Abstract
Purpose
To use optic coherence tomography (OCT) to evaluate idiopathic intracranial hypertension (IIH) patients with subclinical segmental optic atrophy despite being under apparently effective treatment.
Methods
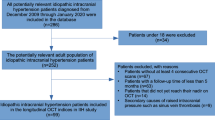
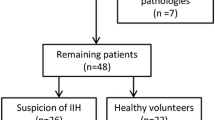
IIH patients underwent an OCT examination including the peripapillary retina never fiber layer (RNFL) thickness, ganglion cell complex (GCC) thickness, focal loss volume (FLV) and global loss volume (GLV) of the GCC, and total macular thickness measurements at presentation and at 3, 6, 9, and 12 months after the diagnosis. The obtained data were compared with healthy subjects. Subjects with and without subclinical segmental atrophy at the 12th month were compared according to the demographics, clinical findings, and the OCT parameters recorded at the beginning of the disease.
Results
Both eyes of 56 patients with papilledema due to IIH and 50 age- and sex-matched control subjects were included in this prospective case–control study. Regression of papilledema with regional axon loss on the peripapillary RNFL thickness map was found in 37 (33%) eyes in the IIH group. IIH patients with segmental atrophy had the following characteristics when compared to those without segmental atrophy at the beginning of the disease: higher CSF opening pressure, higher grade of papilledema, thicker mean peripapillary RNFL thickness, thinner GCC layer, greater FLV and GLV loss, and severe visual field loss.
Conclusions
Axonal loss occurred in the patients despite apparent treatment. It would be appropriate to follow-up with aggressive medical treatment those patients who present with the following characteristics: higher CSF opening pressure, higher grade of papilledema, thicker mean peripapillary RNFL thickness, and thinner GCC.
Similar content being viewed by others
References
De Simone R, Ranieri A, Montella S, Friedman DI, Liu GT, Digre KE (2014) Revised diagnostic criteria for the pseudotumor cerebri syndrome in adults and children. Neurology 18(11):1011–1012
Fraser C, Plant GT (2011) The syndrome of pseudotumor cerebri and idiopathic intracranial hypertension. Curr Opin Neurol 24(1):12–17
Julayanont P, Karukote A, Ruthirago D, Panikkath D, Panikkath R (2016) Idiopathic intracranial hypertension: ongoing clinical challenges and future prospects. J Pain Res 9:87–99
Friedman DI (2014) The pseudotumor cerebri syndrome. Neurol Clin 32(2):363–396
Thurtell MJ, Bruce BB, Newman NJ, Biousse V (2010) An update on idiopathic intracranial hypertension. Rev Neurol Dis 7(2–3):56–68
Chan JW (2017) Current concepts and strategies in the diagnosis and management of idiopathic intracranial hypertension in adults. J Neurol 264(8):1622–1633
Rowe FJ (2011) Assessment of visual function in idiopathic intracranial hypertension. Br J Neurosurg 25(1):45–54
Rowe FJ, Sarkies NJ (1998) Assessment of visual function in idiopathic intracranial hypertension: a prospective study. Eye (Lond) 12(Pt 1):111–118
Rebolleda G, Diez-Alvarez L, Casado A, de Dompablo E, González-López JJ, Muñoz-Negrete FJ (2015) OCT: new perspectives in neuro-ophthalmology. Saudi J Ophthalmol 29(1):9–25
Auinger P, Durbin M, Feldon S et al (2015) Optical coherence tomography substudy committee; nordic idiopathic intracranial hypertension study group papilledema outcomes from the optical coherence tomography substudy of the idiopathic intracranial hypertension treatment trial. Ophthalmology 122(9):1939-e2–1945
Yri MH, Wegener M, Sander B, Jensen R (2012) Idiopathic intracranial hypertension is not benign: a long-term outcome study. J Neurol 259(5):886–894
Laemmer R, Heckmann JG, Mardin CY, Schwab S, Laemmer AB (2010) Detection of nerve fiber atrophy in apparently effectively treated papilledema in idiopathic intracranial hypertension. Graefes Arch Clin Exp Ophthalmol 248(12):1787–1793
Rebolleda G, Muñoz-Negrete FJ (2009) Follow-up of mild papilledema in idiopathic intracranial hypertension with optical coherence tomography. Invest Ophthalmol Vis Sci 50(11):5197–5200
Eren Y, Kabatas N, Guven H, Comoglu S, Gurdal C (2019) Evaluation of optic nerve head changes with optic coherence tomography in patients with idiopathic intracranial hypertension. Acta Neurol Belg 119(3):351–357
Skau M, Sander B, Milea D, Jensen R (2011) Disease activity in idiopathic intracranial hypertension: a 3-month follow-up study. J Neurol 258(2):277–283
Headache Classification Committee of the International Headache Society (IHS) (2018) The international classification of headache disorders 3th edn. Cephalgia, 38 (1):1–211
Heijl A, Patella VM, Bengstsson B (2012) The field analyzer primer: effective perimetry, 4th edn. Carl Zeiss Meditec, Dublin
Cameron JR, Albrecht P, Cruz-Herranz A, Lagreze WA, Schuman JS, Villoslada P, Calabresi P, Balcer L, Petzold A, Green AJ, Paul F, Brandt AU, Albrecht P (2016) IMSVISUAL consortium The APOSTEL recommendations for reporting quantitative optical coherence tomography studies. Neurology 86(24):2303–9
Garas A, Vargha P, Holló G (2011) Diagnostic accuracy of nerve fiber layer, macular thickness and optic disc measurements made with the RTVue-100 optical coherence tomography to detect glaucoma. Eye 25(1):57–65
Rao HL, Babu JG, Addepalli UK, Senthil S, Garudadri CS (2012) Retinal nerve fiber layer and macular inner retina measurements by spectral domain optical coherence tomography in Indian eyes with early glaucoma. Eye 26(1):133–139
Tan Ou, Chopra V, Tzu-Hui LuA, Schuman JS, Ishikawa H, Wollstein G, Varma R, Huang D (2009) Detection of macular ganglion cell loss in glaucoma by Fourier-domain optical coherence tomography. Ophthalmology 116(12):2305–2314
Zhang X, Iverson SM, Tan O, Huang D (2015) Effect of signal intensity on measurement of ganglion cell complex and retinal nerve fiber layer scans in Fourier-domain optical coherence tomography. Transl Vis Sci Technol 4(5):7–17
Jensen RH, Radojicic A, Yri H (2016) The diagnosis and management of idiopathic intracranial hypertension and the associated headache. Ther Adv Neurol Disord 9(4):317–326
Wall M, George D (1991) Idiopathic intracranial hypertension. A prospective study of 50 patients. Brain 114:155–180
Quigley HA, Addicks EM, Green WR (1982) Optic nerve damage in human glaucoma III Quantitative correlation of nerve fiber loss and visual field defect in glaucoma, ischemic neuropathy, papilledema, and toxic neuropathy. Arch Ophthalmol 100(1):135–146
Hedges TR III, Legge RH, Peli E, Yardley CJ (1995) Retinal nerve fiber layer changes and visual field loss in idiopathic intracranial hypertension. Ophthalmology 102(8):1242–1247
OCT Sub-Study Committee for NORDIC Idiopathic Intracranial Hypertension Study Group, Auinger P, Durbin M, Feldon S, Garvin M, Kardon R, Keltner J, Kupersmith M, Sibony P, Plumb K, Wang J-K, Werner JS (2014) Baseline OCT measurements in the idiopathic Intracranial hypertension treatment trial, part I: quality control, comparisons, and variability. Invest Ophthalmol Vis Sci 55(12):8180–8188
Naumann GOH, Apple DJ (1986) Pathology of the eye. Springer, New York, pp 1–31
Yohannan J, Wang J, Brown J, Chauhan BC, Boland MV, Friedman DS, Ramulu PY (2017) Evidence-based criteria for assessment of visual field reliability. Ophthalmology 124(11):1612–1620
Waisbourd M, Leibovitch I, Goldenberg D, Kesler A (2011) OCT assessment of morphological changes of the optic nerve head and macula in idiopathic intracranial hypertension. Clin Neurol Neurosurg 113(10):839–843
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by [Naciye KABATAS, Yasemin EREN, Pinar NALCACIOGLU, Sinan CALISKAN, Tolga BİCER]. The first draft of the manuscript was written by [Naciye KABATAS, Yasemin EREN, Pinar NALCACIOGLU] and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent to Publish
Informed consent was obtained from all individual participants included in the study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the Local Ethics Committee of Diskapi Yildirim Beyazit Research and Education Hospital. Decision number: 76/09–25.11.2019.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kabatas, N., Eren, Y., Nalcacioglu, P. et al. Management of the regression of papilledema with regional axon loss in idiopathic intracranial hypertension patients. Int Ophthalmol 41, 1467–1477 (2021). https://doi.org/10.1007/s10792-021-01711-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-021-01711-6