Abstract
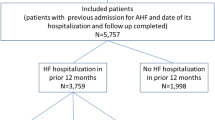
Clinical trials for acute heart failure syndromes (AHFS) have traditionally enrolled patients well after emergency department (ED) presentation. We hypothesized a large proportion of patients would undergo changes in clinical profiles during the first 24 h of hospitalization, and these changes would be associated with adverse events. We evaluated a prospective cohort of patients with clinical data available at ED presentation and 12–24 h after ED treatment for AHFS. Patients were categorized into distinct clinical profiles at these time points based on (1) systolic blood pressure: a—hypertensive (>160 mmHg); b—normotensive (100–159 mmHg); or c—hypotensive (<100 mmHg); (2) moderate-to-severe renal dysfunction (GFR ≤ 60 ml/min/1.73 m2); and (3) presence of troponin positivity. A composite outcome of 30-day cardiovascular events was determined by phone follow-up. In the 370 patients still hospitalized with data available at the 12–24 h time point, 196 (53.0%) had changed their clinical profiles, with 117 (59.7%) improving and 79 (40.3%) worsening. The composite 30-day event rate was 16.9%. Patients whose clinical profile started and stayed abnormal had a significantly greater proportion of events than those who started and stayed normal (26.1% vs. 11.3%; P = 0.03). Patients with abnormal clinical profiles at presentation that remain abnormal throughout the first 12–24 h of hospitalization are at increased risk of 30-day adverse events. Future clinical trials may need to consider targeting these patients, as they may be the most likely to benefit from experimental therapy.
Similar content being viewed by others
References
VMAC Investigators (2002) Intravenous nesiritide vs. nitroglycerin for treatment of decompensated congestive heart failure: a randomized controlled trial. JAMA 287:1531–1540
Collins SP, Hinckley WR, Storrow AB (2005) Critical review and recommendations for nesiritide use in the emergency department. J Emerg Med 29:317–329
Sackner-Bernstein JD, Kowalski M, Fox M, Aaronson K (2005) Short-term risk of death after treatment with nesiritide for decompensated heart failure: a pooled analysis of randomized controlled trials. JAMA 293:1900–1905
O’Connor CM, Starling RC, Hernandez AF, Armstrong PW, Dickstein K, Hasselblad V, Heizer GM, Komajda M, Massie BM, McMurray JJ, Nieminen MS, Reist CJ, Rouleau JL, Swedberg K, Adams KF Jr, Anker SD, Atar D, Battler A, Botero R, Bohidar NR, Butler J, Clausell N, Corbalan R, Costanzo MR, Dahlstrom U, Deckelbaum LI, Diaz R, Dunlap ME, Ezekowitz JA, Feldman D, Felker GM, Fonarow GC, Gennevois D, Gottlieb SS, Hill JA, Hollander JE, Howlett JG, Hudson MP, Kociol RD, Krum H, Laucevicius A, Levy WC, Mendez GF, Metra M, Mittal S, Oh BH, Pereira NL, Ponikowski P, Wilson WH, Tanomsup S, Teerlink JR, Triposkiadis F, Troughton RW, Voors AA, Whellan DJ, Zannad F, Califf RM (2011) Effect of nesiritide in patients with acute decompensated heart failure. N Engl J Med 365:32–43
Mebazaa A, Pang PS, Tavares M, Collins SP, Storrow AB, Laribi S, Andre S, Mark Courtney D, Hasa J, Spinar J, Masip J, Frank Peacock W, Sliwa K, Gayat E, Filippatos G, Cleland JG, Gheorghiade M (2010) The impact of early standard therapy on dyspnoea in patients with acute heart failure: the urgent-dyspnoea study. Eur Heart J 31:832–841
Hasselblad V, Gattis Stough W, Shah MR, Lokhnygina Y, O’Connor CM, Califf RM, Adams KF Jr (2007) Relation between dose of loop diuretics and outcomes in a heart failure population: results of the escape trial. Eur J Heart Fail 9:1064–1069
Gottlieb SS, Abraham W, Butler J, Forman DE, Loh E, Massie BM, O’Connor CM, Rich MW, Stevenson LW, Young J, Krumholz HM (2002) The prognostic importance of different definitions of worsening renal function in congestive heart failure. J Card Fail 8:136–141
Weintraub NL, Collins SP, Pang PS, Levy PD, Anderson AS, Arslanian-Engoren C, Gibler WB, McCord JK, Parshall MB, Francis GS, Gheorghiade M (2010) Acute heart failure syndromes: emergency department presentation, treatment, and disposition: current approaches and future aims: a scientific statement from the american heart association. Circulation 122:1975–1996
Collins SP, Levy PD, Lindsell CJ, Pang PS, Storrow AB, Miller CD, Naftilan AJ, Thohan V, Abraham WT, Hiestand B, Filippatos G, Diercks DB, Hollander J, Nowak R, Peacock WF, Gheorghiade M (2009) The rationale for an acute heart failure syndromes clinical trials network. J Card Fail 15:467–474
Storrow AB, Collins S, Lindsell CJ, Disalvo T, Han J, Weintraub NL (2007) Improving heart failure risk stratification in the ed: Stratify 1r01hl088459-01; treatment endpoints in acute decompensated heart failure 1k23hl085387-01a2
Teerlink JR, Metra M, Felker GM, Ponikowski P, Voors AA, Weatherley BD, Marmor A, Katz A, Grzybowski J, Unemori E, Teichman SL, Cotter G (2009) Relaxin for the treatment of patients with acute heart failure (pre-relax-ahf): a multicentre, randomised, placebo-controlled, parallel-group, dose-finding phase iib study. Lancet 373:1429–1439
Levy P, Compton S, Welch R, Delgado G, Jennett A, Penugonda N, Dunne R, Zalenski R (2007) Treatment of severe decompensated heart failure with high-dose intravenous nitroglycerin: a feasibility and outcome analysis. Ann Emerg Med 50:144–152
Peacock WFt, De Marco T, Fonarow GC, Diercks D, Wynne J, Apple FS, Wu AH (2008) Cardiac troponin and outcome in acute heart failure. N Engl J Med 358:2117–2126
Voors AA, Davison BA, Felker GM, Ponikowski P, Unemori E, Cotter G, Teerlink JR, Greenberg BH, Filippatos G, Teichman SL, Metra M (2011) Early drop in systolic blood pressure and worsening renal function in acute heart failure: renal results of pre-RELAX-AHF. Eur J Heart Fail 13:961–967
Aronson D, Burger AJ (2010) The relationship between transient and persistent worsening renal function and mortality in patients with acute decompensated heart failure. J Card Fail 16:541–547
Gheorghiade M, Abraham WT, Albert NM, Greenberg BH, O’Connor CM, She L, Stough WG, Yancy CW, Young JB, Fonarow GC (2006) Systolic blood pressure at admission, clinical characteristics, and outcomes in patients hospitalized with acute heart failure. JAMA 296:2217–2226
Fonarow GC, Adams KF Jr, Abraham WT, Yancy CW, Boscardin WJ (2005) Risk stratification for in-hospital mortality in acutely decompensated heart failure: classification and regression tree analysis. JAMA 293:572–580
Apple FS (2009) A new season for cardiac troponin assays: It’s time to keep a scorecard. Clin Chem 55:1303–1306
Morrow DA, Cannon CP, Jesse RL, Newby LK, Ravkilde J, Storrow AB, Wu AH, Christenson RH (2007) National academy of clinical biochemistry laboratory medicine practice guidelines: clinical characteristics and utilization of biochemical markers in acute coronary syndromes. Circulation 115:E 356–E 375
Morrow DA, de Lemos JA (2007) Benchmarks for the assessment of novel cardiovascular biomarkers. Circulation 115:949–952
Gheorghiade M, Braunwald E (2011) A proposed model for initial assessment and management of acute heart failure syndromes. JAMA 305:1702–1703
Collins SP, Pang PS, Lindsell CJ, Kyriacou DN, Storrow AB, Hollander JE, Kirk JD, Miller CD, Nowak R, Peacock WF, Tavares M, Mebazaa A, Gheorghiade M.(2010) International variations in the clinical, diagnostic, and treatment characteristics of emergency department patients with acute heart failure syndromes. Eur J Heart Fail 12: 1253–1260
Berry DA (2006) Bayesian clinical trials. Nat Rev Drug Discov 5:27–36
Potluri S, Ventura HO, Mulumudi M, Mehra MR (2004) Cardiac troponin levels in heart failure. Cardiol Rev 12:21–25
WFt Peacock, De Marco T, Fonarow GC, Diercks D, Wynne J, Apple FS, Wu AH, Investigators A, WFt Peacock, De Marco T, Fonarow GC, Diercks D, Wynne J, Apple FS, Wu AHB (2008) Cardiac troponin and outcome in acute heart failure. N Engl J Med 358:2117–2126
Acknowledgments
The authors would like to acknowledge Lyndi Goette, MBA, for her help in preparation of the manuscript. This work was supported in part by National Heart, Lung and Blood Institute grant K23HL085387 and an institutional Clinical and Translational Science Award NIH/NCRR Grant Number 1UL1RR026314-01.
Conflict of interest
Sean Collins: Consultant: Abbott Point of Care, Bayer, The Medicines Company, Trevena, Novartis;Grant Support: NIH/NHLBI, Abbott Point of Care, BG Medicine. Alan Storrow: Current Grant Support: Abbott Diagnostics, NIH/NHLBI (R01HL088459-02). NIH/NHLBI (K23HL085387-01A2), NIH/NHLBI (K12HL1090-01), Centers for Disease Control, Corthera, Roche Diagnostics, Abbott Diagnostics, Thermo Fisher. Current Consultant: Roche Diagnostics. Greg Fermann: Grant support: Dyax, Corthera, The Medicines Company. Advisory Board: Quest Diagnostics/Hemocue, Daiichi Sankyo. Frank Peacock: Research Grants (>$10,000) Abbott, Alere, BAS, Brahms, EKR, Nanosphere, The Medicine’s Company; Consultant (<$10,000) Abbott, Alere, Beckman Coulter, Electrocore, The Medicine’s Company; Speaker’s Bureau (<$10,000) Abbott, Alere; Ownership Interest (<$10,000) Comprehensive Research Associates LLC, Vital Sensors, Emergencies in Medicine LLC. Peter Pang: Dr. Pang has been a consultant for Bayer, J&J, Medtronic, Novartis, Otsuka, SigmaTau, and Trevena and a member of the DSMB for J&J and the Medicines Company. He has received research support from Abbott. Phil Levy: Consultant: The Medicines Company (Data Safety Monitoring Board), Corthera, Inc., Bayer Schering Pharma AG, EKR Therapeutics, Trevena, Inc Research support/grants: The Cleveland Clinic Foundation, Nile Therapeutics, Corthera, Inc., Bayer Schering Pharma AG Speakers Bureau: The Society of Chest Pain Centers Chris Lindsell: Grant support: Abbott Point of Care. Mihai Gheorghiade: Consultant (modest): Abbott Labs, Astellas, Astra Zeneca, Bayer Schering Pharma AG, CorThera, Inc., Cytokinetics, Inc., DebioPharm S.A., Errekappa Terapeutici (Milan, Italy), Glaxo Smith Kline, Johnson & Johnson, Medtronic, Merck, Novartis Pharma AG, Otsuka Pharmaceuticals, Pericor Therapeutics, Protein Design Laboratories, Sanofi Aventis, Sigma Tau, Solvay Pharmaceuticals. Dr. Gheorghiade receives $10,000 or more as a consultant from the following companies: Bayer Schering Pharma AG, DebioPharm S.A., Medtronic, Novartis Pharma AG, Otsuka Pharmaceuticals, Sigma Tau, Solvay Pharmaceuticals, DebioPharm S.A., Pericor Therapeutics. Drs. Doug Sawyer and Neal Weintraub have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Collins, S.P., Lindsell, C.J., Storrow, A.B. et al. Early changes in clinical characteristics after emergency department therapy for acute heart failure syndromes: identifying patients who do not respond to standard therapy. Heart Fail Rev 17, 387–394 (2012). https://doi.org/10.1007/s10741-011-9294-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-011-9294-7