Abstract
Purpose
To describe tele-ophthalmology consultations for primary-physicians in the IDF during the Covid-19 lockdown.
Methods
Retrospective cross-sectional study. Medical records of tele-ophthalmology consultations from March to June 2020 were reviewed.
Results
The study included 245 cases in which an ophthalmologist was consulted. In 62.0% cell-phone camera photographs were used. The mean age was 21.5 ± 6.4 years. The most common diagnoses were acute-conjunctivitis (8.6%); conjunctival-hyperemia (non-specific diagnosis, 8.2%); scleritis/episcleritis (7.3%); chronic allergic-conjunctivitis (7.3%); chalazion (7.3%) hordeolum (6.5%); acute allergic-conjunctivitis (4.5%). 37.6% of patients received primary physician-based treatment, 24.9% of patients received specialist-based treatment. 13.1% were referred to the ER. The consult prevented ER referral for 39.2% and changed the physician's treatment plan in 70.6% of cases. Foreign-body sensation complaints were more likely treated by a primary-physician (p = 0.015). Cases with suspected foreign-body diagnosis were referred more to the ER (p < 0.001). For most cases of eyelid complaints and diagnoses, primary physician care was sufficient (p < 0.001). Conjunctival complaints and diagnoses received significantly more ophthalmologist-based treatment (p < 0.001). Corneal disorders were significantly referred more to the ER (p = 0.001).
Conclusion
Despite of possible ethical and legal problems and clinical limitations of this instrument, Tele-ophthalmology using objective aids such as smartphone photography can be an efficient tool in aiding the primary-physician, especially for patients with low access to ophthalmologists, with major impact on patient management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During the COVID-19 pandemic, the increasing use of telemedicine has become widespread [1]. Teleophthalmology was initially limited mainly to diabetic retinopathy [2, 3]. With time the use of teleophthalmology became broader, including treatment of urgent cases, treatment of anterior and posterior segment diseases, review for retinopathy of prematurity (ROP), glaucoma monitoring, and monitoring of age-related macular degeneration (AMD) [3,4,5]. In absence of dedicated equipment teleophthalmology was mostly limited to the ocular surface.
Recent studies demonstrated that attaching a simple magnifying lens to a smartphone camera could produce accurate and detailed image of the cornea and the anterior segment of the eye [6,7,8]. Kalra et al. [9] demonstrated that current novel smartphones camera are able to produce high quality images of the ocular surface even without an additional lens. Currently, smartphone-based ophthalmic imaging is a rising and promising technique.
Hogarty et al. studied current applications in the Google play store and Apple app store that are meant for ophthalmology use, such as: visual acuity tests; aid for low vision patients; strabismus tests and aid tools; anterior segment examination and education. Almost all of the applications are not validated, but there is a great potential in this field [10,11,12].
Up do this date there is a limited number of studies combining teleophthalmology with primary physician care. Moreover, most of the existing literature in this discipline describe the use of professional slit-lamp or posterior segment cameras and not, smartphone cameras. Tan et al. [13] conducted a systematic review of 12 studies to test the diagnostic accuracy of real-time teleophthalmology and face-to-face encounter. The consultation was made through images and/or lives video. In 7 studies, teleophthalmology was found to be not inferior to face-to-face encounter. A different research showed that for corneal and anterior segment diseases, the use of simple means of photography (such as a cell-phone camera) provides low sensitivity (about 68% on average) but high specificity (about 95% on average) [14].
Recent studies exhibit that teleophthalmology can be useful in managing ophthalmic conditions, even without dedicated equipment [15,16,17].
Mines et al. [18] described teleophthalmology in the US Army in 2004–2009 and showed that in many cases the decision for the necessity of evacuation changed due to counseling with an ophthalmologist.
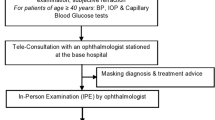
In the IDF, the routine medical treatment for soldiers is based on a primary physician. In relevant cases, the primary physician gives referrals to specialists. It is important to note that according to the IDF clinical guidelines, some medications, such as steroidal eye drops, require a specialist recommendation and cannot be prescribed by a primary care physician.
During the year 2020, the access to specialist in general, and ophthalmologists specifically, reduced due to COVID-19 restrictions. In order to address this shortcoming, diminish the exposure to outer civilian populations and reduce referrals to the ER, there was an increase in the use of telemedicine. These acts were necessary in order to maintain the military’s competence. In most of the cases, consultation was conducted via phone calls, text messages, or a combination of both.
This study aims to describe the cases in which IDF primary physicians used teleophthalmology. This article will test the hypothesis that teleophthalmology can contribute to primary caregivers and increase medical access for ophthalmology care worldwide by smartphone-based teleophthalmology. Currently, there are only a few other studies which demonstrate the potential significance of smartphone-based teleophthalmology on the treatment decision of the primary caregivers. This study aims for assessing this method and its consequences.
Methods
This was a retrospective, cross-sectional study. The computerized database was reviewed for all the cases in which a physician, mostly doctors without specialization, consulted an ophthalmologist between March and June 2020. The patient identity was confidential to the researchers. All the consultations were conducted with the same ophthalmologist. The medical records were reviewed for: patient age and sex; type of army service; mandatory service (combatant, combat assist and non-combatant) and career service; patients' complaints; the ophthalmologist diagnosis; use of photographs from smartphone camera during the consultations; use of objective visual acuity test; the outcome of the consultation (no need for treatment, primary physician-based treatment, specialist-based treatment, referral to ER).
The physicians who consulted were asked via phone call whether the counseling spared them a referral to the emergency room or changed management. In cases where ER referral was decided, they were asked whether the referral was as a result of the counseling, or they would have referred even without the counseling.
The study was approved by the local ethics committee.
Statistical analysis
Data were collected using Microsoft Excel 2016 sheet. Statistical analysis was done using SPSS 25.0 software. Categorical variables were compared by Chi-square test. When the number of expected frequencies was low, the variables were compared using Fisher’s exact test.
Results
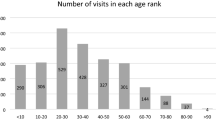
The study population included 245 patients. The male to female ratio was 2.6:1. The mandatory service to career service ratio was 5.6:1. The Demographics of the study population are shown in Table 1. In mandatory service group, 51.9% were combatant, 30.1% were combat support and 18.0% were non-combatant soldiers.
In 152 cases (62.0%) there was a use of cellphone camera photographs. In 27 cases (11.0%), an objective visual acuity test (application or Snellen chart) was used.
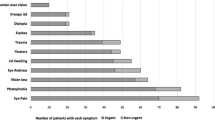
The complaints were classified according to anatomical and clinical groups: conjunctival complaints (72 cases, 29.4%); pain (72 cases, 29.4%); eyelid complaints (59 cases, 24.1%); itching of eye (39 cases, 15.9%); administrative (36 cases, 14.7%) discharge (35 cases, 14.3%); decrease visual acuity (28 cases, 11.4%); foreign body sensation (23 cases, 9.4%); contusion (12 cases, 4.9%); other (21 cases, 8.6%). Table 2 presents the detailed compliant groups.
The diagnoses were classified, similarly according to anatomical and clinical groups: conjunctival disorders (104 cases, 42.4%); eyelid disorders (56 cases, 22.9%); corneal disorders (15 cases, 6.12%); skin disorders (15 cases, 6.1%); suspected foreign body in eye (12 cases, 4.9%); contusion of eye and adnexa (an unspecific diagnosis, 12 cases, 4.9%); visual disturbance disorders (an unspecific diagnosis, 11 cases, 4.5%); other (34 cases, 13.9%). Table 3 presents the detailed groups of diagnoses.
The most common diagnoses were acute conjunctivitis (21 cases, 8.6%); conjunctival hyperemia (unspecified diagnosis, 20 cases, 8.2%); scleritis/episcleritis (18 cases, 7.3%); chronic allergic conjunctivitis (18 cases, 7.3%); chalazion (18 cases, 7.3%) hordeolum and other deep inflammation of eyelid (16 cases, 6.5%); acute atopic (allergic) conjunctivitis (11 cases, 4.5%).
Primary physician-based treatment was given in 92 cases (37.6%). Specialist-based treatment (medications that primary care physicians are not authorized to prescribe in the IDF) was given in 61 cases, (24.9%). For 53 cases (21.6%) no treatment was required. Only 32 cases (13.1%) were referred to the ER, and only 7 cases (2.9%) needed ophthalmologist referral within 1 week.
A telephone survey with treating physicians was conducted in 235 consults out of a total of 245 cases (95.9%). The consult prevented ER referral for 96 patients (39.2%) and changed the physician treatment plan in 173 cases (70.6%). Four patients (0.02%) that would not have been referred to the emergency room prior to the consultation were eventually referred to the ER.
Complaints of a foreign body sensation were significantly more likely, and mostly, treated by primary physician (60.9% vs 35.1%. p-value = 0.015). ER referral was mostly, and significantly more likely to be spared in these cases (66.7% vs 38.3%. p-value = 0.012). Cases that were diagnosed with suspected foreign body were referred more significantly to the ER (50.0% vs 11.2%. p-value < 0.001). Eyelid complaints were significantly more likely, and mostly, treated by primary physician (63.2% vs 29.8%. p-value < 0.001). This correlation was also maintained in the diagnoses groups. Eyelid disorders were significantly more likely, and mostly, treated by primary physician (71.4% vs 27.5%. p-value < 0.001). Conjunctival complaints received significantly more ophthalmologist-based treatment (47.2% vs 15.6%. p-value < 0.001).
Conjunctival disorders diagnoses group were significantly more likely to get specialists-based treatment (42.3% vs 13.5%. p-value < 0.001).
Corneal disorders were significantly referred more to the ER (40.0% vs 11.3%. p-value = 0.001). In 5 out of 6 cases of subconjunctival hemorrhage ER referral was spared (83.3% vs 39.7%. p-value = 0.043).
The study included a total of 36 administrative visits. Administrative consults were mostly, and significantly more likely to get no treatment (66.7% vs 13.9%. p-value < 0.001) and significantly less likely required ambulatory ophthalmologist referral (0% vs 17.4%. p-value = 0.002) or urgent ophthalmologist follow-up (within 1 week) (0% vs 15.1%. p-value = 0.598).
Use of objective visual acuity test was found with significant correlation for ER referral (33.3% vs 10.6%. p-value = 0.001).
Use of smartphone photography was significantly correlated with getting any type of treatment (70.3% vs 32.1%. p-value < 0.001). Furthermore, it was found with significant correlation for getting specialist-based treatment (75.4% vs 57.6%. p-value = 0.015).
Discussion
During the first wave of COVID-19 virus in Israel (March–April 2020), in order to prevent the infection of soldiers from the civilian population, a military directive was issued ordering the need to reduce the number of medical referrals to specialists and ER to a minimum. Ergo, the need for telemedicine in general and teleophthalmology in particular has risen significantly.
This study confirms many presumptions about teleophthalmology. Corneal disorders, foreign body in the eye, and multiple complaints have required more specialist treatment or ER referral. On the other hand, for complaints and diagnoses that does not involve the eyeball itself, such as skin disorders and eyelid disorders (mostly chalazion or hordeolum), primary physician care was sufficient. For administrative consults, the consultation spared referral and granted the patient immediate treatment.
For the foreign body sensation, complaints consultation spared ER referral, and, in most cases, the primary physician could give a sufficient treatment, (60.9% in our study). On the contrary, when the consulting ophthalmologist suspected the presence of a foreign body according to anamnesis or findings in photos, ER referral was needed. A subjective foreign body sensation can be the symptom of many diagnoses such as dryness, various infections, and not necessarily foreign body penetration. Anamnesis or objective findings can help differentiate between the diagnoses. The conclusion is that teleophthalmology can be an aid tool for primary care in cases of foreign body sensation in the eye. In cases with low access to medical services, or in military outlines where medical referral may be a burden, the benefit might be even higher.
In this study, conjunctival disorders were significantly more likely to require a specialist-based treatment. Revising these cases demonstrates that almost all of them were treated with steroidal eye drops. It is important to note that common conjunctival disorders usually do not require steroidal eye drops and are self-limited. In our study steroids have been given mainly for diagnoses of allergic conjunctivitis and episcleritis. It was not administered as a primary treatment for viral conjunctivitis, where the indications for steroid administration are only membranes or sub-epithelial infiltrates. The IDF medical clinical guidelines require specialist recommendation in order to prescribe steroidal eye drops. In civil medicine, a specialist recommendation is not required. A possible reason that contributed to the increase in the use of steroidal drops lies in the need to diminish referrals due to the Covid-19 period directive thus requires treatment with faster response.
We estimate that in civil environment most of the conjunctival disorders could have been treated by primary physician.
Use of smartphone photography was correlated with getting specialist-based treatment. Examination of these cases demonstrates that 50% of them (76 out of 152) were in the conjunctival disorder diagnoses group. Smartphone photography is limited to ocular surface disorders. The fact that specialist recommendation is required for prescribing steroidal drops can explain the positive correlation between using a picture and specialist-based treatment.
This study found that using an objective tool to assess visual acuity increased the need for ER referral. A possible explanation for this lies in the fact that objective findings, such as decreased visual acuity even in the absence of other complaints, can indicate problems in the posterior segment of the eye that require a specialist’s examination. We recommend that primary physicians using teleophthalmology should strive to use as objective means as possible, in order to improve the efficiency of the tool.
The consult prevented a significant amount of ER referrals, and for most cases, changed the physician treatment plan. Furthermore, the medical training in Israel has hardly any exposure to ophthalmology. For the primary physician, additional clinical ophthalmic experience is needed. Due to the lack of experience, the consultation helped the primary physician to get to the correct diagnosis. This data suggests that teleophthalmology was indeed a beneficial tool.
This research has some limitations. First, this is a descriptive study and not interventional. The study did not examine the accuracy of the diagnosis or the effectiveness of the treatment. We tried to follow-up on the cases and find out about the treatment results, unfortunately, we could not find enough data. Most of the cases probably improved, but there was no documentation of it since they did not return to their physician if they improved. We could not extract sufficient data about the patients that were referred to the ER, or about the patients that returned to follow-up with an ophthalmologist. The reason for this is the fact that the army database does not collect data from other health providers, such as civilian ER or civilian ophthalmologists. In some cases, the primary physician documented part of the referral, but it was documented poorly. Second, there is a possibility of recall bias in the study due to phone survey with the treating physicians. Third, there is a very noticeable selection bias in the study population- the treating physicians probably did not consult about less occult cases. Similarly, the treating physicians probably did not consult about grave cases, and probably refer the patient to the ER or an urgent ophthalmologist examination. However, these moderate cases may be the cases that will benefit the most from teleophthalmology. In addition, for some complaints, such as new onset visual disturbances teleophthalmology cannot supply proper consult without dedicated equipment. Adding a magnifying lens for improving the images and thus the efficiency of the consultations, is an inexpensive and practical method to assimilate smartphone based teleophthalmology to common practice.
It is worth noting that telemedicine also raises difficulties: the possibility of violating medical confidentiality; cheap but less professional market formation for remote counseling; there is no legislation on the subject; meeting documentation in text or video; violation of equality (patients without internet access will have no access to this medical service) [19,20,21].
In conclusion, teleophthalmology can contribute to primary caregivers, and increase medical access for ophthalmology care. In our study, the teleconsultation had major impact on sparing ER referrals and affected the treatment for most of the patients. Our study demonstrated for the first time such a significant impact in case management in ophthalmology using telemedicine based. We have yet to find any further studies that have shown such significant effect on the decision making of primary caregivers using teleophthalmology. Despite of possible ethical and legal problems and clinical limitations of this instrument, teleophthalmology as described in this study seems as an efficient tool in aiding primary-care physicians, especially for patients with low access to an ophthalmologist. Using objective tools such as photography and Snellen chart or application to assess the visual acuity may improve the efficacy of this tool.
References
Portnoy J, Waller M, Elliott T (2020) Telemedicine in the Era of COVID-19. J Allergy Clin Immunol Pract 8(5):1489–1491. https://doi.org/10.1016/j.jaip.2020.03.008
Woodward MA, Ple-Plakon P, Blachley T et al (2015) Eye care providers’ attitudes towards tele-ophthalmology. Telemed J E Health 21(4):271–273. https://doi.org/10.1089/tmj.2014.0115
Rathi S, Tsui E, Mehta N, Zahid S, Schuman JS (2017) The Current state of teleophthalmology in the United States. Ophthalmology 124(12):1729–1734. https://doi.org/10.1016/j.ophtha.2017.05.026
Kroenke K (2015) Telemedicine screening for eye disease. JAMA 313(16):1666–1667. https://doi.org/10.1001/jama.2015.107
Quinn GE, Ying GS, Daniel E et al (2014) Validity of a telemedicine system for the evaluation of acute-phase retinopathy of prematurity. JAMA Ophthalmol 132(10):1178–1184. https://doi.org/10.1001/jamaophthalmol.2014.1604
Kaya A (2017) Ophthoselfie: detailed self-imaging of cornea and anterior segment by smartphone. Turk J Ophthalmol 47(3):130–132. https://doi.org/10.4274/tjo.66743
Mohammadpour M, Mohammadpour L, Hassanzad M (2016) Smartphone assisted slit lamp free anterior segment imaging: a novel technique in teleophthalmology. Cont Lens Anterior Eye 39(1):80–81. https://doi.org/10.1016/j.clae.2015.09.005
Lagstein O, Huey D, Guyton DL, Davidson J, Kraus CL (2020) Using IOLs for anterior segment photography in children. J AAPOS 24(4):239–242. https://doi.org/10.1016/j.jaapos.2020.05.004
Kalra G, Ichhpujani P, Thakur S, Singh RB, Sharma U, Kumar S (2021) A pilot study for smartphone photography to assess bleb morphology and vasculature post-trabeculectomy. Int Ophthalmol 41(2):483–490. https://doi.org/10.1007/s10792-020-01598-9
Hogarty DT, Hogarty JP, Hewitt AW (2020) Smartphone use in ophthalmology: what is their place in clinical practice? Surv Ophthalmol 65(2):250–262. https://doi.org/10.1016/j.survophthal.2019.09.001
Yang M, Lo ACY, Lam WC (2020) Smart phone apps every ophthalmologist should know about. Int J Ophthalmol 13(8):1329–1333. https://doi.org/10.18240/ijo.2020.08.21
Samanta A, Mauntana S, Barsi Z, Yarlagadda B, Nelson PC (2020) Is your vision blurry? A systematic review of home-based visual acuity for telemedicine. J Telemed Telecare. https://doi.org/10.1177/1357633X20970398
Tan IJ, Dobson LP, Bartnik S, Muir J, Turner AW (2017) Real-time teleophthalmology versus face-to-face consultation: a systematic review. J Telemed Telecare 23(7):629–638. https://doi.org/10.1177/1357633X16660640
Woodward MA, Musch DC, Hood CT et al (2017) Teleophthalmic approach for detection of corneal diseases: accuracy and reliability. Cornea 36(10):1159–1165. https://doi.org/10.1097/ICO.0000000000001294
Gensheimer WG, Miller KE, Stowe J, Little J, Legault GL (2020) Military teleophthalmology in Afghanistan using mobile phone application. JAMA Ophthalmol 138(10):1053–1060. https://doi.org/10.1001/jamaophthalmol.2020.3090
Bourdon H, Jaillant R, Ballino A et al (2020) Teleconsultation in primary ophthalmic emergencies during the COVID-19 lockdown in Paris: experience with 500 patients in March and April 2020. J Fr Ophtalmol 43(7):577–585. https://doi.org/10.1016/j.jfo.2020.05.005
Sommer AC, Blumenthal EZ (2020) Telemedicine in ophthalmology in view of the emerging COVID-19 outbreak. Graefes Arch Clin Exp Ophthalmol 258(11):2341–2352. https://doi.org/10.1007/s00417-020-04879-2
Mines MJ, Bower KS, Lappan CM, Mazzoli RA, Poropatich RK (2011) The United States army ocular teleconsultation program 2004 through 2009. Am J Ophthalmol 152(1):126–132. https://doi.org/10.1016/j.ajo.2011.01.028
Newton MJ (2014) The promise of telemedicine. Surv Ophthalmol 59(5):559–567. https://doi.org/10.1016/j.survophthal.2014.02.003
Morse AR (2014) Telemedicine in ophthalmology: promise and pitfalls. Ophthalmology 121(4):809–811. https://doi.org/10.1016/j.ophtha.2013.10.033
Shahbaz R, Salducci M (2021) Law and order of modern ophthalmology: teleophthalmology, smartphones legal and ethics. Eur J Ophthalmol 31(1):13–21. https://doi.org/10.1177/1120672120934405
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest, or non-financial interest in the subject matter or materials discussed in this manuscript.
Ethical Approval
This retrospective chart review study involving human participants was in accordance with the ethical standards of the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The local Ethics Committee of IDF approved this study.
Informed Consent
For this type of study formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Koriat, Y., Saveliev, N., Koriat, A. et al. Tele-ophthalmology as an aid tool for primary care physicians in the IDF, during the Covid-19 lockdown. Int Ophthalmol 42, 2741–2748 (2022). https://doi.org/10.1007/s10792-022-02263-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-022-02263-z