Abstract
Purpose
Symptom control in the long-term with less side effects is important in perennial allergic conjunctivitis, since would improve quality of life. This study aimed to assess the clinical efficacies of topical cyclosporin A and subcutaneous allergen immunotherapy (SCIT) in terms of sign control in perennial allergic conjunctivitis.
Methods
This retrospective study included 20 adult patients with perennial allergic conjunctivitis and confirmed sensitization to house dust mites with skin prick test. Patients were assigned to either topical cyclosporine A treatment or SCIT. The participants were followed for 6 months, and signs scores were recorded at 1, 3 and 6 months.
Results
Overall, both cyclosporine and immunotherapy groups showed significant improvements in papillary reaction (p = 0.011 and 0.003, respectively), limbal involvement (p = 0.031 and 0.001), and conjunctival hyperemia (p = 0.001 and p < 0.001) scores during the 6-month follow-up. However, only cyclosporine group showed a significant improvement in corneal involvement scores (p = 0.015) during the study period. When scores at different time points were compared, significant improvement in conjunctival hyperemia was evident at 6 months in both groups when compared to baseline (cyclosporine group, 0.7 ± 0.68 vs. 2.4 ± 0.84, 70.8% decrease, p = 0.01; immunotherapy group, 0.3 ± 0.48 vs. 2.3 ± 0.95, 87.0% decrease, p = 0.004), whereas for limbal involvement such an improvement was only evident in the immunotherapy group (0.1 ± 0.32 vs. 1.3 ± 0.95, 92.3% decrease, p = 0.01).
Conclusions
Allergen immunotherapy and cyclosporin A treatment may provide effective sign relief in perennial allergic conjunctivitis. It may represent an encouraging treatment option particularly for cases with perennial allergic conjunctivitis refractive to other treatments and positive skin prick test to a specific allergen (house dust in the present study). Long-term relief by SCIT would reduce the side effects of polypharmacotherapy. Larger studies with longer follow-up are warranted to confirm our findings.
Similar content being viewed by others
Introduction
Allergic conjunctivitis (AC) is a chronic, bilateral ocular surface inflammation with recurrences and relapses. There are four types of AC that are seasonal allergic conjunctivitis (SAC), perennial allergic conjunctivitis (PAC), vernal keratoconjunctivitis, and atopic keratoconjunctivitis. Although the symptoms in the perennial form are similar to the seasonal form, allergic reaction in this form can often be triggered by allergens of organic origin and non-seasonal characteristics [1]. SAC is often characterized by an acute or subacute onset triggered by trees, grass, and weed pollens, and it is more common and may occur during periods of high allergen exposure. On the other hand, PAC tends to be caused by year-round allergens including house dust mites (HDM), some molds or pet danders [2, 3].
The ocular manifestations of SAC and PAC occur due to mast cell degranulation secondary to allergen exposure in susceptible individuals. In both acute and chronic forms, mast cell degranulation leads to the release of inflammatory mediators and activation of enzymatic cascades that produce pro-inflammatory mediators. Additionally, in chronic allergic conditions, a sustained inflammatory response is observed due to mediators such as eosinophils and cytokines [4]. The main sign and symptom of allergic conjunctivitis are conjunctival hyperemia and ocular itching. The disease pathophysiology seems to be related with type 2 inflammatory pathway [5]. However, neurogenic mechanisms also seem to play a role in allergic inflammation and particularly in ocular itch and pain [6].
It has been shown that effective treatment of allergic conjunctivitis and minimizing exposure to specific allergens can improve the quality of life in patients with ocular allergies [7]. To improve the patient's quality of life, it is important to provide rapid, effective and safe treatment against both seasonal and perennial allergens.
The treatment options in PAC include topical and systemic treatment options. While antihistamine and steroid drops are the main treatment in topical treatment, artificial tears can be used in supportive treatment. However, due to the severe side effects of long-term use of topical steroids such as cataract, glaucoma, and local immunosuppression, immunomodulators such as cyclosporine A, which have fewer side effects, have become one of the topical treatment options [8]. Antihistamines, corticosteroids, and leukotriene antagonists can be included in topical treatment as systemic treatment options in cases whose symptoms are more severe, cannot be controlled with topical treatment, or secondary complications are observed.
Allergen immunotherapy is an important treatment option for patients whose symptoms and signs cannot be controlled despite regular pharmacotherapy [9]. Immunotherapy is based on the idea that the body can be desensitized to certain allergens that stimulate the immune system and trigger allergy symptoms. Hyposensitization created by controlled and regular administration of allergens is one of the effective methods that can be used in the treatment of allergic rhinitis, allergic asthma, and allergic conjunctivitis [9]. Allergen immunoterapy administered through sublingual or subcutaneous route has been shown to provide a sustained effect in the long term up to three years even after discontinuation of the treatment [10].
The use of immunotherapy has increased in recent years due to the side effects caused by the long-term use of topical or systemic agents. Immunotherapy may not only reduce the need for pharmacotherapy but may also reduce the symptoms of allergy seen during attacks and play a preventive role in the emergence of asthma or new allergy types. It has been observed that immunotherapy reduces sensitivity to allergens in the long term and its effect continues after hyposensitization [11, 12]. In this study, we aimed to compare the effects of topical cyclosporine treatment and allergen immunotherapy treatment on allergic signs in patients with perennial allergic conjunctivitis who were sensitized to house dust mite.
Methods
Study design
This retrospective study conducted at Department of Ophthalmology, Gaziosmanpaşa Training and Research Hospital and Division of Allergy and Clinical Immunology, Department of Internal Medicine, Istanbul Faculty of Medicine, Istanbul University. The study adhered to the tenets of the Declaration of Helsinki and received approval from the ethics committee of Gaziosmanpaşa Training and Research Hospital. Informed consent was obtained from all participants.
Subject eligibility criteria
Adult patients who were followed up in the Department of Ophthalmology for more than 24 months with the diagnosis of PAC were referred to the adult Allergy and Clinical Immunology Clinic to be evaluated by skin prick tests (SPTs). SPT with common inhalant allergens including house dust mites (Dermatophagoides pteronyssinus, Dermatophagoides farinea), molds (Aspergillus fumigatus, Alternaria alternata) and pollens [Grasses (Velvet grass, Orchard grass, Rye grass, Timothy grass, Kentucky blue grass, Meadow fescue), Artemisia vulgaris, Chenopodium album, Olea europaea, Urtica dioica, Plantago lanceolata, Betula alba] (Allergopharma®, Reinbek, Germany) were performed as described in detail in previously published studies [13, 14]. Sensitizations in all patients were confirmed by a positive (≥ 3 mm mean wheal response) SPT. PAC patients only having a sensitization to house dust mites were included in the study. Co-sensitization to inhalant allergens other than house dust mites (Dermatophagoides pteronyssinus and/or Dermatophagoides farinea) was an exclusion criteria. The following patients were also excluded from the study: those who (1) had co-existing ocular diseases such as glaucoma, uveitis, ocular infection, ocular surface disease or had a history of a ocular surgery; (2) had uncontrolled asthma, systemic autoimmune disease or active malignancy; (3) reported hypersensitivity to cyclosporine; (4) were pregnant; (5) needed to wear contact lens during the treatment period; (6) used topical or systemic concomitant medications including corticosteroids, NSAIDs, anticholinergics, immunosuppressives; (7) had a history of cyclosporine treatment or immunotherapy for allergic conjunctivitis. The patients were selected from whom were not using the other routine topical therapies for at least 1 month.
Study protocol and clinical assessments
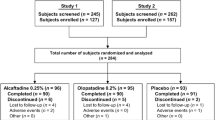
Twenty patients who were found to be sensitive to house dust mites as a result of the skin test divided into two groups. Patients in Group 1 used cyclosporine (Restasis®) only at a dosage of one drop per eye twice daily with an interval of 12 h between drops in both eyes and patients in Group 2 were treated with subcutaneous immunotherapy as in described below for 7 weeks. 1st, 3rd, and 6th month signs’ of the participants were evaluated from medical records. The four signs, papillary reaction, limbal involvement, corneal involvement, and conjunctival hyperemia were graded using the 4-point system (0, none; 1, mild; 2, moderate; and 3 severe) as defined by Uchio et al. [15] and similar to the system used in the study by Dudeja et al. [16]; and the groups were compared using this scoring system. The upper and lower extreme scores were as follows: for upper tarsal papillae, 0 indicates no papillae and 3 indicates predominance of Giant papillae; for limbal activity, 0 indicates no activity and 3 indicates the presence of Horner-Trantas dots; for corneal involvement, 0 indicates intact corneal epithelium and 3 indicates diffuse punctate keratopathy; for conjunctival hyperemia, 0 indicates absence of dilated blood vessels in conjunctiva and 3 indicates generalized dilation of blood vessels.
Subcutaneous immunotherapy (SCIT)
A cluster (accelerated) SCIT protocol lasting 7 weeks was applied to 10 subjects. Three injections were administered once a week during the initial two weeks. The following two weeks, two injections were performed on the treatment days every week. During the subsequent three weeks, only one injection was applied every week. The final dose of immunotherapy reached 1 ml of 5,000 TU at the end of the incremental protocol. The maintenance therapy was administered with 1 ml dose of 5,000 TU monthly as of the incremental protocol. The subjects were observed at least 30 min after every injection due to the risk of allergic reactions under the full emergency resuscitation equipment.
Statistical analysis
In addition to descriptive statistical methods (mean, standard deviation) in the evaluation of the data, the distribution of the variables was examined with the Shapiro–Wilk normality test, the Friedman Test was used for the time comparisons of the non-normally distributed variables and Wilcoxon Signed Ranks test was used for comparison of paired groups. The relations between categorical variables were analyzed using the Chi-square test. The significance level was taken as 95% and the results for p-value, which is equal to and lower than 0.05, were interpreted as statistically significant. For multiple comparisons, Bonferroni correction was also used. All statistical analyses were performed by IBM SPSS Statistics software (Version 27).
Results
Twenty patients who were followed up in the department of ophthalmology for PAC were included in the study. The study was carried out in 2 groups (age- and gender-matched individuals). There was no statistically significant difference between the groups in terms of age, gender (p > 0.05). Table 1 shows the participants’ demographic characteristics.
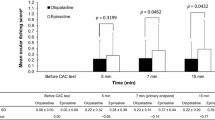
In the study; the initial, 1st, 3rd, and 6th month findings of the relevant parameters (papillary reaction, limbal involvement, corneal involvement, conjunctival hyperemia) of the 2 groups under cyclosporine and immunotherapy treatment were evaluated, and whether there was a difference between repeated measurements of the mentioned parameters for each treatment group was examined (Table 2, Fig. 1). According to the results shown in Table 2, papillary reaction, limbal involvement, and conjunctival hyperemia levels of the patients who received cyclosporine or immunotherapy treatment showed a statistically significant decrease in the later stages of the treatment (p < 0.05).
While there was no difference between repeated measurements in corneal involvement levels in the group receiving immunotherapy treatment (p > 0.05), corneal involvement levels were statistically significantly decreased in patients receiving cyclosporine treatment (p < 0.05).
According to the results in Table 2, the measurements at the end of the treatment periods were compared with the baseline levels for the groups in which a significant difference was found between repeated measurements, and the results are given in Table 3.
In the cyclosporine and immunotherapy groups, the conjunctival hyperemia showed statistically significant differences both in the later stages of the treatment (Table 2) and at the 6th month of the treatment compared to the baseline (Table 3) (p < 0.02).
In both groups, although the limbal involvement decreased in the later stages of the treatment (Table 2), there was no statistically significant difference in Group 1 (Table 3) (p > 0.02) while immunotherapy group showed a statistically significant difference compared to the baseline level at the 6th month (Table 3) (p < 0.02).
Although the corneal involvement levels in the cyclosporin group decreased in the later stages of the treatment (Table 2), there was no statistically significant difference compared to the baseline level at the 6th month (Table 3) (p > 0.02).
In both cyclosporine and immunotherapy groups, the sign of papillary reaction showed a statistically significant decrease in the later stages of treatment (Table 2), but no statistically significant difference was found at the 6th month compared to the baseline level (Table 3) (p > 0.02).
Discussion
This study compared clinical efficacy of two treatment modalities (cyclosporin A and immunotherapy) in perennial allergic conjunctivitis and found almost similar efficacy in terms of sign improvement during 6-month follow-up period. To the best of our knowledge, this study is the first comparing these to treatment types in perennial allergic conjunctivitis.
Large number of studies provided evidence on the use of cyclosporin in the treatment of allergic conjunctivitis cases. A meta-analysis with seven eligible studies examined the benefits of topical cyclosporine in a spectrum of allergic conjunctivitis types [2]. The studies compared cyclosporin treatment with placebo and found significant reductions in sign and symptom scores in association with cyclosporin use beyond 2 weeks [2]. In addition, steroid sparing effect of cyclosporin treatment was evident [2]. Most of the evidence on the effectiveness of cyclosporin treatment comes from severe allergic conjunctivitis cases, mainly vernal keratoconjunctivitis. A recent meta-analysis including 27 studies examined different medical treatments in 1749 vernal keratoconjunctivitis cases. The most frequently used drugs were mast cell stabilizers, cyclosporine, and tacrolimus. Significant symptom/sign improvements were found in association with cyclosporin treatment as well as mast cell stabilizers, tacrolimus, and other less frequently used treatments [17]. A recent randomized controlled trial confirmed the significant benefits of cyclosporine A in pediatric vernal keratoconjunctivitis in terms of both sign/symptom improvement and rescue medication requirement [18]. Similar findings were obtained in an Indian study [19]. Beneficial effects of cyclosporin treatment sign/symptom improvement as well as steroid sparing effects- has been consistently demonstrated in patients with severe keratoconjunctivitis [18,19,20,21,22,23]. Findings of the present study in association with cyclosporin use indicating improvements in most signs are in line with the findings of those previous studies.
The benefits of another immunomodulator agent tacrolimus have also been demonstrated in allergic conjunctivitis. The study by Shoji et al. examined topical tacrolimus in chronic allergic conjunctival disease with and without atopic dermatitis and found equal effectiveness at 6 months of treatment [24]. Cyclosporin and tacrolimus seem to have equal effectiveness in severe keratoconjunctivitis [25], whereas tacrolimus was found to be more effective in cyclosporin resistant cases [26]. In addition, the benefit of combined immunomodulator treatment (cyclosporin plus tacrolimus) has also been demonstrated in patients with severe vernal keratoconjunctivitis [27].
Allergen immunotherapy is considered an effective and safe treatment modality for patients moderate to severe refractory ocular allergic disease and demonstrated sensitization to a specific allergen, which may provide long-term relief [28]. Allergen immunotherapy can be administered via subcutaneous, sublingual, and transcutaneous routes in ocular allergy [28,29,30,31,32,33], although the latter has been rarely reported [29]. In a recent guideline, immunotherapy is considered the only currently available treatment targeting disease pathophysiology in allergic rhino conjunctivitis, thus exhibiting a disease-modifying effect [14]. It is recommended for both seasonal and perennial allergic rhino conjunctivitis for short-term benefit [14]. Both sublingual and subcutaneous routes may be used, usually based on the preference of the patient, with similar efficacy and compliance [30, 31, 33], although sublingual for may be more cost effective [34]. Subcutaneous route has been considered the traditional gold standard administration route for allergen immunotherapy by some authors [28] and this route is the only preferable option in Turkey.
Several recent studies have demonstrated the safety and efficacy of allergen immunotherapy in nasal and ocular allergy. A recent study examined the efficacy and safety of allergen immunotherapy in allergic conjunctivitis [30] in patients with positive skin prick test results. Both subcutaneous and sublingual routes were used in the study, and they were compared. No significant difference was found between the two routes. Significant improvements were found in both groups in terms of symptom relief, reduction in total IgE levels, and wheal diameter of skin prick test. Both treatments were well tolerated with no serious adverse events. A 2019 study examined the efficacy of immunotherapy in perennial form of allergic rhinitis [35]. The study by Tizro et al. used accelerated subcutaneous rush allergen immunotherapy in patients with perennial allergic rhinitis and found significant changes in terms of symptom and quality of life improvement as well as a significant reduction in IgE levels. Findings of the present study are in line with those of previous studies, where significant improvements were found in most sign scores in the immunotherapy group.
Findings of this study have several implications for clinical practice. Effective symptom control has the potential to improve quality of life in allergic conjunctivitis [7]. However, symptom control in perennial allergic conjunctivitis is usually challenging, particularly for treatment refractive cases since effective treatment and avoidance of allergens are necessary all year round. In addition, inadequately managed perennial allergic conjunctivitis can cause dry eye, corneal involvement with chronic inflammatory reaction, and impaired tear film quality [36]. The objectives of the management of perennial allergic conjunctivitis are to prevent ocular surface injury and improve quality of life as well as to provide effective symptom control. Long-term use of topical/systemic polypharmacotherapy has the potential for untoward side effects. For example, long-term use of steroids has the potential to cause cataract and glaucoma. Although cyclosporin A, the other option for the treatment of refractive and/or severe cases, does not usually have severe side effects, its long term use may cause stinging/burning sensation due to the preservative used in the solution; and even molluscum contagiosum, papilloma virus, and herpes virus infections have been reported in association with its long-term use [37]. On the other hand, allergen specific immunotherapy represents an option for treatment refractory cases. Immunotherapy may particularly be useful in perennial allergic conjunctivitis owing to its relatively rapid and sustained effect following hypo-sensitization [11, 12], which has the potential to reduce the need for pharmacotherapy to avoid their side effects as well as to decrease the severity of symptoms and to prevent the development of new sensitizations to aeroallergens. We suggest that allergen immunotherapy can be initiated early in treatment resistant cases to prevent development of asthma, and to improve patient compliance and quality of life. However, immunotherapy should be done under close supervision since it rarely causes life-threatening allergic reactions.
This study has several limitations. The small sample size does limit the generalization of the findings. In addition, a longer follow-up period could have been appropriate to see the clinical effects of SCIT. However, the accelerated SCIT protocol reduced the travel times and hospital visits during the COVID-19 pandemic and provided a faster improvement in allergy symptoms of the patients [38]. In addition, we believe that the absence of symptom evaluation is another limitation. The study was retrospective in nature and a validated instrument was not being used routinely in our institution. In addition, the routine questioning of the symptoms and incorporating them into the study was not possible during the study period since the evaluation of patient history was mostly unsatisfactory during the Covid pandemic. Similarly, post-treatment IgE levels could not be obtained due to the pandemic conditions, although pre-treatment values were available. Changes in IgE levels could contribute to the study and absence may also be regarded as a limitation.
In conclusion, the findings of this study suggest that allergen immunotherapy and cyclosporin A treatment may provide effective sign relief in perennial allergic conjunctivitis. Thus, it may represent a viable treatment option for treatment refractive perennial allergic conjunctivitis cases with positive skin test result for a specific allergen (house dust in the present study), where sign control in the long-term and reduction of the side effects of polypharmacotherapy is particularly important. Large studies with longer follow-up are warranted.
References
Leonardi A, Castegnaro A, Valerio AL, Lazzarini D (2015) Epidemiology of allergic conjunctivitis: clinical appearance and treatment patterns in a population-based study. Curr Opin Allergy Clin Immunol 15:482–488. https://doi.org/10.1097/ACI.0000000000000204
Wan KH, Chen LJ, Rong SS, Pang CP, Young AL (2013) Topical cyclosporine in the treatment of allergic conjunctivitis: a meta-analysis. Ophthalmology 120:2197–2203. https://doi.org/10.1016/j.ophtha.2013.03.044
Offiah I, Calder VL (2009) Immune mechanisms in allergic eye diseases: what is new? Curr Opin Allergy Clin Immunol 9:477–481. https://doi.org/10.1097/ACI.0b013e3283303e2e
Stillerman A, Nachtsheim C, Li W, Albrecht M, Waldman J (2010) Efficacy of a novel air filtration pillow for avoidance of perennial allergens in symptomatic adults. Ann Allergy Asthma Immunol 104:440–449. https://doi.org/10.1016/j.anai.2010.03.006
Bielory L (2022) Immunobiologicals and ocular surface disease. Curr Opin Allergy Clin Immunol 22:314–318. https://doi.org/10.1097/ACI.0000000000000845
Kalangara JP, Vanijcharoenkarn K, Chisolm S, Kuruvilla ME (2022) Neuropathic pain and itch: mechanisms in allergic conjunctivitis. Curr Opin Allergy Clin Immunol 22(5):298–303. https://doi.org/10.1097/ACI.0000000000000843
Leonardi A (1999) Pathophysiology of allergic conjunctivitis. Acta Ophthalmol Scand Suppl. https://doi.org/10.1111/j.1600-0420.1999.tb01167.x
Fukushima A, Yamaguchi T, Ishida W, Fukata K, Liu FT, Ueno H (2006) Cyclosporin a inhibits eosinophilic infiltration into the conjunctiva mediated by type IV allergic reactions. Clin Exp Ophthalmol 34:347–353. https://doi.org/10.1111/j.1442-9071.2006.01221.x
Nolte H, Maloney J (2018) The global development and clinical efficacy of sublingual tablet immunotherapy for allergic diseases. Allergol Int 67:301–308. https://doi.org/10.1016/j.alit.2018.03.008
Penagos M, Durham SR (2022) Long-term efficacy of the sublingual and subcutaneous routes in allergen immunotherapy. Allergy Asthma Proc 43:292–298. https://doi.org/10.2500/aap.2022.43.220026
Huggins JL, Looney RJ (2004) Allergen immunotherapy. Am Fam Physician 70:689–696
Eng PA, Reinhold M, Gnehm HP (2002) Long-term efficacy of preseasonal grass pollen immunotherapy in children. Allergy 57:306–312. https://doi.org/10.1034/j.1398-9995.2002.1o3264.x
Rieker-Schwienbacher J, Nell MJ, Diamant Z, van Ree R, Distler A, Boot JD et al (2013) Open-label parallel dose tolerability study of three subcutaneous immunotherapy regimens in house dust mite allergic patients. Clin Transl Allergy 3:16. https://doi.org/10.1186/2045-7022-3-16
Roberts G, Pfaar O, Akdis CA, Ansotegui IJ, Durham SR, Gerth van Wijk R et al (2018) EAACI guidelines on allergen immunotherapy: allergic rhinoconjunctivitis. Allergy 73:765–798. https://doi.org/10.1111/all.13317
Uchio E, Kimura R, Migita H, Kozawa M, Kadonosono K (2008) Demographic aspects of allergic ocular diseases and evaluation of new criteria for clinical assessment of ocular allergy. Graefes Arch Clin Exp Ophthalmol 246:291–296. https://doi.org/10.1007/s00417-007-0697-z
Dudeja L, Janakiraman A, Dudeja I, Sane K, Babu M (2019) Observer-masked trial comparing efficacy of topical olopatadine (0.1%), bepotastine (1.5%), and alcaftadine (0.25%) in mild to moderate allergic conjunctivitis. Indian J Ophthalmol 67:1400–1404. https://doi.org/10.4103/ijo.IJO_2112_18
Roumeau I, Coutu A, Navel V, Pereira B, Baker JS, Chiambaretta F et al (2021) Efficacy of medical treatments for vernal keratoconjunctivitis: a systematic review and meta-analysis. J Allergy Clin Immunol 148:822–834. https://doi.org/10.1016/j.jaci.2021.03.026
Leonardi A, Doan S, Amrane M, Ismail D, Montero J, Nemeth J et al (2019) A randomized, controlled trial of cyclosporine a cationic emulsion in pediatric vernal keratoconjunctivitis: the vektis study. Ophthalmology 126:671–681. https://doi.org/10.1016/j.ophtha.2018.12.027
Chatterjee A, Bandyopadhyay S, Kumar Bandyopadhyay S (2019) Efficacy, safety and steroid-sparing effect of topical cyclosporine a 0.05% for vernal keratoconjunctivitis in indian children. J Ophthalmic Vis Res 14:412–418. https://doi.org/10.18502/jovr.v14i4.5439
Yucel OE, Ulus ND (2016) Efficacy and safety of topical cyclosporine A 0.05% in vernal keratoconjunctivitis. Singap Med J 57:507–510. https://doi.org/10.11622/smedj.2015161.
Ebihara N, Ohashi Y, Uchio E, Okamoto S, Kumagai N, Shoji J et al (2009) A large prospective observational study of novel cyclosporine 0.1% aqueous ophthalmic solution in the treatment of severe allergic conjunctivitis. J Ocul Pharmacol Ther 25:365–372. https://doi.org/10.1089/jop.2008.0103
Bremond-Gignac D, Doan S, Amrane M, Ismail D, Montero J, Nemeth J et al (2020) Twelve-month results of cyclosporine a cationic emulsion in a randomized study in patients with pediatric vernal keratoconjunctivitis. Am J Ophthalmol 212:116–126. https://doi.org/10.1016/j.ajo.2019.11.020
Subedi K, Sharma B, Shrestha S (2020) Efficacy of topical cyclosporine 0.05% the treatment of vernal keratoconjunctivitis. Nepal J Ophthalmol 12:39–47. https://doi.org/10.3126/nepjoph.v12i1.24489
Shoji J, Ohashi Y, Fukushima A, Miyazaki D, Uchio E, Takamura E et al (2019) Topical tacrolimus for chronic allergic conjunctival disease with and without atopic dermatitis. Curr Eye Res 44:796–805. https://doi.org/10.1080/02713683.2019.1600197
Kumari R, Saha BC, Sinha BP, Mohan N (2017) Tacrolimus versus cyclosporine- comparative evaluation as first line drug in vernal keratoconjuctivitis. Nepal J Ophthalmol 9:128–135. https://doi.org/10.3126/nepjoph.v9i2.19257
Pucci N, Caputo R, di Grande L, de Libero C, Mori F, Barni S et al (2015) Tacrolimus vs. cyclosporine eyedrops in severe cyclosporine-resistant vernal keratoconjunctivitis: a randomized, comparative, double-blind, crossover study. Pediatr Allergy Immunol 26:256–261. https://doi.org/10.1111/pai.12360
Maharana PK, Singhal D, Raj N, Sharma N, Titiyal JS (2021) Role of combined immunomodulator therapy in severe steroid intolerant vernal keratoconjunctivitis. Eye (Lond) 35:979–987. https://doi.org/10.1038/s41433-020-1013-y
Trivedi A, Katelaris C (2021) Presentation, diagnosis, and the role of subcutaneous and sublingual immunotherapy in the management of ocular allergy. Clin Exp Optom 104:334–349. https://doi.org/10.1111/cxo.13129
Agostinis F, Forti S, Di Berardino F (2010) Grass transcutaneous immunotherapy in children with seasonal rhinoconjunctivitis. Allergy 65:410–411. https://doi.org/10.1111/j.1398-9995.2009.02189.x
Sayed KM, Kamel AG, Ali AH (2019) One-year evaluation of clinical and immunological efficacy and safety of sublingual versus subcutaneous allergen immunotherapy in allergic conjunctivitis. Graefes Arch Clin Exp Ophthalmol 257:1989–1996. https://doi.org/10.1007/s00417-019-04389-w
Manzotti G, Riario-Sforza GG, Dimatteo M, Scolari C, Makri E, Incorvaia C (2016) Comparing the compliance to a short schedule of subcutaneous immunotherapy and to sublingual immunotherapy during three years of treatment. Eur Ann Allergy Clin Immunol 48:224–227
Lin CH, Alandijani S, Lockey RF (2016) Subcutaneous versus sublingual immunotherapy. Expert Rev Clin Immunol 12:801–803. https://doi.org/10.1080/1744666X.2016.1196137
Borg M, Lokke A, Hilberg O (2020) Compliance in subcutaneous and sublingual allergen immunotherapy: a nationwide study. Respir Med 170:106039. https://doi.org/10.1016/j.rmed.2020.106039
Di Bona D, Bilancia M, Albanesi M, Caiaffa MF, Macchia L (2020) Cost-effectiveness of grass pollen allergen immunotherapy in adults. Allergy 75:2319–2329. https://doi.org/10.1111/all.14246
Tizro M, Farid Hosseini R, Khoshkhui M, Fouladvand A, Mohammadi M, Sistani S et al (2019) Evaluation of sub cutaneousrush immunotherapy effectiveness in perennial allergic rhinitis after a year from treatment. Iran J Otorhinolaryngol 31:135–139
Miraldi Utz V, Kaufman AR (2014) Allergic eye disease. Pediatr Clin North Am 61:607–620. https://doi.org/10.1016/j.pcl.2014.03.009
Hoy SM (2017) Ciclosporin ophthalmic emulsion 0.1%: a review in severe dry eye disease. Drugs 77:1909–1916. https://doi.org/10.1007/s40265-017-0834-x
Greiwe J, Bernstein JA (2022) Accelerated/rush allergen immunotherapy. Allergy Asthma Proc 43:344–349. https://doi.org/10.2500/aap.2022.43.210108
Acknowledgements
None.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Design of the study (C.U.D., C.T., İ.Ç.T., D.Ç., A.A.A., S.D.); conduct of the study (C.U.D., C.T., İ.Ç.T., D. Ç., A.A.A., S.D.); collection and management of data (C.U.D., C.T., İ.Ç.T., D. Ç., A.A.A , S.D.); analysis and interpretation of data (C.U.D., C.T., İ.Ç.T., DÇ D. Ç., A.A.A , S.D.); preparation of manuscript (C.U.D., C.T., İ.Ç.T., D. Ç., A.A.A , S.D.); review or approval of manuscript (C.U.D., C.T., İ.Ç.T., D. Ç., A.A.A, S.D.).
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest. We have no financial disclosures to report.
Ethical approval
This clinical study is adhered to the tenets of the Declaration of Helsinki and its later amendments and was approved by the Local Ethics Committee of Gaziosmanpaşa Training and Research Hospital, İstanbul, Turkey.
Consent to participate
Informed consent was obtained from all participants included in the study.
Consent for publication
All participants have provided consent for publication.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dogan, C.U., Tuzer, C., Turker, I.C. et al. Topical cyclosporine versus allergen specific immunotherapy in perennial allergic conjunctivitis. Int Ophthalmol 43, 2161–2169 (2023). https://doi.org/10.1007/s10792-022-02612-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-022-02612-y