Abstract
To separate the effects of physicians’ characteristics on the perceived productivity of EMRs from the effects of limitations on usability inherent in EMR design, a multivariate regression model is used to estimate the factors influencing physicians’ rankings of five attributes of their EMRs, namely; ease of use and reliability; the EMRs effect on physician and staff productivity and the EMRs performance vs. vendor’s promises. We divide the factors influencing the rankings into three groups: physician characteristics, EMR characteristics and practice characteristics (type of practice, size, and location). The data are from approximately 1800 practicing physicians in Arizona. Physician’s characteristics influence perceived ease of use and physicians’ productivity, but not staff productivity, reliability or vendors’ promised performance. Practice type and EMR characteristics affect perceived productivity, reliability and performance versus vendors’ promises. Vendor-specific effects are highly correlated across all five attributes and are always jointly significant. EMR characteristics are the most significant influence on physicians’ perceptions of the EMRs effect on their productivity and that of their staff. Physicians’ characteristics (particularly age) have a small but significant influence on perceived productivity.
Similar content being viewed by others
References
Babbott, S., Manwell, L. B., Brown, R., Montague, E., Williams, E., Schwartz, M., et al. (2014). Electronic medical records and physician stress in primary care: Results from the MEMO Study. Journal of the American Medical Informatics Association, 21(E2), e100–e106. doi:10.1136/amiajnl-2013-001875.
Centers for Disease Control and Prevention. NAMCS Participants Page. Available at: http://www.cdc.gov/nchs/ahcd/namcs_participant.htm. Accessed December 10, 2015.
Chaudhry, B., Wang, J., Wu, S., Maglione, M., Mojica, W., Roth, E., et al. (2006). Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Annals of Internal Medicine, 144, 742–752.
Freudenheim, M. (October 9, 2012). The ups and downs of electronic medical records The New York Times: D4
Gagnon, M.-P., Ghandour, E. K., Talla, P. K., et al. (2014). Electronic health record acceptance by physicians: Testing an integrated theoretical model. Journal of Biomedical Informatics, 48, 17–27.
Heisey-Grove, D., Danehy, L. N., Consolazio, M., Lynch, K., & Mostashari, F. (2014). A national study of challenges to electronic health record adoptions and meaningful use. Medical Care, 52(2), 144–148.
Hsiao, C. J., & Hing, E. (2014). Use and characteristics of electronic health record systems among office-based physician practices: United States, 2001–2013. National Center for Health Statistics Data Brief, 143, 1–8.
Ilie, V., Van Slyke, C., Parikh, M. A., & Courtney, J. F. (2009). Paper versus electronic medical records: The effects of access on physicians’ decisions to use complex information technologies*. Decision Sciences, 40(2), 213–241.
Jamoom, E., Beatty, P., Bercovitz, A., Woodwell, D., Palso, K., & Rechtsteiner, E. (2012). Physician adoption of electronic health record systems: United States, 2011. NCHS data brief, no 98, Hyattsville. MD: National Center for Health Statistics.
Jha, A. K., DesRoches, C. M., Campbell, E. G., Donelan, K., Sowmya, R. R., Ferris, T. G., et al. (2009). Use of electronic health records in U.S. hospitals. New England Journal of Medicine, 361, 421–422.
Johnson, W. G., Harootunian, G., & Sama T. L. (September 2013). Physicians’ use, exchange, and evaluation of electronic medical records. Center for Health Information & Research (Prepared for AHCCCS and the Arizona Strategic Enterprise Technology (ASET) Office). http://chir.asu.edu/home.
Jones, S. S., Heaton, P. S., Rudin, R. S., & Schneider, E. C. (2012). Unraveling the IT productivity paradox–lessons for health care. New England Journal of Medicine, 366(24), 2243–2245. doi:10.1056/NEJMp1204980.
Kellermann, A. L., & Jones, S. S. (2013). What it will take to achieve the as-yet-unfulfilled promises of health information technology. Health Affairs, 32(1), 63–68. doi:10.1377/hlthaff.2012.0693.
Lau, F., Price, M., Boyd, J., Partridge, C., Bell, H., & Raworth, R. (2012). Impact of electronic medical record on physician practice in office settings: a systematic review. BMC Medical Informatics and Decision Making, 12(1), 10. doi:10.1186/1472-6947-12-10.
Meinert, D. B., & Peterson, D. (2009). Perceived importance of EMR functions and physician characteristics. Journal of Systems and Information, 11, 57–70.
Niederle, M., Roth, A. E. T., &&Somnez, T. (2008). Matching. In S. N. Durlauf & L. E. Blume (Eds.), The new palgrave dictionary of economics (2nd ed.). New Haven: Palgrave MacMillan.
Nov, O., & Schecter, W. (2012). Dispositional resistance to change and hospital physicians’ use of electronic medical records: A multi-dimensional perspective. Journal of the American Society for Information Science and Technology, 63(4), 648–656.
Ratwani, R. M., Fairbanks, R. J., Hettinger, A. Z., & Benda, N. C. (2015). Electronic health record usability: Analysis of the user-centered design processes of eleven electronic health record vendors. Journal of the American Medical Informatics Association, 22, 1179–1182.
Skolnik, N. S. (Ed.). (2011). Electronic medical records: A practical guide for primary care. New York: Humana Press.
Terry, K. (March 2012). Doctors can’t tear themselves away from paper records. Information Week.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Author Contributors
RJB and WGJ contributed to the conception, design and drafting of this research. WGB supervised the acquisition of the data. RJB completed the data analysis. Both authors approved the final version of this paper.
Conflict of Interests
None.
Funding
Data Support from the Center for Health Information Research at Arizona State University is greatly appreciated, as are programming help from Gevork Harootunian.
Appendix
Appendix
Appendix with ordered logistic regression results for “Rating the Digital Help: Electronic Medical Records, Software Providers, and Physicians”
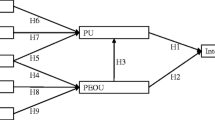
An ordered logit regression accounts for the interval nature of outcomes (namely, the dependent variable only takes the integer values 1, 2, 3, 4, or 5) by calculating the likelihood that individual i’s index function (\(X_i \beta )\) falls in ordered predictive buckets, where \(\beta \) are the empirically calculated weights for the physician-EMR-practice variable vector \(X_i \). The constructed buckets are one of five intervals of a logit distribution function, the transition to each bucket having a distinct intercept value (\(\alpha _i )\). Hence the likelihood to be maximized, by choosing the slope coefficients (the \(\beta )\) for data falling in one of j intervals, \(L\left( {\alpha _j +X_i \beta } \right) -L(\alpha _{j-1} +X_i \beta )\) (with \(z_{i,j} \) is an indicator function equal to one when the ith observation falls in the jth interval), is
A positive coefficient in Table 5 represents the effect of a unit increase in the respective variable on the log-odds ratio of moving up one more productivity index value (Tables 6, 7).
Rights and permissions
About this article
Cite this article
Butler, R.J., Johnson, W.G. Rating the digital help: electronic medical records, software providers, and physicians. Int J Health Econ Manag. 16, 269–283 (2016). https://doi.org/10.1007/s10754-016-9190-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10754-016-9190-8