses of letrozole on the incidence of early-onset ovarian hyperstimulation syndrome after oocyte retrieval. Syst Biol Reprod Med. 2014;60:355–60.
Golan A, Ron-el R, Herman A, Soffer Y, Weinraub Z, Caspi E. Ovarian hyperstimulation syndrome: an update review. Obstet Gynecol Surv. 1989;44:430–40.
Cai QF, Wan F, Huang R, Zhang HW. Factors predicting the cumulativeoutcome of IVF/ICSI treatment: a multivariable analysis of 2450patients. Hum Reprod. 2011;26:2532–40.
Saldeen P, Källen K, Sundström P. The probability of successful IVF outcome after poor ovarian response. Acta Obstet Gynecol Scand. 2007;86:457–61.
Sansone P, Aurilio C, Pace MC, Esposito R, Passavanti MB, Pota V, et al. Intensive care treatment of ovarian hyperstimulation syndrome (OHSS). Ann N Y Acad Sci. 2011;1221:109–18.
Papanikolaou EG, Pozzobon C, Kolibianakis EM, Camus M, Tournaye H, Fatemi HM, et al. Incidence and prediction of ovarian hyperstimulationsyndrome in women undergoing gonadotropin-releasing hormone antagonistin vitro fertilization cycles. Fertil Steril. 2006;85:112–20.
Mitwally MF, Bhakoo HS, Crickard K, Sullivan MW, Batt RE, Yeh J. Estradiol production during controlled ovarian hyperstimulation correlates with treatment outcome in women undergoing in vitro fertilization-embryo transfer. Fertil Steril. 2006;86:588–96.
Valbuena D, Martin J, de Pablo JL, Remohí J, Pellicer A, Simón C. Increasing levels of estradiol are deleterious to embryonic implantation because they directly affect the embryo. Fertil Steril. 2001;76:962–8.
Venetis CA, Kolibianakis EM, Bosdou JK, Tarlatzis BC. Progesterone elevation and probability of pregnancy after IVF: a systematic review and meta-analysis of over 60 000 cycles. Hum Reprod Update. 2013;19:433–57.
Kok JD, Looman CW, Weima SM, TeVelde ER. A high number of oocytes obtained after ovarian hyperstimulation for in vitro fertilization or intracytoplasmic sperm injection is not associated with decreased pregnancy outcome. FertilSteril. 2006;85:918–24.
Acknowledgments
The authors thank everyone at the Reproductive Medical Center of Henan provincial People’s Hospital for their scientific advice and encouragement.
Conlfict of interest
The authors declare that they have no competing interests.
Author contributions
All authors made substantial contributions to the conception and design of this research study. C-yH and X-xH acquired and analyzed the data and wrote the manuscript. QW collected the data. Z-sD, J-lL, and G-zJ critically revised the manuscript. Z-cL finally approved the manuscript. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Capsule
For young women with normal ovarian reserve, retrieving 10∼12 oocytes might result in optimized pregnancy outcomes in consideration of both fresh and frozen transfers. With more than 16 oocytes, a “freeze-all” embryo strategy might be preferable
Yuan-hui Chen and Xiao-hang Xu contributed equally to this work.
Rights and permissions
About this article
Cite this article
Chen, Yh., Xu, Xh., Wang, Q. et al. Optimum oocyte retrieved and transfer strategy in young women with normal ovarian reserve undergoing a long treatment protocol: a retrospective cohort study. J Assist Reprod Genet 32, 1459–1467 (2015). https://doi.org/10.1007/s10815-015-0571-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-015-0571-6